Dry, itchy eyes can be more than just an occasional annoyance. For those dealing with chronic ocular discomfort—often linked to Meibomian Gland Dysfunction (MGD)—everyday activities like working at a computer or driving at night can become daunting tasks. Many people notice their eyes burning or watering excessively, while over-the-counter remedies frequently offer only fleeting relief. These persistent symptoms often lead individuals to seek out new and more advanced treatment approaches that target the root causes of MGD rather than just the symptoms.
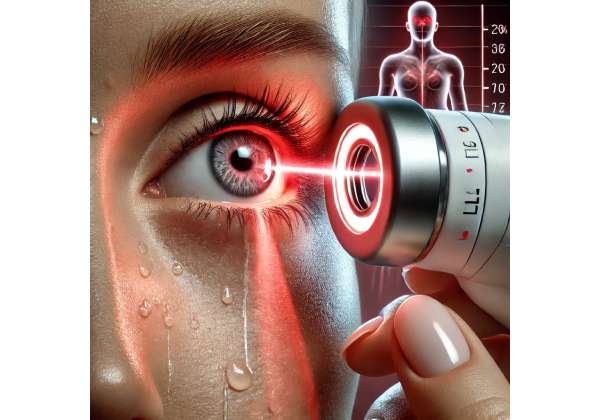
Low-level light therapy has emerged as a promising tool in this quest for more effective relief. Employing specialized wavelengths of light, this approach aims to address the underlying glandular issues that give rise to dryness and inflammation. Unlike basic home remedies and conventional drops, low-level light therapy aspires to promote healthier tear-film stability by enhancing the function of the meibomian glands themselves. Below, we delve into how this therapy works, why it’s generating buzz among eye care professionals, and what patients can expect should they opt for this innovative route.
Unraveling Low-Level Light Therapy for Dry Eye
The meibomian glands, located along the rim of the eyelids, produce the lipid layer of the tear film. This oily component is essential for preventing tears from evaporating too quickly. In Meibomian Gland Dysfunction, these glands either become clogged or produce inadequate or poor-quality oils, leading to the hallmark dryness, irritation, and fluctuating vision many sufferers report. Given that MGD is considered the leading cause of evaporative dry eye, effective treatments must do more than merely alleviate surface-level discomfort.
A Paradigm Shift Toward Gland-Centric Therapies
Historically, conventional management for MGD included warm compresses, eyelid scrubs, and artificial tears. While these interventions can help, they often provide incomplete relief. Over time, chronic MGD can even lead to permanent changes in gland structure, making it more resistant to basic self-care measures. Recognizing this, eye care specialists have turned their focus to more direct strategies aimed at restoring or improving the glands’ functionality.
Low-level light therapy (LLLT) represents one such strategy. Initially used in dermatology and sports medicine, LLLT applies controlled, low-intensity light to tissues in need of healing or rejuvenation. When directed at the eyelids, it may help soften blockages in the meibomian glands while stimulating local blood flow and cellular repair. This approach stands apart from more traditional techniques that rely on intense heat or mechanical force, potentially offering a gentler alternative for people with sensitive skin or eyes.
Distinguishing Low-Level Light Therapy from Heat-Based Modalities
It’s important to differentiate LLLT from other heat-based therapies such as thermal pulsation. Thermal pulsation devices like LipiFlow use targeted heat and pressure to liquefy and express hardened oils within the glands. Although many patients find success with such methods, they can sometimes be uncomfortable or unsuitable for those with delicate eyelids or certain ocular conditions. By contrast, LLLT delivers light energy at cooler, carefully calibrated wavelengths, often resulting in less direct heat to the eyelid surface.
Another potential advantage of LLLT is its reported anti-inflammatory effect. Some theories suggest that the specific wavelengths used (often in the red or near-infrared range) can modulate inflammatory markers and boost tissue repair at the cellular level. This dual mechanism—softening blockages and reducing inflammation—might make LLLT a valuable option for patients who experience frequent flare-ups or secondary eyelid inflammation.
