What is malignant melanoma of the eyelid?
Malignant melanoma of the eyelid is a rare but aggressive type of skin cancer that develops from melanocytes, pigment-producing cells found in the skin of the eyelid. This condition has the potential to spread (metastasize) to other parts of the body, making it life-threatening. Early detection and treatment are critical for improving outcomes and avoiding serious complications. Recognizing the symptoms and risk factors associated with malignant melanoma of the eyelid can lead to early medical intervention and improved outcomes.
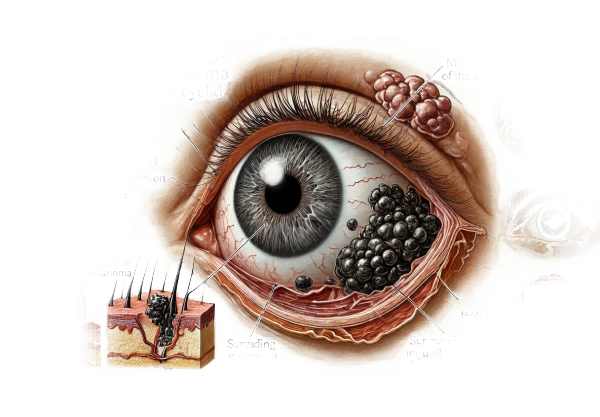
Detailed Examination of Malignant Melanoma of the Eyelid
Malignant melanoma of the eyelid is a serious ocular condition that necessitates a thorough understanding of its pathophysiology, risk factors, clinical manifestation, and potential complications.
Pathophysiology
Melanoma develops from melanocytes, cells that produce melanin, the pigment that gives skin its color. When these cells undergo malignant transformation, they begin to grow uncontrollably, resulting in a tumor. The exact cause of this transformation is unknown, but it is believed to be a combination of genetic and environmental factors.
Risk Factors
Several risk factors raise the possibility of developing malignant melanoma of the eyelid:
- Ultraviolet (UV) Radiation: Prolonged exposure to UV radiation from the sun or tanning beds poses a significant risk. UV radiation can damage the DNA in skin cells, resulting in mutations that cause melanoma.
- Fair Skin: People with fair skin, light hair, and light eyes are more vulnerable due to lower levels of melanin, which provides some protection against UV radiation.
- Family History: A family history of melanoma or other skin cancers raises the risk, suggesting a genetic predisposition.
- Multiple Moles: Having a large number of moles or atypical moles (dysplastic nevi) raises the possibility of developing melanoma.
- Age: Melanoma becomes more common as people get older, with the majority of cases occurring in people over 50.
- Immune Suppression: People with weakened immune systems, such as those who have had organ transplants or are taking immunosuppressive medications, are at a greater risk.
Clinical Presentation
Malignant melanoma of the eyelid can cause a variety of signs and symptoms, which differ depending on the stage and location of the tumor. Common clinical characteristics include:
- Pigmented Lesion: The most recognizable feature is a pigmented lesion on the eyelid. This lesion could appear as a new spot or an existing mole that changes size, shape, or color. It is frequently asymmetrical, with irregular borders and varying shades of brown, black, blue, and red.
- Ulceration and Bleeding: Advanced melanomas can ulcerate and bleed, resulting in crusting and discomfort.
- Nodular Growth: A firm, raised nodule on the eyelid may indicate that the melanoma has spread deeper.
- Change in Sensation: Patients may feel itching, tenderness, or pain in the affected area.
- Loss of Eyelashes: The tumor may cause madarosis (loss of eyelashes) near the lesion.
Types of Eyelid Melanoma
Melanomas are classified into several types based on their appearance and growth patterns:
- Superficial Spreading Melanoma: This is the most common type, with horizontal growth before reaching deeper layers of the skin.
- Nodular Melanoma: This type is more aggressive, with rapid vertical growth and a greater risk of metastasis.
- Lentigo Maligna Melanoma: Typically found in older adults, this type begins as a flat, pigmented lesion that progresses to invasive melanoma.
- Acral Lentiginous Melanoma: Although rare, this type can develop on the eyelids and is more common in people with darker skin tones.
Stages and Prognoses
The prognosis of malignant melanoma of the eyelid is determined by the stage of the disease at diagnosis. The tumor’s thickness, ulceration, and extent of spread to lymph nodes or distant organs all contribute to its staging. Melanoma is most commonly classified using the American Joint Committee on Cancer (AJCC) staging system:
- Stage 0 (In Situ): Melanoma has spread to the outermost layer of skin (epidermis) but not to deeper tissues.
- Stage I: Melanoma is skin-confined but may be thicker than stage 0. It has not spread to lymph nodes or other locations.
- Stage II: The tumor is thicker and may be ulcerated. There has still been no spread to lymph nodes or distant sites.
- Stage III: Melanoma has spread to local lymph nodes but not to distant organs.
