The mammary glands are not only central to nurturing newborns through lactation but also serve as a window into overall breast health. These specialized organs undergo dramatic changes during different life stages—from puberty to menopause—and are influenced by complex hormonal signals. In this guide, you will discover the detailed anatomy of the mammary glands, learn how they function to produce and deliver milk, explore common disorders and diagnostic methods, and review the most effective treatment strategies along with lifestyle practices and supplements to keep your breasts healthy and strong.
Table of Contents
- Structural Composition of Mammary Glands
- Physiology and Functional Mechanisms
- Prevalent Mammary Gland Disorders
- Diagnostic Approaches in Breast Health
- Therapeutic Modalities for Mammary Disorders
- Nutritional and Supplementary Support
- Lifestyle Strategies for Optimal Breast Health
- Reliable Resources and Tools
- Frequently Asked Questions
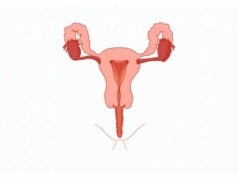
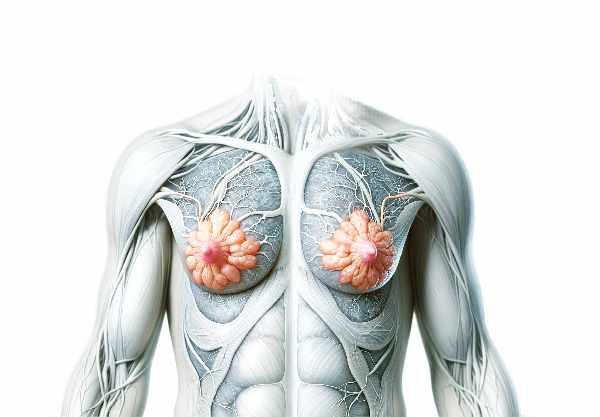
Structural Composition of Mammary Glands
The mammary glands are complex organs that comprise a variety of specialized structures working together to produce and deliver milk. Their architecture is intricately organized into lobes, lobules, ducts, and alveoli, each playing a crucial role in the overall function of the gland.
Fundamental Architecture
Mammary glands are divided into approximately 15 to 20 lobes, each resembling a cluster of grapes. Within each lobe are smaller subunits known as lobules—clusters of milk-producing tissue that contain numerous alveoli. Alveoli are tiny, sac-like structures lined by secretory epithelial cells responsible for synthesizing milk. Encircling these alveoli are myoepithelial cells, which contract to expel milk into a branching network of ducts. These ducts converge and enlarge, ultimately forming the lactiferous ducts that open at the nipple, facilitating the transfer of milk during breastfeeding.
Cellular Landscape
The tissue composition of the mammary glands includes several cell types:
- Epithelial Cells: These line the alveoli and are actively involved in the production and secretion of milk components such as proteins, lipids, and lactose.
- Myoepithelial Cells: Situated around both alveoli and ducts, these contractile cells respond to hormonal signals, playing a vital role in milk ejection.
- Stromal Cells: This supportive framework consists of connective tissue, fat cells, blood vessels, lymphatics, and nerves that collectively ensure structural integrity and nourishment of the gland.
Development and Hormonal Influences
The development of the mammary glands is a dynamic, lifelong process. It begins during embryonic life along the milk lines—linear structures where mammary tissue first appears.
- Puberty: Estrogen and progesterone drive the expansion of ductal networks and the formation of lobular structures, leading to the mature adult breast.
- Pregnancy: A surge in estrogen, progesterone, and prolactin induces further differentiation and growth, preparing the glands for milk production.
- Lactation: After childbirth, high prolactin levels stimulate milk synthesis while oxytocin triggers the contraction of myoepithelial cells, enabling the let-down reflex.
- Menopause: The decline in hormonal levels leads to the involution of glandular tissue, replaced gradually by fibrous and adipose tissue.
Microanatomy and Functional Units
At the microscopic level, the mammary gland’s primary functional unit is the terminal ductal lobular unit (TDLU). The TDLU consists of:
- Terminal Ducts: Small ducts that collect milk from lobules.
- Lobules: Clusters of alveoli where milk production occurs.
Each lobule is richly supplied by a dense capillary network that provides essential nutrients and oxygen, ensuring efficient milk production.
Vascular and Lymphatic Networks
Mammary glands are richly vascularized to meet the high metabolic demands of milk synthesis.
- Arterial Supply: Branches from the lateral thoracic and internal mammary arteries provide a robust blood supply.
