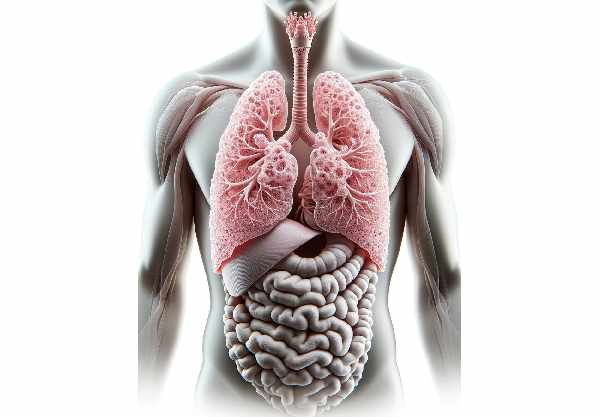
The lungs are vital respiratory organs that facilitate the essential exchange of oxygen and carbon dioxide between the air we breathe and our bloodstream. These paired organs, housed within the thoracic cavity, work tirelessly to support cellular metabolism, maintain acid-base balance, and protect the body from airborne pathogens. Their complex structure and function make them indispensable to life. This comprehensive guide delves into lung anatomy, physiology, common disorders, diagnostic methods, treatment options, nutritional supplements, and lifestyle practices to help you optimize your respiratory health.
Table of Contents
- Anatomy & Structure
- Physiology & Functions
- Common Lung Conditions
- Diagnostic Techniques
- Treatment Options
- Supplements for Lung Health
- Lifestyle Practices
- Trusted Resources
- Frequently Asked Questions
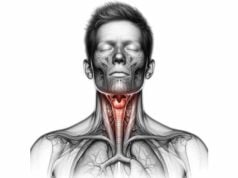
Anatomy & Structure
The lungs are complex organs divided into two distinct halves that differ in size and lobar organization. Located within the thoracic cavity and protected by the rib cage, the right lung is larger than the left, which accommodates the heart. The right lung is divided into three lobes—superior, middle, and inferior—while the left lung contains two lobes, with the cardiac notch providing space for the heart. Each lobe is further subdivided into bronchopulmonary segments, which represent the smallest functional units of the lung.
Gross Anatomy
- Lung Lobes & Fissures:
The right lung’s three lobes are separated by the horizontal and oblique fissures, and the left lung’s two lobes by an oblique fissure. These fissures delineate functional segments that receive air via the bronchial tree. - Pleural Membranes:
The lungs are enveloped by two layers of pleura. The visceral pleura adheres to the lung surface, while the parietal pleura lines the thoracic cavity. The thin, lubricated space between these layers, known as the pleural cavity, facilitates smooth respiratory movements.
Airway Structure
- Trachea and Bronchi:
Air enters through the trachea—a rigid tube reinforced by C-shaped cartilaginous rings—and bifurcates at the carina into the left and right main bronchi. Each bronchus further divides into lobar bronchi, segmental bronchi, and finally into bronchioles. This progressive branching ensures efficient air distribution throughout the lung parenchyma. - Alveolar Network:
At the terminal end of the bronchial tree, bronchioles give rise to alveolar ducts, culminating in clusters of alveoli. These microscopic air sacs are the primary sites of gas exchange. Their walls, which are only one cell thick, are surrounded by dense capillary networks that facilitate the diffusion of oxygen and carbon dioxide.
Vascular and Lymphatic Supply
- Pulmonary Circulation:
Deoxygenated blood is pumped from the right ventricle through the pulmonary arteries to the alveoli. Here, gas exchange occurs before oxygenated blood returns to the left atrium via the pulmonary veins. - Bronchial Circulation:
The bronchial arteries, arising from the aorta, supply oxygenated blood to the lung tissue itself, including the airways and supporting structures. Venous drainage occurs through bronchial veins, which eventually join the pulmonary circulation. - Lymphatic System:
A network of lymphatic vessels and nodes, particularly in the mediastinum, help filter lymph and contribute to immune surveillance, ensuring that pathogens are trapped and neutralized.
Nervous Innervation
- Autonomic Control:
The lungs are innervated by both sympathetic and parasympathetic fibers. The sympathetic nervous system primarily causes bronchodilation during physical exertion or stress, while the parasympathetic nervous system, via the vagus nerve, mediates bronchoconstriction and mucus secretion at rest.
