Lymph nodes are small, bean-shaped structures that play a critical role in the body’s immune defense and fluid regulation. Acting as filtration centers, they trap pathogens, facilitate immune cell communication, and help maintain tissue fluid balance. This guide will explore the intricate anatomy, key functions, common disorders, diagnostic methods, treatment options, and healthy lifestyle tips related to lymph nodes. Whether you are seeking in-depth scientific knowledge or practical health advice, this comprehensive resource provides expertly researched insights into one of the most essential components of the lymphatic system.
Table of Contents
- Structural Blueprint of Lymphatic Nodes
- Constituent Immune Cells
- Lymph Fluid Transport Pathways
- Regional Distribution & Functions
- Physiological Roles and Mechanisms
- Overview of Lymphatic Disorders
- Diagnostic Techniques for Lymph Nodes
- Therapeutic Strategies for Lymphatic Conditions
- Evidence-Based Supplements
- Lifestyle and Preventive Measures
- Reliable References and Tools
- Frequently Asked Questions
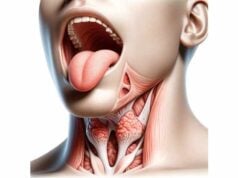
Structural Blueprint of Lymphatic Nodes
The lymph node is a marvel of natural engineering, featuring an intricate design that facilitates its numerous roles in immunity and fluid regulation. Each node is encapsulated by a dense, fibrous covering known as the capsule. This tough outer layer not only offers mechanical support but also shields the delicate internal structures from external pressures. Extending inward, the trabeculae act as supportive beams, subdividing the node and creating compartments that optimize immune cell interactions.
Within these compartments lies the cortex, an outer region densely populated with lymphocytes. The cortex is subdivided into areas where B lymphocytes aggregate in organized follicles, often developing germinal centers during active immune responses. Just beneath this lies the paracortex—a region rich in T lymphocytes and dendritic cells that orchestrate the body’s cellular immune responses. At the core of the lymph node, the medulla houses medullary cords and sinuses, providing a final checkpoint where lymph is further filtered and immune cells may engage with pathogens before the fluid exits via specialized channels.
Over the decades, advanced histological studies have illustrated how this complex architecture underpins the node’s filtering and immunological functions. The dynamic interplay between structural elements such as the capsule, trabeculae, and internal subdivisions ensures that every drop of lymph fluid is scrutinized for potential threats. In essence, the structural blueprint of lymph nodes is optimized to support a rapid and effective immune response while maintaining the homeostasis of body fluids.
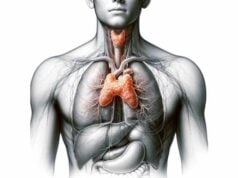
Constituent Immune Cells
Within the sanctuary of each lymph node resides a diverse community of immune cells, each playing a specialized role in protecting the body against infections and other foreign invaders. Among the principal residents are the lymphocytes, divided into B cells and T cells. B cells, which mature in the bone marrow, are responsible for producing antibodies that neutralize pathogens. They often cluster within the follicles of the cortex, where they can rapidly proliferate during an infection.
T cells, which develop in the thymus, predominantly reside in the paracortex. These cells are key players in cell-mediated immunity, identifying and destroying cells that have been compromised by infection or malignancy. Among T cells, CD4+ helper T cells facilitate the activation of other immune cells, while CD8+ cytotoxic T cells directly attack infected or cancerous cells.
Complementing these lymphocytes are macrophages—large, versatile cells that engulf and digest cellular debris, pathogens, and dead cells. Dendritic cells, also present in the lymph node, capture antigens from invading organisms and present them to T cells, kick-starting a targeted immune response. Additionally, plasma cells, which are differentiated forms of B cells, continuously produce antibodies that circulate through the body to combat recurring threats.
This cellular diversity is critical to the node’s ability to function as both an immunological command center and a filtration hub. The synergistic interaction among these cells ensures that any sign of infection or abnormality is promptly addressed, making the lymph node an indispensable part of the body’s defense system.
Lymph Fluid Transport Pathways
Lymph nodes are integral waypoints in the body’s extensive lymphatic network, which is responsible for transporting lymph—a clear fluid rich in immune cells—throughout the tissues. The journey begins at the periphery, where afferent lymphatic vessels collect interstitial fluid laden with cellular debris, pathogens, and antigens from surrounding tissues. These vessels direct the lymph into the lymph node’s subcapsular sinus, where the fluid’s movement slows, allowing immune cells to inspect and process its contents.
As the fluid advances, it traverses the trabecular sinuses—channels formed by the inward projections of the capsule. These sinuses further direct the lymph toward the medullary region of the node, a critical area for the final filtration process. In the medullary sinuses, the lymph interacts with a high concentration of immune cells such as macrophages and plasma cells, which work diligently to capture and eliminate foreign particles.