Key Components of LLLT
- Wavelength Selection: Low-level light therapy devices typically use red or near-infrared wavelengths, as these have demonstrated benefits in cellular activation and tissue recovery.
- Low-Intensity Output: Unlike lasers or intense pulsed light (IPL), LLLT devices emit gentle, non-coherent light that is absorbed gradually by the target area.
- Session Duration and Frequency: Sessions may last anywhere from a few minutes to 20 minutes per eye, with the total treatment frequency varying based on the severity of MGD.
Because of its non-invasive nature, many people find that LLLT integrates well into a comprehensive dry eye management plan. Typically, clinicians may pair LLLT with eyelid hygiene, lubricating drops, and nutritional support (like omega-3 fatty acid supplements) to reinforce and extend the benefits gained.
Addressing Eyelid Inflammation and Redness
Many MGD sufferers also contend with blepharitis or ocular rosacea—conditions involving chronic eyelid redness, scaling, and irritation. The synergy between MGD and lid inflammation often forms a vicious cycle: irritated lids exacerbate dryness, and dryness further inflames the eyelids. One of the standout claims of low-level light therapy is its potential to reduce this inflammatory loop. Studies in other medical fields have shown that LLLT can limit the production of pro-inflammatory cytokines and possibly promote microcirculation, thereby diminishing redness and swelling.
While not all patients experience dramatic results, those with mild to moderate eyelid redness might see improvements in both appearance and comfort after a series of treatments. This anti-inflammatory angle is particularly appealing for those who have not responded well to prescription steroid drops or who prefer to avoid long-term steroid use due to potential side effects.
Minimal Discomfort and Potential Cumulative Benefits
Unlike therapies that rely on physically expressing the glands, LLLT is known for being comfortable and non-painful. Many patients describe it as a warm, soothing experience. Additionally, the cumulative nature of photobiomodulation suggests that multiple sessions may yield progressive benefits. As the eyelid tissues increasingly respond to the light, new blood vessels could form, nutrient delivery might improve, and meibomian gland secretions could become more stable over time. This progression may mean that consistent follow-up and maintenance sessions are recommended for extended relief.
That said, results can vary. Individuals with extensive gland dropout—where the glands are severely atrophied—might derive limited benefit, as you cannot resuscitate fully destroyed glandular tissue. Realistic expectations, coupled with a willingness to maintain ongoing treatments and adjunctive care, is key to maximizing outcomes.
Who Might Benefit Most from LLLT?
- Mild-to-Moderate MGD: Patients in the early or middle stages of gland dysfunction, who still retain enough gland structure to be salvaged or stimulated, often see the best results.
- Chronically Inflamed Eyelids: Individuals grappling with ongoing eyelid redness or mild blepharitis may appreciate LLLT’s potential anti-inflammatory effects.
- Those Sensitive to Heat Treatments: Some people find thermal pulsation devices or heated compresses irritating; LLLT might offer a gentler alternative.
- Combination Therapy Seekers: Anyone looking to elevate their existing regimen of lid hygiene, warm compresses, or medication might discover enhanced benefits when adding LLLT to the mix.
In contrast, those with severely advanced gland dropout, or underlying systemic conditions that severely affect tear production (e.g., Sjögren’s syndrome), might find that LLLT offers limited gains. A thorough exam with an eye care professional is essential to gauge whether the therapy is appropriate.
Practical Steps and Protocols in Using Light Therapy
Low-level light therapy offers a fairly straightforward experience for patients, particularly once it’s determined that they’re suitable candidates. Because MGD involves complex tear-film disturbances, eye doctors often take a multi-step approach that begins with a detailed assessment of gland health, tear function, and eyelid condition. From there, they develop a tailored treatment plan that includes LLLT sessions at appropriate intervals.
Evaluating Candidacy and Preparation
The first step in determining whether LLLT aligns with a patient’s needs involves a thorough ocular exam. Common diagnostic tools include:
- Meibography: Imaging to visualize the structure and number of meibomian glands.
- Tear Film Analysis: Tests such as tear osmolarity or tear breakup time (TBUT) to gauge the stability of the tear film.