Physiology & Functions
The lungs are the cornerstone of the respiratory system, fulfilling essential roles that support cellular respiration and overall homeostasis. They ensure that oxygen is absorbed into the bloodstream and carbon dioxide, a metabolic waste, is expelled from the body.
Gas Exchange
- Alveolar Exchange:
The alveoli, surrounded by dense capillaries, are the primary sites for gas exchange. Oxygen diffuses from the alveolar air into the blood, while carbon dioxide diffuses from the blood into the alveoli for exhalation. This process is driven by concentration gradients and facilitated by the thin respiratory membrane.
Ventilation and Airflow
- Inhalation Mechanics:
Breathing begins with the contraction of the diaphragm and intercostal muscles, which increase the volume of the thoracic cavity. This expansion decreases intrapulmonary pressure, drawing air into the lungs. - Exhalation Dynamics:
Exhalation is typically passive, occurring when the diaphragm and intercostal muscles relax, thereby decreasing the thoracic volume and increasing pressure, which forces air out. Forced exhalation involves the active contraction of abdominal muscles.
Regulation of Breathing
- Respiratory Centers:
The brainstem, particularly the medulla oblongata and pons, houses the respiratory centers that regulate the rate and depth of breathing. These centers integrate signals from chemoreceptors and mechanoreceptors to adjust ventilation in response to changes in blood oxygen, carbon dioxide, and pH levels. - Chemoreceptor Feedback:
Peripheral chemoreceptors in the carotid and aortic bodies, along with central chemoreceptors in the medulla, monitor blood gas levels and modulate respiratory drive to maintain acid-base balance.
Protective Mechanisms
- Mucociliary Clearance:
The lining of the respiratory tract features ciliated epithelium and mucus, which trap and remove inhaled particles, pathogens, and debris from the airways. This mechanism is essential for keeping the lungs free from infections and blockages. - Immune Defense:
Alveolar macrophages reside in the alveoli, providing a first line of immune defense by engulfing and destroying pathogens, while the lymphatic system filters lymph to prevent systemic spread of infections.
Additional Metabolic Functions
- Enzymatic Activity:
The lungs play a role in converting angiotensin I to angiotensin II via angiotensin-converting enzyme (ACE), an essential process in blood pressure regulation. - Surfactant Production:
Type II alveolar cells produce surfactant, a substance that reduces surface tension within the alveoli, preventing collapse and facilitating efficient gas exchange. - Thermoregulation:
The lungs contribute to body temperature regulation by evaporating heat during exhalation and by redistributing heat through blood circulation. - Phonation Support:
While the larynx is primarily responsible for sound production, the lungs provide the airflow and pressure necessary for vocalization, playing a supportive role in communication.
Common Lung Conditions
The lungs are vulnerable to a range of disorders that can impair respiratory function and overall health. Early diagnosis and management are critical for preventing long-term complications.
Asthma
- Overview:
Asthma is a chronic inflammatory disorder of the airways characterized by bronchial hyperresponsiveness. It is triggered by allergens, respiratory infections, exercise, and environmental factors. - Symptoms:
Common symptoms include wheezing, coughing, shortness of breath, and chest tightness, which can vary in severity and frequency. - Management:
Treatment involves inhaled corticosteroids, bronchodilators, and avoiding known triggers. Long-term management includes monitoring and adjusting medications as needed.
Chronic Obstructive Pulmonary Disease (COPD)
- Overview:
COPD is an umbrella term for chronic bronchitis and emphysema, conditions that lead to persistent airflow limitation. It is primarily caused by long-term smoking and exposure to pollutants. - Symptoms:
Symptoms include a chronic cough, sputum production, shortness of breath, and frequent respiratory infections. - Management:
Management strategies include smoking cessation, inhaled bronchodilators, corticosteroids, pulmonary rehabilitation, and supplemental oxygen in advanced cases.
Pneumonia
- Overview:
Pneumonia is an infection of the lung parenchyma, which can be caused by bacteria, viruses, or fungi. It results in inflammation and fluid accumulation within the alveoli. - Symptoms:
Symptoms typically include fever, cough (often productive), chest pain, shortness of breath, and fatigue. Severe cases can lead to respiratory failure. - Management:
Treatment varies by the causative organism and includes antibiotics, antiviral medications, supportive care, and sometimes hospitalization.
Pulmonary Fibrosis
- Overview:
Pulmonary fibrosis is the scarring of lung tissue, which impairs gas exchange by reducing lung elasticity and compliance. It can be idiopathic or secondary to other conditions. - Symptoms:
Symptoms include a chronic dry cough, progressive shortness of breath, fatigue, and sometimes clubbing of the fingers. - Management:
Management involves antifibrotic medications, oxygen therapy, pulmonary rehabilitation, and in severe cases, lung transplantation.