Once filtered, the cleansed lymph exits the node via efferent lymphatic vessels, which are located at the hilum or concave surface of the node. This exit pathway ensures that the purified lymph is efficiently returned to the bloodstream, where it can continue to circulate and support systemic immunity. This well-orchestrated flow of lymph not only sustains the body’s fluid balance but also plays a pivotal role in the rapid detection and neutralization of pathogens.
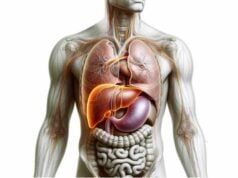
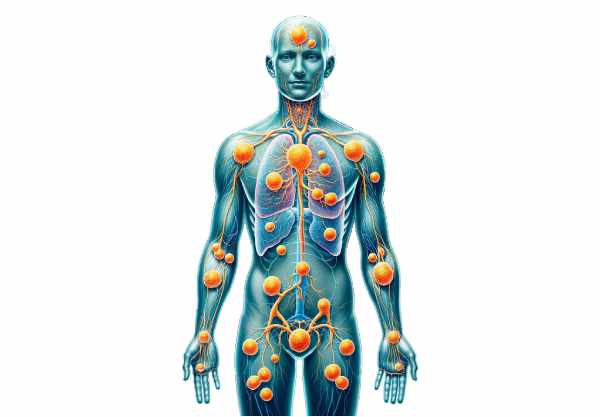
Regional Distribution & Functions
Lymph nodes are distributed throughout the body in strategic clusters, each performing specialized roles based on their location. In the head and neck region, cervical lymph nodes serve as the first line of defense by filtering lymph from the brain, face, and upper respiratory tract. Their ability to capture airborne and ingested pathogens is critical in preventing the spread of infections to vital organs.
Moving to the upper body, axillary lymph nodes situated in the armpits drain lymph from the arms, upper chest, and breast tissue. Their role becomes particularly significant in the context of breast cancer, where the presence of cancer cells in these nodes can influence treatment decisions. In the lower body, inguinal lymph nodes, located in the groin, filter lymph from the legs, lower abdomen, and external genital regions, ensuring that pathogens from these areas are promptly identified and neutralized.
Deep within the abdominal cavity, mesenteric lymph nodes collect lymph from the intestines, contributing to immune surveillance in the gastrointestinal tract. This regional specialization not only highlights the functional diversity of lymph nodes but also underscores their collective importance in maintaining overall health by ensuring that every region of the body is equipped with its own localized defense system.
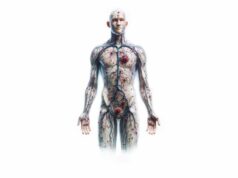
Physiological Roles and Mechanisms
Lymph nodes are not mere passive filters; they are dynamic entities that play multiple, interrelated roles in maintaining bodily health. One of their primary functions is the physical filtration of lymph. As lymph passes through the nodes, the slow flow created by the intricate network of trabeculae and sinuses allows immune cells ample time to interact with and neutralize any foreign substances present.
In addition to this mechanical filtering, lymph nodes serve as critical sites for immunosurveillance. Antigen-presenting cells, such as dendritic cells and macrophages, capture pathogens and display fragments of these invaders to T lymphocytes. This antigen presentation is pivotal for initiating a robust adaptive immune response, which includes the activation and proliferation of both T and B cells.
Moreover, lymph nodes contribute significantly to fluid homeostasis by collecting excess interstitial fluid and returning it to the circulatory system, thereby preventing edema. They also play a role in nutrient transport, particularly in the handling of dietary lipids. Chylomicrons, which are lipid-rich particles absorbed from the intestines, traverse the lymphatic system and are partially processed within lymph nodes before entering the bloodstream.
Beyond these functions, lymph nodes act as reservoirs for immune cells, facilitating constant cell exchange between the bloodstream and lymphatic system. This continuous circulation ensures that the immune system remains vigilant and capable of mounting a rapid response to any emerging threats, including cancer cells and senescent cellular debris.
Overview of Lymphatic Disorders
A spectrum of disorders can affect the lymph nodes, ranging from benign inflammatory reactions to malignant cancers. One common condition is lymphadenopathy, which is characterized by the enlargement of lymph nodes. This enlargement may result from various causes such as bacterial, viral, or parasitic infections, as well as autoimmune reactions and malignancies.
Lymphadenitis, an inflammation of the lymph nodes, is often associated with acute infections. It typically presents as tender, swollen nodes that may be accompanied by systemic symptoms like fever. Chronic lymphadenitis, on the other hand, can be a consequence of long-standing infections such as tuberculosis, where nodes become persistently enlarged yet less acutely painful.
