What is multifocal choroiditis and panuveitis (MCP)?
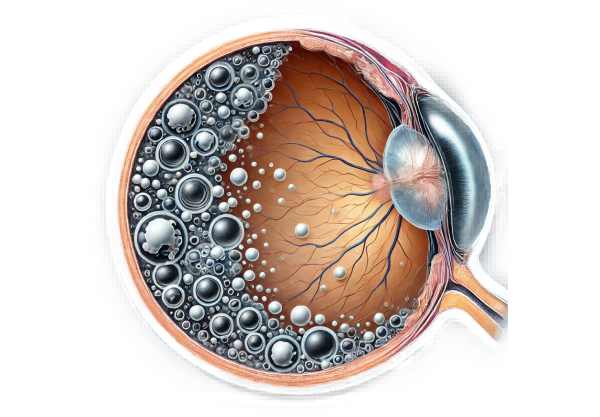
Multifocal Choroiditis and Panuveitis (MCP) is a rare, idiopathic inflammatory eye disease that affects the choroid, retina, and vitreous. MCP, which is characterized by the presence of multiple, small, yellowish-white lesions in the eye’s posterior segment, can cause significant visual impairment. It most commonly affects young to middle-aged women and can lead to complications like macular edema, choroidal neovascularization, and vitreous inflammation. Early detection and appropriate management are critical for preventing severe vision loss.
Detailed Investigation of Multifocal Choroiditis and Panuveitis (MCP)
Multifocal Choroiditis and Panuveitis (MCP) is a complex inflammatory disorder that affects several eye structures, including the choroid, retina, and vitreous. This condition belongs to a larger group of white dot syndromes, which are distinguished by the presence of numerous inflammatory lesions scattered throughout the posterior segment of the eye.
Epidemiology and Demographics
MCP is a rare disease that primarily affects young to middle-aged adults, with a strong female predilection. The disease typically develops between the ages of 20 and 50. Although the exact prevalence is unknown, it is considered a rare condition. There is no known racial or ethnic preference for MCP.
Etiology and Pathogenesis
The exact etiology of MCP is unknown, but it is thought to be an autoimmune condition. The immune system mistakenly targets ocular tissues, causing inflammation. Possible triggers include genetic predisposition, environmental factors, and infectious agents. However, no definitive causes have been identified.
The inflammatory process in MCP primarily affects the choroid, the vascular layer of the eye that supplies blood to the outer retina. The inflammation can spread to the retina and vitreous, resulting in panuveitis. The lesions seen in MCP are thought to be the result of a focal accumulation of inflammatory cells followed by tissue damage.
Clinical Presentation
Patients with MCP usually present with a variety of visual symptoms that can vary in severity. Common symptoms include:
- Blurred Vision: Blurred or decreased vision is frequently one of the first signs. This could be the result of retinal involvement or macular edema.
- Photopsia: Patients may experience light flashes, which are most commonly caused by vitreous inflammation or retinal traction.
- Floaters: The presence of floaters, caused by vitreous opacities caused by inflammatory debris, is a common complaint.
- Scotomas: Patients may experience blind spots or reduced vision in their visual field due to the location of choroidal lesions.
- Photophobia: Increased sensitivity to light is a common symptom.
Ophthalmic Examination
An ophthalmic examination of MCP patients reveals specific findings that aid in diagnosis. The key features observed during the examination include:
- Fundoscopic Examination: The fundoscopic examination reveals numerous small, yellowish-white lesions scattered throughout the retina’s posterior pole and mid-periphery. These lesions are typically less than one disc diameter in size and can vary in number and location.
- Macular Involvement: The macula may develop edema or scarring, resulting in central vision loss.
- Vitritis: Inflammation of the vitreous occurs frequently, presenting as vitreous haze or opacities.
- Choroidal Neovascularization (CNV): In some cases, MCP can cause the development of CNV, which appears as grayish or greenish lesions and can result in significant vision loss if not treated.
Complications
MCP can cause a number of complications, including vision impairment. The complications include:
- Macular Edema: Inflammation can cause fluid to accumulate in the macula, resulting in swelling and distortion of central vision.
- Choroidal Neovascularization: The formation of abnormal blood vessels beneath the retina can cause leakage, bleeding, and scarring, resulting in severe vision loss.
- Epiretinal Membrane: Inflammatory cells can form a membrane on the retina’s surface, resulting in wrinkling and distortion.
- Retinal Detachment: Although uncommon, extensive inflammation can lead to retinal detachment, a serious condition that necessitates immediate surgical intervention.