- Stage IV: Melanoma has spread to distant organs or other areas of the body.
Complications
Malignant melanoma of the eyelid can cause a number of serious complications if not treated promptly:
- Metastasis: The most serious risk is the spread of melanoma to other parts of the body, such as the lymph nodes, liver, lungs, brain, and bones.
- Vision Loss: Tumor growth can damage the structures of the eye, resulting in vision impairment or loss.
- Disfigurement: Surgical removal of the tumor may cause significant cosmetic and functional defects that necessitate reconstructive surgery.
- Local Recurrence: Even after treatment, melanoma can return locally, necessitating ongoing monitoring and management.
Diagnostic methods
Accurate and timely detection of malignant melanoma of the eyelid is critical for effective treatment and better patient outcomes. Several diagnostic methods are used to detect and assess this condition.
Clinical Examination
- Visual Inspection: The first step is to conduct a thorough visual inspection of the eyelid and its surroundings. Dermatologists and ophthalmologists look for specific signs such as asymmetrical pigmented lesions, changes in existing moles and nodules, and any ulceration or bleeding.
- Dermatoscopy: This non-invasive technique uses a dermatoscope to magnify and illuminate the skin, allowing for a more in-depth examination of pigmented lesions. Dermatoscopy assists in identifying specific patterns and structures within the lesion that are indicative of melanoma.
Imaging Techniques
- High-Frequency Ultrasound: High-frequency ultrasound can produce detailed images of the eyelid structures, allowing doctors to assess the depth of tumor invasion and the involvement of nearby tissues.
- Optical Coherence Tomography (OCT): OCT is a non-invasive imaging technique for creating cross-sectional images of the skin and ocular tissues. It is useful for determining the thickness and size of melanoma.
- Magnetic Resonance Imaging (MRI): MRI is used to determine the extent of tumor spread to nearby structures, such as the orbit or brain, and is especially useful for surgical planning.
Biopsy
A biopsy is necessary to confirm the diagnosis of malignant melanoma. There are several kinds of biopsy techniques used:
- Excisional Biopsy: This procedure involves completely removing the lesion as well as a margin of normal tissue. It is the preferred method for small, easily accessible lesions.
- Incisional Biopsy: This procedure involves removing a portion of the lesion and is used when the lesion is large or in a location that prevents complete removal.
- Fine-Needle Aspiration (FNA): FNA can be used to sample suspicious lymph nodes or deeper tissues to detect metastasis.
Histopathologic Examination
A pathology laboratory receives the biopsy sample for histopathological examination. The pathologist examines the tissue under a microscope to confirm the presence of melanoma cells and evaluates characteristics such as tumor thickness (Breslow thickness), ulceration, and mitotic rate. These factors are critical for staging melanoma and making treatment decisions.
Molecular and Genetic Testing
Advances in molecular and genetic testing have improved the diagnostic capabilities for melanoma.
- Immunohistochemistry (IHC): IHC employs antibodies to identify specific proteins expressed by melanoma cells. This helps to distinguish melanoma from other types of skin cancer.
- Fluorescence In Situ Hybridization (FISH): FISH detects genetic abnormalities associated with melanoma, such as gene amplifications or deletions.
- Next-Generation Sequencing (NGS): NGS can detect specific genetic mutations and changes in melanoma cells, providing useful information for targeted therapies and personalized treatment plans.
Sentinel Lymph Node Biopsy
Sentinel lymph node biopsy is a surgical procedure that determines whether melanoma has spread to the lymph nodes. A radioactive tracer and dye are injected near the tumor site to identify sentinel lymph nodes, which are the first to receive tumor drainage. The nodes are then surgically removed and examined for melanoma cells. This procedure is critical for accurate staging and determining disease severity.
Malignant Melanoma of the Eyelid Treatment
The treatment of malignant melanoma of the eyelid takes a multidisciplinary approach, with the goal of removing the tumor, preventing metastasis, and preserving the eyelid’s function and appearance. The treatment plan is tailored to the patient’s individual needs, taking into account tumor size, location, and stage.
Surgical Treatment
- Wide Local Excision: The primary treatment for malignant melanoma of the eyelid is surgical removal with clear margins. This entails removing the tumor as well as a margin of healthy tissue in order to eliminate all cancerous cells. The size and depth of the tumor determine the extent of tissue removal.
- Sentinel Lymph Node Biopsy: If there is any concern about lymph node involvement, a sentinel lymph node biopsy may be performed alongside the excision. This helps determine whether the cancer has spread to the lymph nodes, which guides future treatment decisions.
- Reconstructive Surgery: Due to the critical functional and aesthetic role of the eyelids, reconstructive surgery is frequently required following tumor removal. Skin grafts, local flaps, and complex reconstruction can all be used to restore the appearance and function of the eyelid.