Lung Cancer
- Overview:
Lung cancer, predominantly caused by smoking, involves uncontrolled cell growth in the lung tissues. It can manifest as small cell or non-small cell lung cancer. - Symptoms:
Symptoms may include persistent cough, chest pain, hemoptysis, weight loss, and recurrent respiratory infections. - Management:
Treatment options include surgical resection, chemotherapy, radiation therapy, targeted therapy, and immunotherapy, depending on the stage and type of cancer.
Tuberculosis (TB)
- Overview:
TB is an infectious disease caused by Mycobacterium tuberculosis that primarily affects the lungs, leading to chronic inflammation and cavitary lesions. - Symptoms:
Symptoms include a persistent cough, night sweats, fever, weight loss, and hemoptysis. TB can be latent or active. - Management:
A prolonged, multidrug antibiotic regimen is essential for treating active TB, while latent TB may be managed with a shorter course of medication.
Interstitial Lung Disease (ILD)
- Overview:
ILD encompasses a group of disorders characterized by inflammation and scarring of the lung interstitium, impairing oxygen exchange. - Symptoms:
Symptoms include progressive shortness of breath, a persistent dry cough, and fatigue. ILD can be idiopathic or related to environmental exposures, autoimmune diseases, or medications. - Management:
Treatment focuses on reducing inflammation with corticosteroids or immunosuppressants, managing symptoms with oxygen therapy, and in some cases, lung transplantation.
Diagnostic Techniques & Evaluations
Effective diagnosis of lung disorders relies on a comprehensive approach that integrates clinical assessments, imaging modalities, and specialized tests to evaluate lung function and structure.
Pulmonary Function Tests (PFTs)
- Spirometry:
Measures airflow, lung volumes, and capacity by assessing the amount of air exhaled and the speed of exhalation. It is crucial for diagnosing obstructive and restrictive lung diseases. - Plethysmography:
Estimates lung volumes and airway resistance by measuring pressure changes in an enclosed chamber, useful for diagnosing restrictive lung conditions. - Diffusing Capacity (DLCO):
Evaluates how effectively gases, such as oxygen, diffuse from the alveoli into the bloodstream, aiding in the diagnosis of interstitial lung diseases and emphysema.
Imaging Modalities
- Chest X-Ray:
A basic imaging technique that provides a quick overview of lung structure, detecting conditions like pneumonia, pleural effusions, and lung masses. - Computed Tomography (CT) Scan:
Offers detailed cross-sectional images of the lungs and chest, allowing for the identification of nodules, tumors, interstitial lung disease, and emphysema. High-resolution CT is particularly useful for evaluating lung parenchyma. - Magnetic Resonance Imaging (MRI):
Although less common for lung imaging, MRI provides excellent soft tissue contrast and is used to assess vascular structures and mediastinal involvement. - Positron Emission Tomography (PET) Scan:
Often combined with CT, PET scans evaluate the metabolic activity of lung tissues, helping differentiate benign from malignant lesions and staging lung cancer.
Endoscopic and Invasive Procedures
- Bronchoscopy:
A procedure that involves inserting a flexible scope into the airways to visually inspect the bronchial tree, obtain tissue biopsies, and perform therapeutic interventions such as foreign body removal or lavage. - Bronchoalveolar Lavage (BAL):
During bronchoscopy, saline is instilled into the lung segments and then retrieved for analysis, aiding in the diagnosis of infections, interstitial lung diseases, and malignancies. - Lung Biopsy:
Tissue samples are collected either percutaneously, via bronchoscopy, or surgically to examine cellular architecture and diagnose diseases such as cancer or fibrosis.
Laboratory and Specialized Tests
- Arterial Blood Gas (ABG) Analysis:
Measures blood pH, oxygen, and carbon dioxide levels to evaluate respiratory function and detect gas exchange abnormalities. - Sputum Analysis:
Examines expectorated material to identify infectious agents, inflammatory cells, or malignant cells, useful for diagnosing pneumonia, tuberculosis, and other infections. - Molecular and Biomarker Tests:
Blood tests for markers such as troponin (for cardiac-related lung congestion), and specific tumor markers can aid in diagnosing secondary lung conditions.