- Venous Drainage: Mammary veins collect deoxygenated blood and return it to systemic circulation.
- Lymphatic System: A comprehensive network of lymphatic vessels drains excess fluid and immune cells from the gland, converging in the axillary lymph nodes. This system plays a critical role in immune surveillance and early detection of pathological changes.
Nipple and Areola Complex
The nipple and areola form the external components of the mammary glands.
- Nipple: Houses multiple openings of the lactiferous ducts and is densely innervated to enhance the sensory experience during nursing.
- Areola: This pigmented area surrounds the nipple and contains Montgomery glands, which secrete protective lubricants essential during breastfeeding.
Lifespan Modifications
Mammary glands undergo significant transformations throughout life:
- Puberty: Rapid ductal growth and initial lobular development occur under hormonal influence.
- Menstrual Cycle: Hormonal fluctuations cause cyclical changes, often resulting in transient tenderness and swelling.
- Pregnancy and Lactation: The glandular component expands and differentiates to meet the nutritional demands of the newborn.
- Menopause: With decreasing hormonal stimulation, functional tissue regresses, leading to increased deposition of fibrous and adipose tissue.
Physiology and Functional Mechanisms
The primary function of the mammary glands is lactation—the production and delivery of milk to nourish infants. This process involves an intricate interplay of cellular differentiation, hormonal regulation, and reflex actions that together create a highly efficient system.
Initiation of Milk Production: Lactogenesis
Lactogenesis is the onset of milk production, which occurs in two distinct phases:
- Lactogenesis I: Begins mid-pregnancy, when the mammary alveoli differentiate into lactocytes capable of producing colostrum. Despite early milk synthesis, high levels of progesterone inhibit full milk secretion.
- Lactogenesis II: Occurs within two to three days postpartum, following the dramatic drop in progesterone levels after placental expulsion. This phase marks the commencement of copious milk production, driven primarily by sustained high levels of prolactin.
Sustaining Milk Production: Galactopoiesis
Galactopoiesis refers to the continuous production of milk, maintained by regular emptying of the breast.
- Prolactin Role: The hormone prolactin is crucial for ongoing milk synthesis. Its secretion is reinforced by the act of nursing, establishing a positive feedback loop.
- Milk Removal: Effective milk removal through infant suckling or mechanical pumping is essential to prevent milk stasis, which in turn stimulates further milk production.
Milk Ejection Mechanism
The milk ejection reflex, commonly known as let-down, is a vital process that enables the transfer of milk from the alveoli into the ducts.
- Oxytocin Surge: When the nipple is stimulated, sensory signals trigger the release of oxytocin from the posterior pituitary gland.
- Myoepithelial Contraction: Oxytocin causes the myoepithelial cells surrounding the alveoli to contract forcefully, pushing milk into the ductal network and out through the nipple.
Composition and Nutritional Value of Breastmilk
Breastmilk is a dynamic, multifaceted fluid perfectly tailored to support the growth and development of infants. It comprises:
- Macronutrients: Carbohydrates (mainly lactose), proteins (including casein and whey), and fats that provide energy and essential fatty acids.
- Micronutrients: A range of vitamins and minerals vital for infant growth.
- Bioactive Components: Immunoglobulins (especially IgA), hormones, enzymes, and growth factors that bolster the infant’s immune system and facilitate overall development.
- Living Cells: Leukocytes and stem cells contribute to immune protection and tissue repair in the infant.
Hormonal Control and Regulation
The orchestration of lactation is regulated by a host of hormones:
- Prolactin: Produced by the anterior pituitary, it is the key hormone responsible for milk synthesis.
- Oxytocin: Secreted by the posterior pituitary, oxytocin is essential for milk ejection and helps establish the maternal-infant bonding process.
- Estrogen and Progesterone: These hormones drive mammary gland development during puberty and pregnancy. Their precipitous drop after delivery facilitates the transition to active lactation.
- Human Placental Lactogen (hPL): Secreted by the placenta, hPL supports mammary development during pregnancy, preparing the breast for lactation.
Immunological and Protective Functions
Breastmilk offers vital immunological protection to the newborn:
- Antibody Transfer: IgA antibodies present in colostrum and mature milk help protect the infant’s gastrointestinal tract from pathogens.
- Immune Cells: The inclusion of leukocytes enhances the newborn’s defense mechanisms during the early months of life.
- Bioactive Molecules: Various hormones and growth factors contribute to the maturation of the infant’s immune system.