- Eyelid Assessment: Inspection for signs of blepharitis, Demodex mite infestation, or ocular rosacea that may influence treatment outcomes.
If substantial gland dropout or severe ocular surface disease is detected, the eye doctor may recommend stabilizing the condition with medical therapy before introducing light treatment. Likewise, patients with active infections, certain corneal abnormalities, or photosensitivity disorders should discuss these thoroughly with their doctor to avoid complications.
The Treatment Environment
During an LLLT session, patients are typically seated in a reclined chair. Protective eyewear or shields might be used, depending on the device’s design. The low-level light source can be applied via a handheld device or a specialized mask that fits snugly over the eyelids. Sessions typically last 10–20 minutes, during which the gentle light is directed at the meibomian glands.
Some practitioners might combine LLLT with a mild warming effect, though the temperature is generally much lower than that used by devices specifically designed for thermal pulsation. The aim is to encourage blood flow and gently loosen any meibomian gland blockages without overheating the delicate eyelid tissues.
Number of Sessions and Interval
Because photobiomodulation tends to have cumulative effects, multiple sessions are usually necessary. A common schedule might involve weekly or bi-weekly treatments over a one- or two-month period. However, some providers choose more extended intervals, depending on how quickly a patient responds and the severity of gland dysfunction. After the initial series, maintenance sessions every few months may help preserve improvements—especially for patients prone to relapses or those living in harsh, dry climates.
Integrating Manual Expression and Hygiene
Many eye doctors incorporate eyelid expression, either before or after light therapy, to remove any softened blockages. By manually compressing the gland openings along the eyelid margin, stagnant or congealed oils can be extracted, facilitating the production of healthier meibum. This approach is particularly popular when combining LLLT with other advanced techniques. In some cases, clinicians may use specialized lid-cleaning tools, microblepharoexfoliation devices, or antibacterial solutions to ensure the eyelid margin remains clear of debris and harmful bacteria.
Patients are also encouraged to continue at-home eyelid hygiene between appointments—this might include warm compresses, lid scrubs, and artificial tears. Doing so can prolong the benefits of LLLT, keeping the glands free-flowing until the next session. Certain doctors might suggest nutritional supplements, like omega-3 fatty acids, to support meibum composition from within.
Addressing Discomfort and Post-Treatment Recommendations
One of the advantages of low-level light therapy is its generally mild side effect profile. Most patients experience little to no discomfort during or after the procedure. If mild irritation or redness does occur, it typically subsides within a few hours. To further minimize sensitivity, some clinics offer soothing eye drops or cool compresses immediately following each session.
After treatment, patients can generally resume their normal daily activities, including using digital devices. They’re advised to pay attention to any changes in eye comfort, lubrication needs, or eyelid appearance so they can report back at subsequent visits. For those noticing persistent dryness or other symptoms, a quick follow-up call or appointment may help the doctor adjust the treatment plan or suggest supportive measures.
Potential Contraindications and Precautions
Although LLLT is considered low-risk, certain populations should exercise caution. For instance, individuals with epilepsy or seizure disorders triggered by flashing lights should thoroughly discuss the risks with their healthcare providers. Likewise, pregnant or breastfeeding women should consult with an ophthalmologist about LLLT’s safety profile, as formal research in this demographic might be limited.
Finally, patients who rely heavily on photosensitive medications—like certain antibiotics or chemotherapy drugs—must clarify whether LLLT poses additional risks. Shielding the eyes or adjusting medication schedules may be necessary in specific cases. An open dialogue between patient and practitioner ensures that any possible complications are anticipated and managed proactively.
In sum, the practical application of low-level light therapy for MGD is grounded in a structured yet adaptable series of treatments. By pairing LLLT with thorough pre-assessments, manual gland expression, and consistent home care, many patients stand to experience meaningful improvements in dryness, comfort, and daily functioning.
Current Research and Real-World Evidence
Low-level light therapy’s role in managing Meibomian Gland Dysfunction remains a relatively recent development, yet a growing body of clinical findings and anecdotal reports points to its promise. Early adopters—both practitioners and patients—often share encouraging feedback, noting reductions in dryness, inflammation, and dependency on lubricating eye drops. However, as with any evolving treatment, further large-scale investigations are essential to fully understand its long-term efficacy, optimal protocols, and potential limitations.