Treatment Options & Therapeutic Approaches
Treatment strategies for lung diseases depend on the underlying condition, its severity, and the patient’s overall health. Options range from conservative lifestyle modifications and pharmacotherapy to advanced interventional procedures and surgical interventions.
Lifestyle Modifications
- Smoking Cessation:
Quitting smoking is the single most effective way to improve lung health, reduce inflammation, and prevent chronic lung diseases like COPD and lung cancer. - Diet and Hydration:
A balanced diet rich in antioxidants, omega-3 fatty acids, and fiber supports lung function. Adequate hydration helps maintain mucus clearance and overall respiratory health. - Regular Exercise:
Aerobic exercise, such as walking, cycling, and swimming, improves lung capacity, strengthens respiratory muscles, and enhances overall cardiovascular health. - Avoidance of Pollutants:
Limiting exposure to indoor and outdoor pollutants, such as dust, chemicals, and secondhand smoke, is crucial for preserving lung function.
Pharmacologic Treatments
- Bronchodilators:
These medications relax the airway muscles, improving airflow and alleviating symptoms in conditions like asthma and COPD. Short-acting and long-acting formulations are available based on clinical needs. - Corticosteroids:
Inhaled, oral, or intravenous corticosteroids reduce airway inflammation and are critical in managing acute asthma exacerbations, COPD flare-ups, and certain interstitial lung diseases. - Antibiotics and Antivirals:
Targeted antibiotic or antiviral therapies are employed to treat lung infections such as pneumonia or tuberculosis. Early intervention is essential to prevent complications. - Anti-fibrotic Agents:
For patients with pulmonary fibrosis, medications like pirfenidone and nintedanib slow disease progression and improve quality of life. - Immunomodulators:
In conditions like severe asthma or autoimmune lung diseases, immunomodulatory drugs help to regulate the immune response and reduce tissue damage.
Interventional and Surgical Procedures
- Percutaneous Coronary Intervention (PCI):
Not directly for lung disease but critical for patients with comorbid cardiovascular conditions that impact pulmonary function. - Bronchoscopy and Therapeutic Procedures:
Bronchoscopic interventions, including stent placement, tumor ablation, and foreign body removal, address airway obstructions and other intrathoracic issues. - Lung Volume Reduction Surgery (LVRS):
For patients with advanced emphysema, this surgery removes diseased lung tissue, allowing healthier lung areas to function more efficiently. - Lung Transplantation:
In end-stage lung disease, a lung transplant can significantly improve survival and quality of life. This option is considered when all other treatments have failed.
Emerging Therapies
- Targeted Therapies and Immunotherapy:
Novel drugs targeting specific molecular pathways in lung cancer cells or inflammatory pathways in chronic lung diseases offer personalized treatment options. - Stem Cell and Regenerative Medicine:
Research is ongoing into using stem cells to repair or regenerate damaged lung tissue, offering potential future treatments for conditions like pulmonary fibrosis. - Gene Therapy:
Experimental gene therapies aim to correct genetic mutations that cause certain lung diseases, such as cystic fibrosis, opening new avenues for treatment.
Supplements for Supporting Lung Health
Nutritional supplementation can play a supportive role in maintaining lung function, reducing inflammation, and protecting against oxidative stress.
Key Supplements
- Omega-3 Fatty Acids:
Found in fish oil, these essential fats have potent anti-inflammatory effects that help reduce lung inflammation and improve airway function. - N-Acetylcysteine (NAC):
NAC boosts glutathione production, an important antioxidant that protects lung tissue from oxidative damage, particularly in chronic bronchitis and COPD. - Vitamin D:
Adequate vitamin D levels support immune function and may reduce the risk of respiratory infections and asthma exacerbations. - Magnesium:
Magnesium relaxes bronchial muscles and may improve symptoms in asthmatic patients by promoting airway dilation. - Quercetin:
A natural flavonoid with anti-inflammatory and antioxidant properties, quercetin can help alleviate allergic responses and support overall lung health. - Curcumin:
Derived from turmeric, curcumin’s anti-inflammatory effects can reduce pulmonary inflammation and improve respiratory function. - Eucalyptus Oil:
Used in inhalation therapies, eucalyptus oil acts as a decongestant and can help clear the airways by reducing mucus viscosity. - Zinc:
Zinc plays a crucial role in immune function and may help shorten the duration of respiratory infections.
Lifestyle Practices for Lung Health
Adopting healthy lifestyle habits is key to preserving lung function and preventing respiratory diseases. The following best practices can help protect and enhance your lung health.