Psychological and Emotional Impacts
Breastfeeding is not only a physical nourishment process but also a critical emotional and psychological bond between the mother and child:
- Oxytocin Effects: Known as the “love hormone,” oxytocin fosters a deep emotional connection, reduces maternal stress, and enhances overall well-being.
- Maternal Fulfillment: Many mothers report a sense of accomplishment and emotional satisfaction through the act of breastfeeding, reinforcing maternal instincts and reducing postpartum depression.
Benefits for Maternal Health
In addition to its role in infant nutrition, lactation confers several health benefits to the mother:
- Postpartum Recovery: Milk production stimulates uterine contractions, which help in returning the uterus to its pre-pregnancy size and reducing postpartum hemorrhage.
- Long-Term Protection: Epidemiological studies suggest that prolonged breastfeeding may lower the risk of breast and ovarian cancers, type 2 diabetes, and cardiovascular disease.
- Psychological Well-Being: The bonding experience of breastfeeding can enhance maternal emotional health and reduce stress.
Prevalent Mammary Gland Disorders
Despite the essential role of the mammary glands, they are vulnerable to a variety of conditions. These disorders range from benign inflammatory processes to serious malignancies and can significantly impact both physical and emotional health.
Inflammatory Conditions
Mastitis:
Mastitis is an acute inflammation of the mammary gland, most commonly observed in breastfeeding women. Often caused by a bacterial infection (frequently Staphylococcus aureus or Streptococcus species), mastitis is characterized by localized breast pain, redness, swelling, warmth, and systemic symptoms such as fever and flu-like malaise. Early intervention with antibiotics, combined with continued milk expression, is essential to manage the infection and prevent abscess formation.
Breast Abscess:
A progression from untreated mastitis, a breast abscess is a localized collection of pus within the breast tissue. Patients typically experience intense pain, fever, and a palpable lump. Diagnosis is confirmed through imaging studies, and treatment generally involves drainage—either percutaneous (needle aspiration) or surgical—followed by a course of antibiotics.
Benign Breast Conditions
Fibrocystic Breast Changes:
This condition refers to non-cancerous alterations in the breast tissue that are often linked to hormonal fluctuations during the menstrual cycle. Women may experience cyclical breast pain, lumpiness, and tenderness, which can be managed with supportive care, dietary modifications, and over-the-counter pain relievers. In more severe cases, hormonal therapies may be considered to alleviate symptoms.
Gynecomastia:
Although primarily observed in males, gynecomastia—the enlargement of male breast tissue—occurs due to hormonal imbalances, medication side effects, or underlying systemic conditions. Treatment is focused on addressing the underlying cause and may involve hormone therapy, medication adjustments, or, in persistent cases, surgical reduction.
Malignant Disorders
Breast Cancer:
Breast cancer remains one of the most prevalent cancers worldwide. It can manifest as a palpable lump, changes in breast shape or size, skin dimpling, nipple discharge, or pain. Diagnosis is based on a combination of clinical examination, imaging studies (mammography, ultrasound, MRI), and histopathological evaluation through biopsy. Treatment is multifaceted and may include surgery, radiation, chemotherapy, hormone therapy, and targeted therapies.
Paget’s Disease of the Breast:
A rare form of breast cancer, Paget’s disease primarily affects the skin of the nipple and areola. It often presents with eczema-like changes, such as redness, scaling, itching, and sometimes nipple discharge. Diagnosis is confirmed through a biopsy, and treatment typically involves surgical resection combined with adjuvant therapies.
Hormonal Imbalance and Secretion Disorders
Galactorrhea:
Galactorrhea is characterized by the inappropriate secretion of milk from the breast, unrelated to childbirth or nursing. Often associated with hyperprolactinemia or thyroid dysfunction, this condition may also be induced by certain medications. Management involves identifying and treating the underlying cause, which may include medication adjustments or hormonal therapies.
Nipple Discharge:
Nipple discharge can be a concerning symptom, as it may signal a range of conditions—from benign duct ectasia and intraductal papillomas to malignancies. The color and consistency of the discharge provide clues for diagnosis. Evaluation generally includes a clinical examination, imaging, and sometimes ductoscopy or biopsy to determine the underlying cause.
Duct Ectasia:
Duct ectasia involves the dilation and inflammation of the milk ducts, often resulting in nipple discharge, retraction, and occasionally discomfort or a palpable mass. Conservative management with warm compresses and analgesics is usually effective, though surgical intervention may be required for persistent cases.
