If you’ve ever struggled to read traffic signs in the distance or found yourself holding books inches from your face, you know the inconveniences of nearsightedness (myopia). But in some cases, myopia brings more than just the usual squinting and headaches. For certain individuals, progressive myopia can lead to a serious complication called myopic choroidal neovascularization (CNV)—an overgrowth of abnormal blood vessels beneath the retina that can threaten central vision. That’s where Lucentis (ranibizumab) comes in as a game-changer. Designed to tackle the vascular issues that drive vision loss, Lucentis offers new hope for those at risk of losing their sight to this rare but damaging condition.
Myopic choroidal neovascularization might not receive as much attention as age-related macular degeneration, but its impact on quality of life can be just as profound. People with high myopia often worry that every new blur or distortion in their field of view signals the start of something worse. Thanks to growing evidence and modern treatment protocols, Lucentis injections can help stabilize or even improve vision in many patients with myopic CNV. If you’ve been wondering how this therapy works and whether it’s right for you or a loved one, this article covers the essentials—from how Lucentis halts abnormal vessel growth to what the latest research reveals about long-term outcomes.
How Lucentis Combats Choroidal Neovascularization in High Myopia
Myopic choroidal neovascularization arises when structural changes in an elongated, highly myopic eye lead to microscopic tears or disruptions in the layers beneath the retina. In response, the body grows fragile new blood vessels (neovascular membranes) in an attempt to repair or compensate for these injuries. Unfortunately, these vessels tend to be leaky and poorly organized, causing fluid and blood to accumulate under the retina. This accumulation can warp central vision—distorting straight lines or creating dark spots that make reading and detailed tasks difficult.
Why Anti-VEGF Therapy Matters
A key factor behind these abnormal vessels is a protein called vascular endothelial growth factor (VEGF). Under stress—such as that seen in highly stretched tissues of a myopic eye—the retina and surrounding structures produce more VEGF to spur new vessel growth. While the intention is healing, the result in CNV is often destructive. That’s where Lucentis steps in. It’s classified as an anti-VEGF agent, meaning it neutralizes the excess VEGF floating around in the eye. By blocking VEGF from binding to receptors on blood vessels, Lucentis:
- Slows or Stops New Vessel Growth: Fewer abnormal vessels mean less risk of fluid leakage and hemorrhages under the retina.
- Stabilizes Existing Damage: Reducing the inflammatory and growth signals can prevent further scarring, preserving more healthy retinal tissue.
- Enhances Potential for Visual Recovery: Even partial reabsorption of fluid can improve how light hits the photoreceptors, leading to sharper images reaching the brain.
Specifics of Lucentis in Myopic CNV
Lucentis (ranibizumab) is a fragment of a monoclonal antibody specifically engineered for use in the eye. Though it’s also employed in conditions like wet age-related macular degeneration and diabetic macular edema, its success in myopic CNV underscores the shared role of VEGF across multiple retinal diseases. Unlike certain other anti-VEGF agents, Lucentis was designed with the eye in mind—this means it has a relatively short systemic half-life, reducing the likelihood of body-wide side effects, while still hitting high concentrations within the vitreous cavity and retina.
Key Signs and Symptoms Addressed by Lucentis
Patients with myopic CNV often notice sudden or gradual changes to their central vision:
- Grayish or dark spots (scotomas) that obscure letters or parts of a page
- Straight lines appearing bent or wavy, a phenomenon called metamorphopsia
- Reduced contrast sensitivity, making reading and nighttime driving more challenging
- Colors seeming duller or less vivid than usual
By shrinking or stabilizing the neovascular membranes, Lucentis can alleviate many of these symptoms, allowing the macula to regain a more normal contour.
Considering Early Intervention
One critical aspect of myopic CNV is that it can progress rapidly. The sooner therapy is initiated, the higher the chance of preserving functional vision. While some small membranes might regress spontaneously, many do not—and waiting might risk permanent scarring. If you or your eye specialist suspect new CNV (signs might include sudden blurriness or distortions), scheduling a prompt evaluation and possible treatment can make a considerable difference in long-term outcomes.
Balancing Myopia Management and CNV Control
Even as you address the immediate threat of CNV, it’s crucial to remember that high myopia itself comes with other risks—like retinal detachment or macular holes. Maintaining routine ophthalmic check-ups ensures that any new or emerging conditions are caught early. Some patients pursue contact lenses or refractive surgery to reduce dependence on glasses, but these interventions don’t address the structural factors behind myopia-induced stretch and potential CNV formation. Lucentis is specifically about halting the sight-threatening aspect of abnormal vessel growth, making it a vital tool rather than a cure for the myopic eye’s elongated shape.