Differential Diagnosis
MCP’s differential diagnosis includes other conditions that exhibit similar symptoms and clinical findings. These conditions include the following:
- Presumed Ocular Histoplasmosis Syndrome (POHS): POHS has similarities to MCP, including the presence of chorioretinal lesions and CNV. POHS, on the other hand, is usually free of vitritis and has a history of exposure to the fungus Histoplasmacapsulatum.
- Sarcoidosis: This systemic granulomatous disease can affect the eyes, causing chorioretinal lesions and vitritis. Sarcoidosis differs from MCP by the presence of systemic symptoms and granulomas on biopsy.
- Birdshot Chorioretinopathy is characterized by multiple hypopigmented choroidal lesions that are strongly associated with the HLA-A29 antigen. Birdshot chorioretinopathy is typically characterized by bilateral involvement and a chronic course.
- Multiple Evanescent White Dot Syndrome (MEWDS) is characterized by multiple white dots in the retina and has a transient course. It frequently affects young women and is usually unilateral, with self-limiting characteristics.
- Acute Posterior Multifocal Placoid Pigment Epitheliopathy (APMPPE) is defined by multiple placoid lesions in the posterior pole. Unlike MCP, APMPPE usually resolves spontaneously without causing significant long-term visual impairment.
Pathologic Findings
A histopathological examination of affected eyes in MCP reveals characteristic findings. These include inflammatory infiltrates of lymphocytes and histiocytes in the choroid, retina, and vitreous. The choroidal lesions contain focal areas of necrosis, fibrosis, and pigmentary changes. The retinal pigment epithelium (RPE) may show atrophy and hyperplasia in the vicinity of the lesions.
Imaging Studies
Imaging studies are critical for diagnosing and monitoring MCP. The key imaging modalities are:
- Fluorescein Angiography (FA): FA visualizes the retinal vasculature and detects leakage, staining, and CNV. In MCP, FA typically exhibits early hyperfluorescence of the choroidal lesions followed by late leakage.
- Indocyanine Green Angiography (ICGA): ICGA offers detailed imaging of the choroidal circulation. It aids in identifying choroidal lesions that may not be visible on FA and detecting CNV.
- Optical Coherence Tomography (OCT): OCT can produce high-resolution cross-sectional images of the retina and choroid. It is useful in determining macular edema, CNV, and the overall structural integrity of the retina.
- Fundus Autofluorescence (FAF): FAF imaging detects RPE damage and can show the distribution and progression of choroidal lesions.
Prognosis
The prognosis for patients with MCP is highly variable, depending on the severity of the inflammation and the presence of complications. Some patients may have a relatively mild course with little vision loss, whereas others may have significant visual impairment due to complications like macular edema or CNV. Early detection and appropriate treatment are critical for maintaining vision and improving outcomes.
Diagnostic methods
Accurate and timely diagnosis of Multifocal Choroiditis and Panuveitis (MCP) is critical for successful treatment. The diagnostic process consists of clinical evaluation, imaging studies, and laboratory tests to confirm the diagnosis and rule out other possibilities.
Clinical Evaluation
The first step in diagnosing MCP is a comprehensive clinical evaluation by an ophthalmologist. This includes a thorough medical history, with emphasis on the onset and progression of symptoms, as well as any relevant systemic conditions. A thorough eye examination is performed to determine visual acuity, intraocular pressure, and inflammation in the anterior and posterior segments of the eye.
Imaging Studies
- Fluorescein Angiography (FA) is an important imaging modality for detecting MCP. It entails the intravenous injection of fluorescein dye, which highlights the retinal vascular system. FA can detect early hyperfluorescence in choroidal lesions, late leakage, and the presence of CNV.
- Indocyanine Green Angiography (ICGA): ICGA is especially useful for visualizing the choroidal circulation and identifying lesions that may not be visible with FA. It entails an intravenous injection of indocyanine green dye, which produces detailed images of the choroid.
- Optical Coherence Tomography (OCT): OCT is a non-invasive imaging technique for obtaining high-resolution cross-sectional images of the retina and choroid. It is extremely useful for assessing macular edema, CNV, and the overall structural integrity of the retina.
- Fundus Autofluorescence (FAF): FAF imaging can detect areas of RPE damage and atrophy. It provides information on the distribution and progression of choroidal lesions, which aids in disease monitoring over time.
Multifocal Choroiditis and Panuveitis (MCP) Treatment
The treatment of Multifocal Choroiditis and Panuveitis (MCP) focuses on reducing inflammation, avoiding complications, and maintaining vision. Because the condition is autoimmune, the therapeutic approach frequently includes the use of immunosuppressive and anti-inflammatory medications.