Diagnostic Approaches in Breast Health
Timely and accurate diagnosis of mammary gland disorders is crucial for effective treatment. A multi-modal approach involving physical examinations, imaging techniques, biopsies, and molecular testing is often necessary to ascertain the precise nature of breast conditions.
Clinical Breast Examinations (CBE)
A thorough clinical breast examination, performed by a healthcare professional, is the first step in detecting abnormalities. During a CBE, the clinician inspects and palpates the breast tissue to identify any lumps, thickening, or irregularities. The patient’s medical history, including family history and prior breast issues, is also reviewed to assess risk factors.
Imaging Techniques
Mammography:
Mammography is the cornerstone of breast imaging and utilizes low-dose X-rays to detect early signs of breast cancer. It is employed for routine screening in asymptomatic women and for diagnostic purposes in those with symptoms. Digital mammography has further enhanced image clarity and diagnostic accuracy.
Ultrasound:
Breast ultrasound uses high-frequency sound waves to generate images of the breast’s internal structures. It is particularly useful in differentiating solid masses from fluid-filled cysts and in guiding needle biopsies, especially in women with dense breast tissue.
Magnetic Resonance Imaging (MRI):
MRI provides high-resolution images without the use of ionizing radiation. It is particularly beneficial for evaluating high-risk patients, clarifying ambiguous findings from other imaging modalities, and planning surgical interventions.
Ductography (Galactography):
This specialized imaging technique involves injecting contrast material into the milk ducts to visualize their structure. It is especially useful when evaluating nipple discharge and identifying ductal abnormalities.
Positron Emission Tomography (PET) Scan and Elastography:
PET scans assess the metabolic activity of breast tissue, often in conjunction with CT imaging, while elastography evaluates tissue stiffness—a parameter that can help differentiate benign from malignant lesions.
Biopsy Techniques
Fine Needle Aspiration (FNA) and Core Needle Biopsy:
FNA is a minimally invasive technique that extracts cells for cytological analysis, whereas core needle biopsy provides a larger tissue sample for a more comprehensive histopathological evaluation. Both techniques are essential for confirming a diagnosis when imaging findings are suspicious.
Surgical Biopsy:
In certain cases, a surgical biopsy may be performed to remove an entire lesion or a segment of breast tissue for thorough microscopic examination.
Molecular and Genetic Testing
Advancements in molecular biology have led to the development of tests that analyze the genetic profile of breast tumors. Tests such as BRCA1/BRCA2 mutation analysis, Oncotype DX, and MammaPrint help assess cancer risk, predict recurrence, and guide personalized treatment strategies.
Advanced Imaging Modalities
Emerging technologies like thermography and advanced ultrasound techniques (e.g., elastography) are being explored to provide additional functional insights into breast tissue, complementing conventional imaging modalities.
Therapeutic Modalities for Mammary Disorders
The management of mammary gland disorders is highly individualized, ranging from conservative measures for benign conditions to aggressive, multi-modal treatments for malignant diseases. Treatment decisions depend on the specific diagnosis, disease stage, patient preferences, and overall health.
Surgical Interventions
Lumpectomy and Mastectomy:
For localized breast cancer, a lumpectomy involves removing the tumor with a margin of surrounding healthy tissue, preserving most of the breast. In contrast, mastectomy entails the complete removal of the breast, often accompanied by reconstructive surgery to restore cosmetic appearance. The choice between these procedures is influenced by tumor size, location, and patient factors.
Sentinel Lymph Node Biopsy and Axillary Dissection:
Assessing the spread of cancer to regional lymph nodes is critical. Sentinel lymph node biopsy involves removing the first few nodes draining the tumor region to evaluate metastasis. If cancer is detected, a more extensive axillary lymph node dissection may be performed.
Radiation Therapy
Radiation therapy is commonly used after surgery to eradicate residual cancer cells and reduce recurrence risk. Techniques include:
- External Beam Radiation: Delivered from outside the body using high-energy rays.
- Brachytherapy: Involves placing radioactive sources directly into or near the tumor bed.
Chemotherapy and Hormone Therapy
Chemotherapy:
Administered either before (neoadjuvant) or after (adjuvant) surgery, chemotherapy uses cytotoxic drugs to target rapidly dividing cancer cells. Regimens are tailored to the cancer type and stage.