Lymphedema is another significant disorder, marked by the abnormal accumulation of lymph fluid that leads to swelling, usually in the limbs. This condition can be primary—due to congenital malformations—or secondary, resulting from surgical removal of lymph nodes, radiation therapy, or injury. Additionally, lymphomas, including both Hodgkin and non-Hodgkin variants, represent malignant transformations of lymphatic tissue, often signaled by painless lymph node enlargement, unexplained weight loss, and systemic symptoms.
Rare conditions such as Castleman disease and sarcoidosis further illustrate the diverse pathology that can affect lymph nodes. In Castleman disease, abnormal cell proliferation leads to enlarged nodes, whereas sarcoidosis is marked by granuloma formation that can impact multiple organs including the lymphatic system. Metastatic lymph nodes occur when cancer from other parts of the body spreads to these nodes, complicating the clinical picture and often necessitating more aggressive treatment strategies.
Diagnostic Techniques for Lymph Nodes
Timely and accurate diagnosis of lymph node abnormalities is crucial for effective treatment planning. The diagnostic journey typically begins with a thorough physical examination, where clinicians palpate accessible nodes in areas such as the neck, armpits, and groin to assess for changes in size, tenderness, or consistency. A physical exam can offer initial clues, but further diagnostic testing is usually required to pinpoint the underlying cause.
Imaging techniques provide a non-invasive window into the internal structure of lymph nodes. Ultrasound, for example, uses high-frequency sound waves to produce images of superficial nodes, helping to distinguish between cystic and solid masses. More advanced modalities such as computerized tomography (CT) scans and magnetic resonance imaging (MRI) offer detailed cross-sectional and soft tissue images, respectively. Positron emission tomography (PET) scans combine metabolic and anatomical data to detect malignancies with high sensitivity, especially when used in conjunction with CT.
Biopsy procedures are the gold standard for definitive diagnosis. Fine needle aspiration (FNA) involves using a thin needle to extract a small sample of cells, which can then be examined microscopically. In cases where more tissue is needed, a core needle biopsy or an excisional biopsy—where the entire node or a significant portion is surgically removed—may be performed. Laboratory tests, including complete blood counts (CBC), serological assays, and molecular techniques like polymerase chain reaction (PCR) and fluorescence in situ hybridization (FISH), further complement imaging and histopathology by providing insights into infection markers, immune function, and genetic abnormalities.
Recent advances have introduced techniques such as sentinel lymph node biopsy, next-generation sequencing (NGS), and immunohistochemistry (IHC), which refine diagnostic precision and enable personalized treatment strategies based on the molecular characteristics of lymph node tissue.
Therapeutic Strategies for Lymphatic Conditions
Treatment strategies for lymph node disorders are as diverse as the conditions themselves, ranging from conservative management of infections to aggressive interventions for malignancies. For infectious causes of lymphadenitis, antibiotic therapy remains the cornerstone of treatment. Broad-spectrum antibiotics are frequently used to target the most common bacterial pathogens, while supportive care—including rest, hydration, and analgesics—helps manage symptoms during viral infections. In cases where abscess formation occurs, surgical drainage may be necessary to remove pus and alleviate discomfort.
Autoimmune-related lymph node enlargement is managed with immunomodulatory agents. Corticosteroids, for instance, are effective in reducing inflammation, while disease-modifying antirheumatic drugs (DMARDs) and biologic agents target specific immune pathways to control chronic autoimmune activity. When malignancy is the culprit—such as in various forms of lymphoma—treatment often involves a multimodal approach. Chemotherapy regimens like CHOP and ABVD are designed to eliminate rapidly dividing cancer cells, while radiation therapy may be used to target localized disease. Advances in targeted therapies and immunotherapies, including immune checkpoint inhibitors and CAR T-cell treatments, are revolutionizing the management of refractory or relapsed cancers. In select cases, hematopoietic stem cell transplantation (HSCT) offers a pathway to replace diseased marrow with healthy cells, providing a potential cure for otherwise intractable conditions.
For lymphedema, both non-surgical and surgical interventions are available. Compressive therapy using specialized garments, manual lymphatic drainage (MLD) massage techniques, and tailored physical exercise programs help improve lymphatic flow and reduce swelling. In severe cases, surgical procedures such as lymphaticovenous anastomosis (LVA) or vascularized lymph node transfer (VLNT) may be indicated to restore lymphatic drainage and alleviate symptoms.
Evidence-Based Supplements
Optimizing lymph node health can be complemented by nutritional strategies that support the immune system. A variety of vitamins, minerals, herbal extracts, and other dietary supplements have been scientifically linked to improved immune function and lymphatic circulation. For instance, vitamin C is a potent antioxidant that enhances the function of white blood cells, thereby supporting both innate and adaptive immunity. Similarly, vitamin D plays a crucial role in modulating immune responses and may lower the risk of infections, while zinc is essential for cellular signaling and immune cell development.