Integration with Modern Eye Care Approaches
As anti-VEGF therapy has evolved, so have supplementary techniques. Optical coherence tomography (OCT) scans let doctors precisely measure fluid buildup and track subtle shifts in retinal thickness, guiding the timing of injections. In select cases, your doctor might supplement anti-VEGF with focal laser photocoagulation or photodynamic therapy (PDT), especially if scarring extends beyond the macular center. However, many myopic CNV patients do well on Lucentis alone, especially given the therapy’s direct targeting of the molecular driver—VEGF—that spurs neovascular growth.
Lucentis’s role in controlling myopic CNV is significant, but equally important is how it’s actually administered and what to expect if you move forward with treatment. Understanding the application and protocols can help you feel more prepared if you’re newly diagnosed or if you’re comparing it to other therapeutic avenues.
Steps Involved: How Lucentis Is Administered and Monitored
For many people, the thought of an injection into the eye is concerning. Fortunately, the procedure for intravitreal Lucentis is well-established and generally quick, minimizing discomfort and potential complications. The application process is similar across various retinal disorders, though myopic CNV does come with some nuances in monitoring.
The Pre-Treatment Evaluation
Before you receive your first injection of Lucentis for myopic choroidal neovascularization, your ophthalmologist or retina specialist will likely:
- Review Detailed Medical History: This includes checking whether you’ve had prior eye surgeries, allergies to medications, or any systemic conditions (like uncontrolled hypertension) that might complicate treatment.
- Perform Comprehensive Eye Exams: Expect a visual acuity test, tonometry (eye pressure measurement), and an evaluation of the fundus through dilated pupil examination.
- Obtain OCT and Possibly Fluorescein Angiography (FA): OCT imaging gives a cross-sectional view of the retina, identifying any fluid pockets or thickening. FA involves injecting a special dye into the bloodstream to highlight abnormal vessels in the back of the eye. Together, these help confirm CNV activity and gauge how urgent therapy might be.
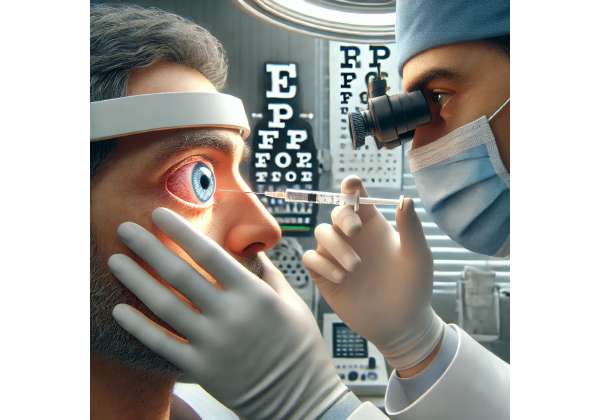
Intravitreal Injection Process
Once it’s clear that Lucentis is appropriate for your condition, an injection date is scheduled. Here’s what typically happens on the day of treatment:
- Sterilization and Anesthesia: The surface of your eye is cleansed with an antiseptic solution, and topical anesthetic drops are applied to reduce pain.
- Positioning and Lid Speculum: You’ll lie back or lean in a specialized chair, and a small device may be used to gently keep your eyelids open.
- Intravitreal Injection: Using a fine needle, the specialist injects a measured dose of Lucentis into the vitreous cavity (the gel-filled area in the middle of the eyeball). This moment usually lasts just a few seconds.
- Post-Injection Observation: The medical team may check your intraocular pressure and overall eye condition. Some patients experience mild redness, irritation, or a sensation of pressure, but significant pain is uncommon. You’ll typically use antibiotic drops for a few days post-injection to reduce infection risk.
A common concern is whether the injection might “hurt.” Most patients describe it as a brief, mild discomfort, especially when numbing is done properly. The entire office visit is often under an hour from start to finish.
Follow-Up Scheduling and Management
Lucentis therapy often follows one of several approaches, depending on your unique response and your specialist’s protocol:
- Monthly Injections (Loading Phase): In some practices, you receive an injection monthly for three months to rapidly suppress the disease. After that, you might shift to fewer injections if imaging and vision tests suggest the neovascularization is under control.
- PRN (As-Needed) Treatment: Instead of an automatic monthly regimen, your doctor monitors your retina via OCT and only injects when signs of active leakage or fluid reemerge.
- Treat-and-Extend: A hybrid approach where intervals between injections gradually lengthen (from 4 weeks to 6, 8, or more) if the retina remains stable. If fluid or bleeding reappear, the interval shrinks again.