Hormone Therapy:
Hormone receptor-positive breast cancers respond to therapies that block estrogen or reduce its production. Options include:
- Tamoxifen: An estrogen receptor modulator effective in both premenopausal and postmenopausal women.
- Aromatase Inhibitors: Lower estrogen levels in postmenopausal women.
- Ovarian Suppression: Pharmacologic or surgical interventions to reduce estrogen production in premenopausal women.
Targeted and Immunotherapy
Targeted Therapy:
These treatments specifically target molecular abnormalities in cancer cells. Examples include HER2 inhibitors (e.g., trastuzumab) and CDK4/6 inhibitors, which block proteins involved in cell division.
Immunotherapy:
Emerging immunotherapeutic strategies, including checkpoint inhibitors and CAR-T cell therapy, are designed to empower the patient’s immune system to recognize and attack cancer cells more effectively.
Supportive and Palliative Care
In addition to curative treatments, supportive care is essential to manage symptoms, reduce side effects, and maintain quality of life. This includes:
- Pain Management: Through medications, physical therapy, and alternative modalities.
- Nutritional Support: To preserve strength and well-being during treatment.
- Psychosocial Support: Counseling and support groups to assist patients and families in coping with the emotional impact of breast cancer.
Emerging and Integrative Therapies
Ongoing research continues to refine breast cancer treatment:
- Genomic Medicine: Tailoring treatment based on the tumor’s genetic signature.
- Oncolytic Virus Therapy and Photodynamic Therapy: Innovative approaches currently under investigation.
- Integrative Medicine: Complementary therapies such as acupuncture, meditation, and yoga can enhance conventional treatments and improve overall quality of life.
Nutritional and Supplementary Support
Optimal mammary gland health is supported by a balanced diet and targeted nutritional supplementation. Scientific research underscores the benefits of specific vitamins, herbal extracts, enzymes, hormones, and antioxidants in maintaining breast health and reducing disease risk.
Essential Vitamins and Nutrients
Vitamin D:
Crucial for calcium absorption and bone health, vitamin D also supports cell growth regulation. Adequate levels may lower the risk of breast cancer and promote healthy mammary tissue.
Vitamin E:
As a powerful antioxidant, vitamin E helps protect breast cells from oxidative stress and may reduce the severity of mastalgia (breast pain).
Vitamin C:
Vitamin C supports immune function and tissue repair. Its antioxidant properties help neutralize free radicals, safeguarding the delicate cellular environment of the breast.
Omega-3 Fatty Acids:
Found in fish oil and flaxseed, omega-3s reduce inflammation and may decrease the risk of breast cancer, while also supporting overall cellular health.
Herbal and Natural Extracts
Turmeric (Curcumin):
Curcumin’s potent anti-inflammatory and antioxidant activities contribute to reduced inflammation in breast tissues and may lower the risk of cancerous changes.
Green Tea Extract:
Rich in catechins, green tea extract exerts anti-cancer effects by lowering oxidative stress and inhibiting tumor growth.
Flaxseed:
With its high content of lignans and omega-3 fatty acids, flaxseed helps modulate estrogen metabolism and supports hormonal balance.
Enzymatic and Hormonal Support
Bromelain and Papain:
These enzymes, derived from pineapple and papaya respectively, offer anti-inflammatory benefits that may alleviate discomfort associated with benign breast conditions.
Melatonin:
Beyond its role in sleep regulation, melatonin exhibits antioxidant properties and may contribute to a lower incidence of breast cancer by inhibiting cancer cell proliferation.
Bioidentical Hormones:
For menopausal women, bioidentical hormone replacement therapy (BHRT) can help balance estrogen and progesterone levels, easing symptoms and supporting breast health.
Antioxidants and Micronutrients
Coenzyme Q10 (CoQ10):
Essential for cellular energy production, CoQ10 also protects cells from oxidative damage, thereby supporting mammary gland function.
Selenium:
This trace mineral is vital for antioxidant enzyme function and helps mitigate oxidative stress, potentially reducing breast cancer risk.
Lifestyle Strategies for Optimal Breast Health
Maintaining mammary gland health extends beyond medical interventions. Daily lifestyle choices play a significant role in reducing risk and promoting overall breast well-being.
