What is a Lacrimal Gland Tumor?
Lacrimal gland tumors are abnormal growths that form in the lacrimal glands, which produce tears. These tumors, whether benign or malignant, can have a significant impact on eye health and vision. Symptoms typically include swelling, pain, and changes in the appearance of the eye. Early diagnosis and treatment are critical for controlling these tumors and avoiding complications. Understanding the nature and characteristics of lacrimal gland tumors is critical to accurate diagnosis and treatment planning.
Detailed Investigation of Lacrimal Gland Tumors
Lacrimal gland tumors are a diverse group of neoplasms that can develop from the various cell types found in the lacrimal gland. These tumors are uncommon, but because of their location and potential for malignancy, they can have serious clinical consequences.
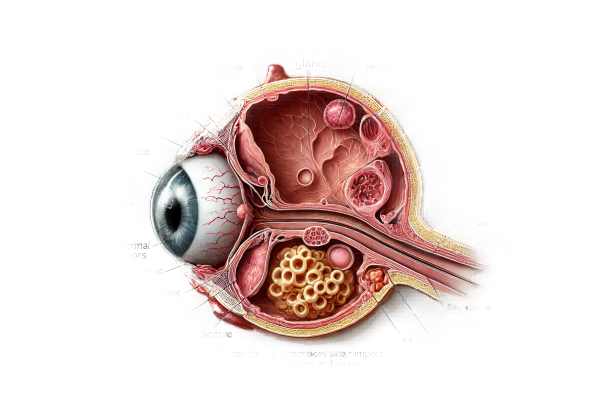
Structure and Function of the Lacrimal Gland
The lacrimal glands are located in the upper outer region of each eye, within the orbit. They produce the aqueous layer of the tear film, which lubricates and protects the ocular surface. The lacrimal gland has two parts: the larger orbital lobe and the smaller palpebral lobe. Tears produced by the lacrimal gland travel through multiple ducts to the conjunctival sac, where they spread across the eye before draining into the nasolacrimal duct.
Types of Lacrimal Gland Tumors
There are two types of lacrimal gland tumors: benign and malignant, each with its own histopathological features and clinical behavior.
Benign Tumors
- Pleomorphic Adenoma (Benign Mixed Tumor): Pleomorphic adenoma is the most common benign tumor of the lacrimal gland, and it grows slowly and painlessly. It usually appears in adults and has a mixed cellular composition, with epithelial and stromal elements. Encapsulation of these tumors aids in surgical removal.
- Adenoid Cystic Carcinoma: Although adenoid cystic carcinomas are typically malignant tumors, some have a relatively slow progression. These tumors are prone to recurrence and metastasis, and they frequently cause pain due to perineural invasion.
- Additional Benign Tumors: Other benign tumors include monomorphic adenoma, oncocytoma, and benign lymphoid hyperplasia. These are less common but have a good prognosis with proper treatment.
Malignant Tumors
- Adenoid Cystic Carcinoma is the most common malignant tumor in the lacrimal gland. It is aggressive, with a high risk of perineural invasion, recurrence, and distant metastasis. Patients typically report pain, proptosis, and a mass in the lacrimal gland region.
- Mucoepidermoid Carcinoma: Mucoepidermoid carcinoma is a type of malignant tumor that contains a mixture of mucus-secreting, squamous, and intermediate cells. It can be aggressive, necessitating significant surgical intervention.
- Lymphoma: Primary lymphoma of the lacrimal gland is a non-Hodgkin lymphoma that manifests as a painless, growing mass. It often has a better prognosis than other malignant tumors if detected and treated early.
- Squamous Cell Carcinoma: Although uncommon, squamous cell carcinoma can develop from the lacrimal gland and is usually aggressive, with a poor prognosis.
- Metastatic Tumors: Tumors that originate in other parts of the body, such as the breast or lung, can spread to the lacrimal gland. These secondary tumors frequently indicate advanced systemic disease.