For myopic CNV specifically, some patients achieve significant stability after just a few injections, as their membranes might be smaller or less aggressive than those in age-related macular degeneration. However, frequent checks remain critical: an apparently quiet membrane can reactivate, especially if the underlying myopia continues to exert stress on the retina.
Complementing Other Eye Health Practices
While receiving Lucentis, it’s wise to remain vigilant about overall eye health:
- Monitor Changes: If you notice new floating spots (floaters), flashes of light, or intensifying distortions, contact your doctor immediately. These could signal a complication like retinal detachment or a reactivation of CNV.
- Maintain Refractive Correction: Proper correction with glasses or contacts can help reduce eyestrain. If your prescription changes frequently, keep your retina specialist informed.
- Manage Systemic Health: Conditions like hypertension can exacerbate vascular problems in the eye, so controlling blood pressure may protect against further damage.
Handling Potential Side Effects or Concerns
Infection (endophthalmitis) is a rare but serious complication of any intraocular injection. Symptoms include severe pain, redness, and marked vision loss—prompt treatment is essential to save vision. Minor side effects like redness, a scratchy feeling, or a small subconjunctival hemorrhage (a red spot on the white of the eye) often resolve spontaneously within days. If you have a known sensitivity to ranibizumab or have experienced prior complications with anti-VEGF injections, share this with your healthcare provider to tailor your treatment plan.
By working closely with a specialized retina clinic, you can navigate any challenges that arise. The structured nature of intravitreal therapy ensures frequent follow-ups, letting you stay ahead of any complications while benefiting from the proven efficacy of Lucentis.
Current Evidence: Key Clinical Trials and Real-Life Experiences
The use of Lucentis for myopic choroidal neovascularization may sound like a novel idea, but clinical research has been backing up its efficacy for several years now. While it’s more commonly discussed in the context of age-related macular degeneration (AMD), myopic CNV has a different etiology—one grounded in the mechanical stretching of the eye. Nonetheless, the shared role of VEGF means that a therapy successful in AMD can also be highly effective in halting or reversing visual decline in severe myopia.
Landmark Clinical Studies
Several pivotal trials have laid the groundwork for Lucentis’s acceptance in myopic CNV:
- RADIANCE Trial (Published in Ophthalmology, 2014): One of the earliest large-scale studies focusing on myopic CNV, RADIANCE compared ranibizumab (Lucentis) with photodynamic therapy (PDT). Participants who received Lucentis had significantly better improvements in best-corrected visual acuity (BCVA) at three and six months. Moreover, fewer injections than expected were required to maintain gains.
- MYRROR Study (Published in American Journal of Ophthalmology, 2015): This trial evaluated another anti-VEGF agent, aflibercept, but it underscored the role of VEGF inhibition in myopic CNV. The findings indirectly bolstered Lucentis’s position because they reaffirmed that blocking VEGF effectively countered disease progression, leading to better visual outcomes.
- Meta-Analysis and Real-World Reports (Various Journals, 2016–2022): Multiple reviews have pooled data from smaller observational studies, consistently concluding that Lucentis not only improves vision in many patients with myopic CNV but also helps sustain these improvements over the long term if retreatment protocols are followed.
Insights on Injection Frequency and Durability
One interesting takeaway is that patients with myopic CNV often require fewer injections overall than those with wet AMD. In some series, people received just 3–5 injections in the first year, with some going months without additional therapy once the lesion stabilized. This lower treatment burden is partly because myopic CNV lesions can be smaller and have less robust neovascular growth than AMD lesions. Nonetheless, “fewer injections” doesn’t apply to everyone—some complex or large lesions still need frequent re-treatments.
Real-World Case Examples
Observational data and case reports from ophthalmology practices around the globe corroborate the positive results:
- Case 1: A 35-year-old patient with a history of progressive high myopia experiences sudden central distortion. OCT reveals a small subretinal hemorrhage. After three monthly Lucentis injections, fluid nearly disappears, and BCVA improves by 2–3 lines on the Snellen chart. Follow-up at one year shows stable vision with no additional injections.
- Case 2: A 50-year-old with degenerative myopia and repeated episodes of subretinal bleeding finds partial relief from PDT but continues to develop new bleeds. Transitioning to Lucentis injections significantly reduces bleed frequency, eventually restoring enough central vision for reading without magnifiers.