- Regular Self-Examinations:
Monthly self-exams can help detect early changes or abnormalities. Familiarity with your own breast tissue is key to recognizing signs that warrant professional evaluation. - Routine Screening:
Following established guidelines for clinical breast examinations and mammography is crucial, particularly for those with a family history or increased risk factors. - Balanced Diet:
Consuming a diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats provides the nutrients necessary for cellular health and hormonal balance. - Healthy Weight Maintenance:
Obesity is linked to a higher risk of breast cancer. Achieving and maintaining a healthy weight through diet and exercise is essential for lowering risk. - Regular Physical Activity:
Aim for at least 150 minutes of moderate aerobic activity each week. Exercise improves circulation, supports immune function, and helps regulate hormone levels. - Limiting Alcohol and Avoiding Smoking:
Reducing alcohol intake and avoiding tobacco can significantly decrease the risk of developing breast cancer and other systemic diseases. - Stress Management:
Chronic stress can impact hormone levels and immune function. Techniques such as meditation, yoga, and deep breathing exercises are effective ways to manage stress. - Adequate Sleep:
Quality sleep is fundamental for cellular repair and hormonal regulation. Aim for 7–9 hours of sleep per night to support overall health. - Environmental Toxin Reduction:
Minimizing exposure to endocrine disruptors found in plastics, pesticides, and certain personal care products can help protect hormonal balance and breast tissue integrity. - Breastfeeding:
For new mothers, breastfeeding not only offers significant nutritional benefits to the infant but also reduces the mother’s risk of breast cancer and supports postpartum recovery. - Staying Informed:
Keep up-to-date with the latest research on breast health and engage in regular consultations with healthcare professionals to tailor preventive measures to your needs.
Reliable Resources and Tools
For those seeking to deepen their understanding of mammary gland health, a wide array of trusted resources is available—from comprehensive books and academic journals to innovative mobile applications.
Recommended Books
- “Dr. Susan Love’s Breast Book” by Susan M. Love, MD:
An all-encompassing guide to breast health that covers anatomy, physiology, and various treatment options, this book is a vital resource for both patients and healthcare professionals. - “Breasts: The Owner’s Manual” by Kristi Funk, MD:
Offering practical, evidence-based advice on breast care and cancer prevention, this book simplifies complex concepts and provides actionable strategies for maintaining breast health. - “The Breast Cancer Prevention Diet” by Bob Arnot, MD:
This resource explores dietary interventions and lifestyle modifications aimed at reducing breast cancer risk and promoting long-term mammary health.
Scholarly Journals
- Journal of Mammary Gland Biology and Neoplasia:
This academic journal publishes cutting-edge research on mammary gland development, physiology, and pathology, making it an invaluable tool for clinicians and researchers. - Breast Cancer Research and Treatment:
Focusing on both basic science and clinical studies, this journal covers advances in breast cancer detection, treatment, and prevention strategies.
Mobile Applications
- Breast Cancer: Beyond The Shock:
An educational app offering comprehensive information on breast cancer, treatment options, and patient experiences through videos and interactive resources. - Breast Cancer Healthline:
A supportive community app that connects patients and survivors, offering guidance, symptom tracking, and access to a wealth of informational resources. - My Breast Cancer Coach:
A personalized tool designed to help patients navigate their diagnosis, treatment options, and recovery, featuring symptom tracking, treatment planning, and expert advice.
Frequently Asked Questions
What are the primary functions of the mammary glands?
The mammary glands produce and secrete milk to nourish infants. They also play roles in hormonal regulation, immune protection, and providing emotional bonding between mother and child.
How do hormonal changes affect mammary gland development?
Hormones such as estrogen, progesterone, prolactin, and oxytocin regulate the growth, differentiation, and function of mammary glands during puberty, pregnancy, lactation, and menopause.
What are common symptoms of benign breast disorders?
Symptoms can include breast pain, tenderness, lumpiness, nipple discharge, and cyclical swelling, particularly before menstruation or during hormonal fluctuations.
Which imaging techniques are most effective in detecting breast abnormalities?
Mammography is the standard screening tool, while ultrasound and MRI are used for further evaluation, especially in dense breast tissue. Biopsies provide definitive diagnoses when abnormalities are detected.
How can lifestyle choices influence breast health?
A balanced diet, regular exercise, maintaining a healthy weight, limiting alcohol, avoiding smoking, and stress management can all significantly reduce the risk of breast disorders and support overall mammary gland health.
Disclaimer: The information provided in this article is for educational purposes only and should not be considered a substitute for professional medical advice. Always consult with a qualified healthcare provider regarding any medical concerns.
If you found this article informative, please share it on Facebook, X (formerly Twitter), or your preferred social media platform. Your support helps spread valuable health insights and encourages others to learn more about maintaining optimal mammary gland health.