Radiation Therapy
Radiation therapy can be used as an adjunct to surgery, especially when complete surgical excision is difficult or the tumor has high-risk characteristics. It can help to lower the risk of local recurrence and manage metastatic disease.
Chemotherapy
Chemotherapy is not typically the first-line treatment for localized malignant melanoma of the eyelid, but it may be considered in cases of advanced or metastatic disease. Systemic chemotherapy can help control the spread of cancer throughout the body.
Targeted Therapy
- BRAF Inhibitors: Some melanoma cells contain specific genetic mutations, such as BRAF mutations. Targeted therapies, such as BRAF inhibitors (vemurafenib, dabrafenib), can effectively treat melanomas with these mutations by blocking the pathways that promote cancer cell growth.
- MEK Inhibitors: Often used in conjunction with BRAF inhibitors, MEK inhibitors (e.g., trametinib) target a different part of the same pathway, providing a synergistic effect that can improve outcomes in BRAF-mutated melanoma patients.
Immunotherapy
- Checkpoint Inhibitors: Immunotherapy has transformed the treatment of melanoma, particularly of the eyelid. Checkpoint inhibitors (such as pembrolizumab and nivolumab) enhance the immune system’s ability to recognize and attack cancer cells. These drugs inhibit proteins that keep immune cells from attacking melanoma cells.
- Adoptive Cell Transfer: This experimental therapy involves removing a patient’s immune cells, modifying them to improve their ability to fight cancer, and reintroducing them back into the patient. While still in clinical trials, this approach has shown promise in treating advanced melanoma.
Emerging Therapies
- Oncolytic Virus Therapy: This novel approach employs genetically modified viruses to selectively infect and kill cancer cells while also stimulating an anti-tumor immune response. Talimogene laherparepvec (T-VEC) is an oncolytic virus therapy approved for melanoma treatment.
- Personalized Medicine: Advances in genomic profiling and personalized medicine are allowing for more individualized treatment strategies. Oncologists can identify specific mutations in a patient’s tumor and choose the most effective targeted therapies by analyzing its genetic makeup.
- Combination Therapies: Researchers are investigating the efficacy of combining different treatment modalities, such as immunotherapy and targeted therapy or radiation. These combined approaches seek to improve treatment efficacy and overcome resistance.
A combination of surgical, medical, and emerging therapies, tailored to the patient’s specific condition and genetic profile, is required for effective management of malignant melanoma of the eyelid. Continuous advances in cancer research are improving patient outcomes and survival rates in this difficult condition.
Effective Ways to Improve and Prevent Malignant Melanoma of the Eyelid
- Regular Skin Examinations: Schedule regular skin exams with a dermatologist to catch any suspicious changes early. Regular self-examinations can also help detect new or changing lesions.
- Protect Eyes from UV Radiation: To protect your eyes and eyelids from harmful ultraviolet rays, wear UV-protected sunglasses and broad-brimmed hats. Avoid tanning beds and prolonged sun exposure.
- Use Sunscreen: Apply a broad-spectrum sunscreen with an SPF of 30 or higher to all exposed skin, including your eyelids. Reapply every two hours, particularly after swimming or sweating.
- Avoid Peak Sun Hours: Limit outdoor activities from 10 a.m. to 4 p.m., when UV radiation is strongest.
- Stay Informed About Skin Changes: Be aware of the ABCDEs of melanoma (asymmetry, border irregularity, color variation, diameter greater than 6mm, and changing shape/size). Report any concerning changes to a healthcare professional as soon as possible.
- Maintain a Healthy Lifestyle: Eat a well-balanced diet high in antioxidants, vitamins, and minerals to promote overall skin health. Fruits and vegetables, as well as fish, are nutritious.
- Avoid Smoking: Smoking weakens the immune system and impairs the body’s ability to fight cancer. Quitting smoking can improve overall health and lower cancer risk.
- Genetic Counseling: If you have a family history of melanoma or other skin cancers, you should seek genetic counseling to determine your risk and discuss preventive strategies.
- Monitor Immunosuppressive Conditions: If you have a weak immune system or are taking immunosuppressive medications, consult with your doctor to monitor your skin’s health and take preventive measures.
- Educate Yourself and Others: Be aware of the risk factors and prevention strategies for melanoma. Educate family and friends to increase awareness and early detection.
Trusted Resources
Books
- “The Melanoma Handbook” by Julie A. Sosa and Charlotte Ariyan
- “Cutaneous Melanoma: Etiology and Therapy” by William H. Ward and April Armstrong
- “Melanoma: A Modern Multidisciplinary Approach” by Howard L. Kaufman
Online Resources
- American Academy of Dermatology (AAD) – aad.org
- National Cancer Institute (NCI) – cancer.gov
- Skin Cancer Foundation – skincancer.org
- American Society of Clinical Oncology (ASCO) – asco.org