Avoid Harmful Exposures
- Quit Smoking:
Smoking is the leading cause of chronic lung disease. Quitting smoking and avoiding secondhand smoke are vital for lung recovery and prevention. - Limit Pollutant Exposure:
Reduce exposure to air pollutants and allergens by using air purifiers, staying indoors on high pollution days, and wearing protective masks when necessary.
Dietary and Hydration Strategies
- Balanced Diet:
Consume a nutrient-dense diet rich in fruits, vegetables, whole grains, and lean proteins. These foods provide antioxidants and vitamins that protect lung tissue. - Stay Hydrated:
Adequate water intake helps maintain thin mucus secretions, facilitating clearance of irritants and pathogens from the airways.
Physical Activity
- Regular Exercise:
Aerobic exercises such as walking, cycling, and swimming improve lung capacity, enhance circulation, and strengthen respiratory muscles. - Breathing Exercises:
Techniques such as diaphragmatic breathing and pursed-lip breathing can help increase lung efficiency and reduce stress.
Stress Management and Mental Health
- Manage Stress:
Chronic stress can negatively impact lung health by triggering inflammatory responses. Practices such as mindfulness, yoga, and meditation help reduce stress levels. - Adequate Sleep:
Good quality sleep is essential for overall recovery and immune function, which supports lung health.
Routine Medical Care
- Regular Check-Ups:
Regular visits to healthcare providers for lung function tests and screenings can help detect issues early and facilitate prompt treatment. - Vaccinations:
Staying updated on vaccinations, such as those for influenza and pneumonia, reduces the risk of respiratory infections.
Trusted Resources & Further Reading
For those seeking to deepen their understanding of lung health or manage respiratory conditions, the following resources provide comprehensive and reliable information.
Recommended Books
- “The Oxygen Advantage” by Patrick McKeown:
This book explores techniques for optimizing breathing and improving overall respiratory efficiency. - “Breathe: The New Science of a Lost Art” by James Nestor:
A fascinating look at the mechanics of breathing, its impact on health, and strategies to improve lung function. - “Lung Health for Everyone” by Barry D. Jordan:
Provides practical advice on preventing and managing respiratory conditions, with insights into lifestyle modifications and treatment options.
Academic Journals
- American Journal of Respiratory and Critical Care Medicine:
Publishes cutting-edge research on respiratory diseases, treatments, and clinical studies. - Chest:
A leading journal in pulmonary medicine, offering research articles, reviews, and clinical guidelines on lung health and respiratory care.
Mobile Apps
- MyCOPD:
Designed to help individuals with chronic obstructive pulmonary disease manage their symptoms through educational resources, exercise programs, and medication reminders. - Breathe2Relax:
Offers guided breathing exercises that reduce stress and improve lung function, especially useful for individuals with respiratory conditions. - QuitNow!:
A support app for those looking to quit smoking, offering motivational tools and progress tracking to improve lung health.
Frequently Asked Questions About the Lungs
What is the primary function of the lungs?
The lungs are essential for gas exchange, providing oxygen to the blood and removing carbon dioxide. They also play a role in thermoregulation, immune defense, and metabolic processes such as the conversion of angiotensin I to angiotensin II.
How do the lungs facilitate breathing?
Breathing is achieved by the rhythmic contraction and relaxation of the diaphragm and intercostal muscles, which increase and decrease the thoracic cavity volume. This change in volume creates pressure differences that allow air to flow into and out of the lungs.
What are common lung conditions?
Common lung disorders include asthma, chronic obstructive pulmonary disease (COPD), pneumonia, pulmonary fibrosis, lung cancer, tuberculosis, and interstitial lung disease. Each condition affects lung function in different ways and requires tailored management strategies.
How is lung function evaluated?
Lung function is evaluated through pulmonary function tests such as spirometry and plethysmography, imaging studies like chest X-rays and CT scans, and specialized procedures such as bronchoscopy and lung biopsy. These tests help diagnose and monitor lung diseases.
What lifestyle changes support lung health?
Maintaining lung health involves quitting smoking, avoiding pollutants, engaging in regular exercise, eating a balanced diet rich in antioxidants, staying hydrated, managing stress, and receiving regular health check-ups and vaccinations.
Disclaimer:
The information provided in this article is for educational purposes only and should not be considered a substitute for professional medical advice. Always consult a healthcare provider for personalized guidance.
If you found this guide helpful, please share it on Facebook, X (formerly Twitter), or your preferred social media platform to help spread awareness about lung health and overall wellness.