Corticosteroids
- Systemic Corticosteroids: Oral prednisone is a common first-line treatment for inflammation. The dosage and duration are determined by the severity of the condition, with a typical initial dose of 40 to 60 mg per day, tapered gradually based on response.
- Periocular Corticosteroid Injections: For patients who cannot tolerate systemic corticosteroids or who prefer localized treatment, periocular corticosteroids, such as triamcinolone acetonide, can be used.
- Intravitreal Corticosteroids: In severe cases, intravitreal corticosteroid injections, such as dexamethasone implants (Ozurdex), may be used to deliver high doses of the drug directly to the site of inflammation.
Immunosuppressive Agents
Immunosuppressive agents are frequently required for patients with chronic or severe MCP in order to achieve long-term inflammation control and minimize the side effects of prolonged corticosteroid use.
- Methotrexate: This antimetabolite drug is widely used due to its efficacy and relatively low risk profile. It is available orally or as a subcutaneous injection.
- Mycophenolate Mofetil: Mycophenolate mofetil is another commonly used immunosuppressant that inhibits lymphocyte proliferation, thereby reducing inflammation.
- Cyclosporine and Tacrolimus: These calcineurin inhibitors reduce ocular inflammation by inhibiting T-cell activation.
- Biologic Agents: Tumor necrosis factor (TNF) inhibitors like infliximab and adalimumab are becoming more popular for refractory MCP. These biologic agents target specific immune response pathways, allowing for a more targeted treatment approach.
Additional Therapies
- Antivascular Endothelial Growth Factor (anti-VEGF) Therapy: To inhibit abnormal blood vessel growth and reduce leakage, patients with choroidal neovascularization (CNV) receive intravitreal injections of anti-VEGF agents such as bevacizumab (Avastin) or ranibizumab (Lucentis).
- Photodynamic Therapy (PDT): PDT may be considered for the treatment of CNV in conjunction with MCP. This procedure entails administering a photosensitizing agent intravenously before activating the laser to selectively destroy abnormal blood vessels.
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Topical or systemic NSAIDs can be used as an adjunctive treatment to control minor inflammation and pain.
Emerging Therapies
- JAK Inhibitors: Janus kinase (JAK) inhibitors are being studied for their potential use in treating autoimmune uveitis, including MCP. These orally administered medications inhibit specific pathways involved in the inflammatory response.
- Interleukin Inhibitors: Targeting interleukins, which are important mediators of inflammation, is another promising therapeutic approach. Tocilizumab (anti-IL-6) is being studied for its efficacy in uveitis.
- Stem Cell Therapy: Studies on the use of mesenchymal stem cells to modulate immune responses and promote tissue repair are ongoing. This novel approach could provide new hope for patients with refractory MCP in the future.
Ways to Improve and Prevent Multifocal Choroiditis and Panuveitis (MCP)
- Regular Eye Examinations: Regular eye exams can aid in the early detection and monitoring of ocular changes, allowing for more effective MCP management and the prevention of complications.
- Prompt Treatment of Symptoms: If you experience symptoms such as blurred vision, floaters, or light flashes, seek medical attention right away to ensure timely intervention.
- Adherence to Medication: Adhere to prescribed treatment regimens, including taking medications as directed and attending follow-up appointments to monitor your condition.
- Avoid Triggers: Identify and avoid potential sources of inflammation, such as stress, specific foods, or environmental factors.
- Healthy Lifestyle: Eat a well-balanced diet rich in anti-inflammatory foods, exercise regularly, and avoid smoking to improve overall health and reduce systemic inflammation.
- Protective Eyewear: Wear protective eyewear to avoid trauma or exposure to irritants, which could cause inflammation or worsen the condition.
- Manage Systemic Conditions: Treat any underlying systemic autoimmune or inflammatory conditions, such as rheumatoid arthritis or sarcoidosis, that may affect the course of MCP.
- Patient Education: Be aware of MCP and its potential complications. To take an active role in your care, educate yourself on the symptoms and treatment options.
- Stress Management: To help manage stress, try stress-reduction techniques like mindfulness, meditation, or yoga. Stress can have a negative impact on immunity and inflammation.
- Immunization: Stay up to date on vaccinations to avoid infections that could cause or exacerbate inflammatory responses.
Trusted Resources
Books
- “Uveitis: Fundamentals and Clinical Practice” by Robert B. Nussenblatt and Scott M. Whitcup
- “The Eye: Basic Sciences in Practice” by John V. Forrester, Andrew D. Dick, Paul G. McMenamin, and William R. Lee
- “Retina” by Stephen J. Ryan






