What is lens-induced uveitis?
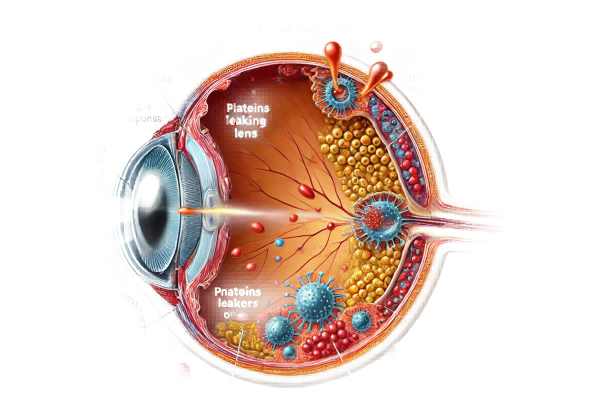
Lens-induced uveitis is an ocular condition marked by inflammation of the uvea, the eye’s middle layer, caused by lens-related issues. This condition can occur as a result of trauma, cataract formation, or lens dislocation, causing lens proteins to leak into the eye. These proteins elicit an immune response, which causes inflammation. Lens-induced uveitis can cause significant discomfort and vision impairment, and if not treated, can progress to complications such as glaucoma or cataract.
Detailed Insights into Lens-Induced Uveitis
Lens-induced uveitis, also known as phacoantigenic uveitis, is a type of uveitis that results from an immune response to lens proteins. Because of the variety of symptoms and potential complications, this condition can be difficult to diagnose and manage.
Pathophysiology
The lens of the eye is usually enclosed in a capsule that protects its proteins from the immune system. However, if the lens capsule is damaged due to trauma, surgery, or degenerative changes, lens proteins can leak into the anterior chamber. The immune system recognizes these proteins as foreign antigens and responds with inflammation.
- Trauma: Physical injury to the eye can rupture the lens capsule, resulting in the release of lens proteins.
- Surgery: Complications from cataract surgery or other intraocular procedures can cause lens capsule disruption.
- Degenerative Changes: Conditions such as hypermature cataracts can cause the lens capsule to weaken and leak proteins.
Clinical Presentation
Lens-induced uveitis can be acute or chronic, with symptoms ranging from mild to severe. Common clinical characteristics include:
- Ocular Pain: Patients frequently report eye pain as a result of inflammation.
- Redness: The affected eye may appear red as a result of uveal blood vessel engorgement.
- Blurred Vision: Inflammation can cause visual disturbances, including blurred vision.
- Photophobia: One of the most common symptoms is sensitivity to light.
- Lacrimation: Tear production may increase in response to irritation.
- Anterior Chamber Reaction: Inflammatory cells and protein exudates can accumulate in the anterior chamber, causing flares and cells to appear under a slit lamp.
Types of Lens-Induced Uveitis
- Phacoanaphylactic Uveitis: This is an immune-mediated reaction that occurs when lens proteins leak following trauma or surgery, resulting in granulomatous inflammation.
- Phacotoxic Uveitis: This type develops as a result of the toxic effect of lens proteins on intraocular tissues. It is most common in hypermature cataracts where the lens material slowly leaks.
- Phacolytic Uveitis: This condition results from the leakage of high-molecular-weight lens proteins through an intact lens capsule and is frequently associated with hypermature cataracts.
Epidemiology
Lens-induced uveitis is uncommon compared to other types of uveitis, but it is significant because it has the potential to cause serious complications. It can affect people of all ages, but it is most common in older adults who have cataracts or have had ocular trauma or surgery.
Pathogenesis
The pathogenesis of lens-induced uveitis includes both humoral and cellular immune responses. When lens proteins come into contact with the immune system, they act as antigens, stimulating antibody production and T-cell activation. The resulting immune response causes inflammation and damage to the ocular tissues.
- Humoral Immunity: B-cells generate antibodies against lens proteins, resulting in immune complexes that accumulate in the eye and contribute to inflammation.
- Cell-Mediated Immunity: T-cells are activated and migrate to the site of antigen exposure, releasing cytokines that maintain the inflammatory response.