Pioneer Studies and Preliminary Trials
Several small-scale pilot studies have paved the way for LLLT’s acceptance in eye care settings:
- Journal of Ocular Surface Therapies (2020): A preliminary study followed 15 patients with moderate MGD who underwent weekly LLLT sessions for four weeks. Most participants reported noticeable relief from dryness and itching by the end of the treatment series. Objective measures, such as tear breakup time, also improved, indicating a tangible enhancement in tear film stability.
- Clinical Ophthalmology Reports (2021): This observational study tracked 25 participants receiving combined low-level light therapy and mechanical eyelid expression. Researchers found that, on average, patients realized a 25% reduction in corneal staining scores and a 30% boost in tear stability. Notably, even individuals who had previously failed to respond to thermal pulsation therapy saw significant gains, suggesting that LLLT may offer a distinct mechanism of action.
These studies, while limited by their small sample sizes and lack of control groups, helped establish a baseline understanding of how LLLT could serve as a feasible intervention for evaporative dry eye.
Comparative Findings with Other Treatments
Direct comparisons between low-level light therapy and alternative advanced MGD interventions (such as intense pulsed light or thermal pulsation) are still emerging. However, preliminary indications suggest LLLT might confer particular advantages in addressing inflammation and eyelid redness:
- Intense Pulsed Light (IPL): IPL targets vascular irregularities and is sometimes used to reduce eyelid telangiectasia that can worsen MGD. While IPL has shown successes, some patients experience discomfort or react poorly to intense light bursts. LLLT, with its gentler approach, may be preferable for those seeking a cooler, less intense alternative.
- Thermal Pulsation (e.g., LipiFlow): Known for delivering heat and pressure directly to meibomian glands, thermal pulsation is well-established. That said, patients with very sensitive skin or advanced ocular surface inflammation sometimes find it too invasive. LLLT’s non-contact approach could fill a gap for those who require a more delicate yet effective modality.
A crucial factor in these comparisons is that every patient’s condition varies in severity, gland structure, and tolerance. Rather than viewing each therapy as mutually exclusive, some ophthalmologists now explore combination treatments to leverage the unique benefits of each modality—e.g., an initial course of thermal pulsation followed by maintenance LLLT sessions to preserve gains and manage inflammation.
Expanded Role in Ocular Rosacea and Lid Margin Disease
Beyond pure meibomian gland blockage, LLLT may prove valuable for ocular rosacea, a chronic condition that features inflamed eyelids and visible blood vessels. In many patients, ocular rosacea exacerbates meibomian gland dysfunction by creating a perpetually inflamed environment around the gland openings. By calming local inflammation, LLLT could interrupt the cyclical damage that ocular rosacea inflicts on the glands.
Case reports presented at the 2022 American Academy of Ophthalmology meeting illustrated how a small number of ocular rosacea patients achieved sustained symptom relief after combining LLLT with standard medical therapy (like topical antibiotics or immunomodulators). While more controlled research is needed, these observations point to a potentially significant role for LLLT in broader lid margin disease contexts.
Patient Satisfaction and Quality of Life
Anecdotally, many patients describe LLLT as offering a refreshing, spa-like experience. They often report immediate soothing effects during treatment sessions, attributing this relaxation to the gentle warmth and mild massaging sensation sometimes produced by the light sources. Over the course of multiple treatments, improvements in daily comfort—like less reliance on artificial tears and a diminished burning sensation when staring at a digital screen—translate to tangible quality-of-life enhancements.
In a 2022 retrospective survey shared by a European eye clinic, nearly 70% of 40 responding MGD patients indicated that LLLT met or exceeded their expectations. A sizeable portion claimed it allowed them to return to activities that were previously curtailed by dryness, such as reading or gaming for extended periods. While subjective perceptions can vary widely, this user satisfaction underscores the interest in maintaining LLLT as part of ongoing dry eye management.