Combination Therapies and Special Scenarios
While Lucentis alone is sufficient for many, some advanced or recurrent CNV cases respond best to a hybrid approach:
- Lucentis + Photodynamic Therapy (PDT): PDT used to be a primary therapy for myopic CNV, but it’s generally less favored now due to the success of anti-VEGF. However, in certain large or fibrotic lesions, a single round of PDT can reduce the bulk of abnormal vessels, followed by Lucentis to mop up residual activity.
- Lucentis + Laser Photocoagulation: Focal laser can be used if CNV is extrafoveal (away from the center of the macula), though this is less common because direct laser on the macula can risk scarring.
- Treatment in Pregnancy or Other Complex Situations: While no large-scale trials focus on pregnant individuals with myopic CNV, off-label experiences indicate that careful monitoring and limiting exposure to any medication are recommended. In other special cases—like high ocular pressure or coexisting pathologies—dosages and intervals may be fine-tuned to minimize risk.
Future Directions and Ongoing Studies
Research continues on:
- Sustained-Release Implants: Investigational approaches aim to free patients from monthly visits by slowly releasing ranibizumab or similar drugs into the eye over many months.
- Gene Therapy and Novel Agents: Although primarily tested in AMD, gene-based treatments that reduce VEGF expression or new biologics could eventually extend to severe myopia cases, potentially offering even longer intervals between treatments.
- Advanced Imaging Modalities: Tools like adaptive optics scanning laser ophthalmoscopy may soon help precisely map how the therapy influences photoreceptors, giving deeper insight into which eyes respond best.
In sum, the wealth of data from controlled trials and everyday practice endorses Lucentis as a mainstay for tackling myopic CNV. It’s typically well-tolerated, and improvements in visual function can be long-lasting when follow-up is diligent. But every medical intervention has potential risks, and outcomes can vary from person to person. Hence, understanding effectiveness and safety is pivotal in deciding whether Lucentis is the right path for your unique circumstances.
How Well It Works and Key Safety Considerations
For many individuals grappling with myopic choroidal neovascularization, Lucentis can significantly enhance or stabilize vision—and, in some instances, even avert imminent legal blindness. The therapy’s success rate is high: large-scale studies often find that the majority of patients either retain their initial visual acuity or gain additional lines on the reading chart. Still, as with any intraocular injection, potential risks and side effects require vigilant attention.
Notable Efficacy Highlights
- Rapid Fluid Reduction: Patients often notice a decrease in metamorphopsia (wavy lines) within weeks, correlating with fluid reabsorption visible on OCT scans.
- Sustained Visual Gains: Many see stable improvements at six and twelve months, although occasional reactivation of CNV might necessitate further injections.
- Fewer Shots Needed: Compared to degenerative conditions like wet AMD, the number of required injections can be relatively modest—some individuals need fewer than six injections over the first year.
Typical Side Effects
- Mild Irritation or Redness: Most common and usually resolves quickly.
- Transient Intraocular Pressure Rise: Eye pressure may spike briefly after injection. Clinicians monitor and address it if necessary.
- Subconjunctival Hemorrhage: A small red spot on the eye’s surface can appear at the injection site, harmless but sometimes alarming in appearance.
- Floaters or Specks: Small air bubbles or medication droplets may cause floaters, typically dissipating within a day or two.
Serious but Rare Complications
- Endophthalmitis: A severe internal eye infection. Early signs include significant pain, vision drop, redness, and discharge. Immediate medical attention is essential.
- Retinal Detachment: Although more common in very high myopia, the injection itself is rarely the root cause. Nonetheless, prompt care is vital if detachment occurs.
- Intraocular Inflammation: Uncommon, but can lead to pain, light sensitivity, and reduced vision. Responsive to anti-inflammatory treatment.
Under the care of an experienced retina specialist, the risk of these complications is low. Sterile injection techniques and immediate follow-up if abnormal symptoms appear can further mitigate these dangers. Overall, the substantial potential benefits typically outweigh the small risk of serious adverse events, especially for those facing progressive vision loss without timely intervention.
Financial Aspects: The Cost of Lucentis Treatment
Lucentis pricing can vary based on region, insurance coverage, and healthcare facility protocols. In the United States, a single dose might range from approximately \$1,200 to \$2,000 without insurance, while in other countries, national health services or private insurance plans might shoulder some or most of the expense. Some retina clinics offer patient-assistance programs or payment plans to help individuals manage out-of-pocket costs. If affordability is a major concern, discussing alternative treatments or exploring manufacturer discount programs could provide viable options.
Disclaimer:
This article is for informational purposes only and does not replace professional medical advice. Always consult a qualified healthcare provider for individualized guidance about your eye health.
If you’ve found this overview useful, feel free to share it on social media—spreading the word can help others facing myopic CNV discover effective solutions like Lucentis.