Complications
If not treated promptly and adequately, lens-induced uveitis can lead to a number of complications:
- Secondary Glaucoma: Inflammation can clog the trabecular meshwork, reducing aqueous humor outflow and raising intraocular pressure.
- Cataract Formation: Chronic inflammation can hasten cataract development.
- Posterior Synechiae: Adhesions between the iris and lens can form, resulting in an irregular pupil shape and preventing aqueous humor flow.
- Cystoid Macular Edema: Inflammation can cause fluid to accumulate in the macula, resulting in vision loss.
- Retinal Detachment: Severe or prolonged inflammation can weaken the retinal structure, raising the possibility of detachment.
Differential Diagnosis
Distinguishing lens-induced uveitis from other types of uveitis is critical for effective treatment. Differential diagnosis includes:
- Infectious Uveitis: A bacterial, viral, fungal, or parasitic infection.
- Autoimmune Uveitis: Linked to systemic autoimmune diseases like rheumatoid arthritis and sarcoidosis.
- Traumatic Uveitis: An injury to the eye that causes inflammation.
Diagnostic methods
To confirm the condition and determine the underlying cause of lens-induced uveitis, a comprehensive approach involving clinical evaluation, laboratory tests, and imaging techniques is required.
Clinical Evaluation
- Patient History and Symptoms: A thorough history of symptoms, recent ocular trauma, surgery, or pre-existing conditions such as cataracts is required. Symptoms such as eye pain, redness, blurred vision, and photophobia provide important diagnostic information.
- Visual Acuity Test: Measuring visual acuity helps determine the severity of vision impairment.
- Slit-Lamp Examination: This examination provides a thorough examination of the anterior segment, revealing signs of inflammation such as cells, flare, and keratic precipitates. It can also detect lens abnormalities such as swelling, discoloration, and leakage.
Intraocular Pressure Measurement
- Tonometry: Measuring intraocular pressure (IOP) is critical because elevated IOP can indicate secondary glaucoma due to inflammatory blockage of the trabecular meshwork.
- Gonioscopy: Examining the anterior chamber angle can aid in determining potential angle closure or synechiae formation.
Lab Tests
- Aqueous Humor Analysis: In cases of suspected lens-induced uveitis, analyzing the aqueous humor can detect the presence of inflammatory cells, proteins, and immune complexes, which can help with diagnosis.
- Blood Tests: These can be used to rule out systemic infections or autoimmune conditions that may cause similar symptoms.
Imaging Techniques
- Ultrasound Biomicroscopy (UBM): UBM produces high-resolution images of anterior segment structures, which aids in the detection of lens dislocation, capsular rupture, and residual lens material.
- Optical Coherence Tomography (OCT): OCT imaging can reveal macular edema or retinal thickening caused by uveitis.
- Fundus Fluorescein Angiography (FFA): FFA visualizes the retinal vasculature and identifies areas of leakage or edema that indicate inflammation.
Differential Diagnosis
A thorough evaluation is required to distinguish lens-induced uveitis from other types of uveitis or ocular conditions.
- Infectious Uveitis: Laboratory tests and imaging can rule out infections such as toxoplasmosis, herpes, and syphilis.
- Autoimmune Uveitis: Blood tests for autoimmune markers (such as ANA and HLA-B27) can help distinguish autoimmune-related uveitis.
- Traumatic Uveitis: A history of recent trauma and the presence of external injuries may indicate traumatic uveitis.
Lens-induced uveitis treatment
To avoid recurrence and complications, lens-induced uveitis treatment focuses on inflammation management, symptom relief, and addressing underlying lens pathology. The specific approach is determined by the severity of the condition and its underlying cause.
Medical Management
- Corticosteroids: Corticosteroids are the primary treatment for reducing inflammation. They can be administered in a variety of ways, including:
- Topical Corticosteroids: For mild to moderate cases, eye drops such as prednisolone acetate are common.
- Oral Corticosteroids: For more severe inflammation, oral steroids such as prednisone may be recommended.
- Periocular or Intravitreal Injections: For severe or refractory uveitis, corticosteroids can be injected around or directly into the eye.
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): NSAID eye drops can reduce inflammation and pain and are frequently used in conjunction with corticosteroids.