Limitations and Calls for Further Investigation
Despite promising signs, some key questions remain:
- Longevity of Results: Just how lasting are the improvements gained from LLLT? Many providers believe maintenance sessions are critical, but more longitudinal data is needed to confirm how often these sessions should be administered to sustain improvements.
- Optimal Dosage and Wavelengths: Current devices differ in their emitted wavelengths, intensity levels, and usage durations. Identifying the best combination for maximum gland rejuvenation and minimal discomfort demands additional rigorous studies.
- Cost-Effectiveness: While some clinics already tout LLLT as a cost-effective solution relative to repeated prescription medications or office visits, formal analyses that incorporate patient outcomes and financial metrics over time are still underway.
Large-scale, randomized controlled trials (RCTs) comparing LLLT with standard MGD treatments would offer the clearest insights. Industry experts advocate for multi-center RCTs that factor in a variety of patient demographics, MGD severities, and ocular comorbidities. Such research could establish a more standardized protocol for LLLT use and help doctors recommend precise treatment schedules.
Real-World Experiences
In day-to-day practice, ophthalmologists and optometrists who have integrated LLLT into their services often highlight its patient-friendly nature as a central selling point. Eye doctors can seamlessly incorporate the sessions into typical clinic workflows; treatment times are usually short, and patient preparation is minimal. This logistical convenience, combined with the perceived comfort of the therapy, contributes to its growing popularity among both practitioners and the people they serve.
As the evidence base broadens, low-level light therapy is poised to become a mainstay choice—especially for those who haven’t found success with other advanced treatments or are searching for a gentle yet potentially effective means of tackling MGD at its core. For those ready to test a pioneering solution to chronic dry eye, the rising tide of positive reports surrounding LLLT offers a hopeful sign.
Gauging Success and Safety
When introducing a novel therapy for MGD, questions about effectiveness and safety are paramount. The consensus among many eye care professionals is that low-level light therapy offers an appealing balance: potential relief from inflammation, improved tear stability, and minimal discomfort during and after the procedure. But as with any medical intervention, it’s vital for patients to weigh potential risks, manage expectations, and maintain open communication with their healthcare providers.
Effectiveness in Clinical Settings
In practice, LLLT often yields noticeable benefits such as reduced dryness, less eyelid redness, and a lower dependence on artificial tears. Patients may also report fewer episodes of fluctuating vision, especially when engaged in visually demanding tasks. While some individuals experience significant relief relatively quickly, others might observe gradual improvements as multiple sessions build upon each other. Additionally, pairing LLLT with lid hygiene, dietary supplements, and periodic manual gland expression tends to amplify these gains and sustain them longer.
Overall Safety Profile
Low-level light therapy is generally considered low-risk, particularly when administered by trained professionals who follow established guidelines. Because the treatment relies on cool or warm light rather than concentrated heat or harsh pressure, it avoids many of the potential irritations associated with thermal pulsation devices. Common side effects include mild eyelid redness or a transient feeling of warmth in the treated area, both of which typically resolve within a short period. Adverse events like infection, corneal damage, or severe inflammation remain rare.
Nonetheless, certain groups—such as pregnant individuals, people with photosensitive conditions, or those on specific medications—should discuss their circumstances in depth with their eye care providers. A thorough pre-treatment assessment and follow-up check can prevent complications, ensuring that the therapy remains both safe and effective.
Financial Factors to Keep in Mind
Fees for low-level light therapy vary depending on factors like clinic location, the complexity of each patient’s MGD, and the number of treatment sessions required. In many U.S.-based practices, patients can expect prices ranging from \$200 to \$400 per session, though bundled packages may offer discounts if multiple visits are anticipated. Insurance coverage for LLLT is not yet common, as it is frequently considered an elective or emerging procedure. Patients may wish to explore health savings account (HSA) or flexible spending account (FSA) options to offset some out-of-pocket costs.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider about any personal health concerns.
If you found this discussion on low-level light therapy helpful, feel free to share it on Facebook or X (formerly Twitter) so that others dealing with Meibomian Gland Dysfunction can explore potential solutions for relief.