Herbal supplements such as echinacea and astragalus have long been used in traditional medicine to boost immune function. Echinacea, available in teas, extracts, or capsules, may help reduce the severity of common colds, whereas astragalus is reputed for its immune-enhancing properties and is commonly used in Eastern medicine practices. Antioxidants like green tea extract and curcumin—derived from turmeric—offer additional support by reducing oxidative stress and inflammation. Probiotics, which foster a balanced gut microbiome, indirectly boost systemic immunity, while omega-3 fatty acids from fish oil provide anti-inflammatory benefits that help maintain overall lymphatic health.
Integrating these evidence-based supplements into a balanced diet can reinforce the body’s natural defenses, promote optimal lymphatic function, and enhance the overall health of the immune system.
Lifestyle and Preventive Measures
A proactive approach to maintaining lymph node health is essential for overall well-being. A balanced diet rich in fruits, vegetables, lean proteins, and whole grains forms the foundation of a robust immune system. Adequate hydration ensures that lymphatic fluid flows efficiently, while regular physical activity promotes circulation and aids in the prevention of fluid accumulation.
Personal hygiene practices, such as regular handwashing and proper wound care, help minimize the risk of infections that can compromise lymph node function. Equally important is the management of stress, which has a profound impact on immune competence. Techniques such as meditation, yoga, and deep breathing exercises can mitigate chronic stress and bolster immune resilience. Ensuring sufficient sleep—typically 7 to 9 hours per night—is vital for cellular repair and immune regulation.
Avoiding harmful substances, such as tobacco and excessive alcohol, further protects the lymphatic system. Maintaining a healthy weight through balanced nutrition and exercise prevents obesity-related stress on lymphatic circulation. Routine medical check-ups and staying current with vaccinations provide additional safeguards by facilitating early detection and management of potential lymph node abnormalities. Together, these lifestyle strategies empower individuals to maintain optimal lymph node function and enhance their overall health.
Reliable References and Tools
For readers interested in delving deeper into lymph node science and related health strategies, a number of trusted resources are available. Scholarly books such as “The Lymphatic System: A Comprehensive Review” by John R. Hesselgesser provide an in-depth analysis of lymphatic anatomy, physiology, and pathology. Complementary works like “Immunity: The Science of Staying Well” by Jenna Macciochi offer practical insights into supporting immune health, while specialized texts such as “Lymphatic Yoga: Book I” by Edely L. Wallace focus on exercises designed to improve lymphatic flow.
Academic journals, including The Journal of Immunology and Lymphology, publish cutting-edge research that further elucidates the complexities of the lymphatic system and its disorders. In the digital age, mobile applications like “My Lymph Node Tracker” and “ImmunoApp” empower individuals to monitor their lymph node health, track symptoms, and stay informed about the latest medical advances. These resources collectively serve as invaluable tools for both healthcare professionals and laypersons seeking to understand and optimize lymphatic function.
Frequently Asked Questions
What roles do lymph nodes play in immune defense?
Lymph nodes act as filtration centers that trap pathogens, facilitate antigen presentation, and enable the activation of lymphocytes. This coordinated effort ensures rapid immune responses and helps prevent the spread of infections throughout the body.
How are lymph nodes connected to the circulatory system?
Lymph nodes are part of the lymphatic system, which collects excess interstitial fluid, filters it, and returns it to the bloodstream. This connection is essential for maintaining fluid balance and distributing immune cells systemically.
What symptoms might indicate a lymph node disorder?
Common symptoms include swollen or tender lymph nodes, unexplained weight loss, fever, and night sweats. However, these signs require professional evaluation to determine if they result from infection, autoimmune disease, or malignancy.
How can imaging tests aid in diagnosing lymph node abnormalities?
Imaging techniques such as ultrasound, CT scans, MRI, and PET scans provide detailed views of lymph nodes. These modalities help determine the size, structure, and metabolic activity of nodes, which are crucial in distinguishing between benign and malignant conditions.
Are lifestyle changes effective in supporting lymph node health?
Yes, adopting a balanced diet, staying hydrated, exercising regularly, managing stress, and maintaining proper hygiene all contribute to the optimal functioning of the lymphatic system and overall immune health.
Disclaimer: The information provided in this article is for educational purposes only and is not intended as a substitute for professional medical advice. Always consult a qualified healthcare provider regarding any medical concerns.
If you found this article helpful, please share it on Facebook, X (formerly Twitter), or your favorite social media platform. Your support can help spread valuable health insights and encourage others to learn more about maintaining optimal lymph node health.