- Immunosuppressive Agents: When corticosteroids do not effectively control inflammation, immunosuppressive drugs such as methotrexate or cyclosporine may be used. These medications help to suppress the immune system and reduce inflammation.
- Cycloplegic Agents: Drugs like atropine or cyclopentolate are used to dilate the pupil and relieve pain caused by iris muscle spasms. They also help to prevent the formation of posterior synechiae.
Surgical Interventions
Surgery may be required to address the underlying lens pathology that contributes to uveitis.
- Cataract Extraction: When hypermature cataracts cause phacolytic or phacotoxic uveitis, cataract extraction is required to remove the inflammatory stimulus. The preferred method is phacoemulsification, which involves lens fragmentation via ultrasonic technology.
- Lens Fragment Removal: Surgical removal of residual lens fragments from the anterior chamber is required to resolve inflammation in lens particle uveitis.
- Lens Exchange: If you have ectopia lentis or a dislocated lens, you may need lens exchange surgery to replace it with an intraocular lens implant.
Innovative and Emerging Therapies
- Biological Agents: Monoclonal antibodies that target specific inflammatory pathways are being investigated for the treatment of uveitis. Adalimumab (an anti-TNF drug) has shown promise in treating refractory uveitis.
- Intravitreal Implants: Long-acting corticosteroid implants, such as fluocinolone acetonide, can provide continuous drug delivery, eliminating the need for frequent injections.
- Nanotechnology: Researchers are working to create nanoparticle-based drug delivery systems capable of providing targeted and sustained release of anti-inflammatory medications within the eye.
Post-operative Care
Postoperative care is critical to ensure proper healing and avoid complications.
- Anti-inflammatory Medications: To control postoperative inflammation, continue to use topical or oral anti-inflammatory medications.
- Regular Follow-Up: Patients should have frequent follow-up visits to monitor IOP, check for signs of recurrent inflammation, and ensure the surgical site is healing properly.
- Infection Prevention: To avoid post-operative infections, prophylactic antibiotics may be prescribed.
Lens-induced uveitis is effectively managed with a combination of medical and surgical interventions tailored to the individual patient’s needs, with a focus on reducing inflammation and addressing underlying lens pathology.
Effective Ways to Improve and Prevent Lens-Induced Uveitis
- Regular Eye Exams: Have routine eye exams to detect and treat early signs of lens abnormalities or cataracts before they progress to uveitis.
- Protect Eyes from Trauma: Wear protective eyewear when participating in activities that increase the risk of eye injury, such as sports or hazardous work environments, to avoid lens capsule rupture and subsequent uveitis.
- Manage Systemic Diseases: Treat systemic conditions like diabetes and autoimmune diseases, which can increase the risk of cataracts and lens dislocation.
- Monitor Post-Surgical Healing: Following cataract or other intraocular surgeries, consult with your ophthalmologist to ensure proper healing and detect any signs of lens-induced inflammation early.
- Avoid Delayed Cataract Surgery: Treat cataracts as soon as possible to avoid hypermature growth and protein leakage, which can cause inflammation.
- Use Anti-inflammatory Medications as Prescribed: To avoid chronic inflammation, follow prescribed anti-inflammatory regimens, particularly after eye surgeries or injuries.
- Educate on Symptoms: Be aware of the symptoms of uveitis, which include eye pain, redness, blurred vision, and photophobia, and seek immediate medical attention if they occur.
- Healthy Lifestyle: Eat a well-balanced diet high in antioxidants and nutrients to improve overall eye health and possibly delay the onset of cataracts.
- Avoid Smoking: Smoking can aggravate oxidative stress and inflammation, raising the risk of cataracts and subsequent uveitis.
Trusted Resources
Books
- “Uveitis: Fundamentals and Clinical Practice” by Robert B. Nussenblatt and Scott M. Whitcup
- “Lens and Cataract” by David F. Chang
- “Cataract Surgery: Technique, Complications, and Management” by Roger F. Steinert
Online Resources
- American Academy of Ophthalmology (AAO) – aao.org
- National Eye Institute (NEI) – nei.nih.gov
- American Uveitis Society – uveitissociety.org
- MedlinePlus – Uveitis – medlineplus.gov