Symptoms Of Lacrimal Gland Tumors
The symptoms of lacrimal gland tumors vary according to the type and size of the tumor. Common symptoms include:
- Swelling: A palpable mass or swelling of the upper outer quadrant of the orbit.
- Pain: Discomfort or pain, usually caused by malignant tumors that invade nearby structures.
- Proptosis: Forward displacement of the eye, resulting in a bulging appearance.
- Diplopia: Double vision caused by eye displacement and the involvement of extraocular muscles.
- Vision Changes: If the tumor compresses the optic nerve or other critical structures, you may experience blurred or lost vision.
- Epiphora: excessive tearing caused by an obstruction in the lacrimal drainage system.
- Eyelid Changes: Eyelid drooping (ptosis) or contour changes.
Pathophysiology
Lacrimal gland tumors develop as a result of abnormal cell proliferation within the gland. The precise mechanisms differ based on the tumor type:
- Benign Tumors: These are typically caused by a localized overgrowth of glandular or stromal cells. They are frequently well-encapsulated, which reduces their spread.
- Malignant Tumors: Malignant tumours have uncontrolled cell growth, the potential for local invasion, and metastasis. Adenoid cystic carcinoma, for example, is known for its aggressive nature, with a proclivity for perineural invasion, which contributes to discomfort and recurrence.
Epidemiology
Lacrimal gland tumors are uncommon, accounting for only 10% of all orbital tumors. They can occur at any age, but adults are more likely to experience them. There is no significant gender preference. Benign tumors, such as pleomorphic adenoma, are more common than malignant ones.
Risk Factors
Several factors may increase the risk of developing lacrimal gland tumors:
- Age: Adults are more likely to develop lacrimal gland tumors, but children can be affected as well.
- Genetic Predisposition: A family history of similar tumors or other neoplasms may raise the risk.
- Environmental Factors: Exposure to radiation or specific chemicals may increase the risk of developing tumors.
Understanding the specific features and behavior of lacrimal gland tumors is critical for accurate diagnosis and treatment planning. Early detection and appropriate management are critical for improving outcomes and maintaining ocular function.
Diagnostic methods
The correct diagnosis of lacrimal gland tumors requires a combination of clinical evaluation, imaging studies, and histopathological examination. Early and precise diagnosis is critical for determining the best treatment plan and improving patient outcomes.
Clinical Examination
- Patient History: A detailed patient history is required to determine the onset, duration, and progression of symptoms. Key questions include the presence of pain, swelling, visual changes, and a history of cancer or radiation exposure.
- Physical Examination: The clinician conducts a thorough physical examination of the eyes and surrounding structures, concentrating on:
- Visual Inspection: Check for visible swelling, proptosis, or asymmetry in the orbital area.
- Palpation: Gently palpating the orbital region to determine the size, consistency, and mobility of the mass.
- Ocular Movements: Assessing eye movements to identify any restriction or double vision.
- Visual Acuity and Field Testing: Evaluates the patient’s vision and peripheral fields to detect any tumor-related deficits.
Imaging Studies
- Computed Tomography (CT) Scan: CT imaging provides detailed cross-sectional views of the orbit, which aids in determining the tumor’s size, shape, and extent. CT scans are particularly effective at detecting bony involvement and calcifications.
- Magnetic Resonance Imaging (MRI): MRI provides high-resolution images of soft tissues, making it useful for evaluating the lacrimal gland and its surrounding structures. MRI is particularly useful for distinguishing between benign and malignant tumors and assessing perineural invasion in cases of adenoid cystic carcinoma.
- Ultrasound: High-frequency ultrasound can reveal the lacrimal gland and its surrounding tissues. This non-invasive imaging technique aids in determining the gland’s size, position, and any cystic or solid lesions.
Histopathologic Examination
- Biopsy: A biopsy is required for a conclusive diagnosis. Tissue samples for histopathological examination can be obtained through fine-needle aspiration (FNA) or incisional biopsy. The biopsy helps to determine the tumor type, grade, and potential malignancy.
- Cytology and Histology: Biopsy samples are examined under a microscope to determine the tumor’s cellular characteristics. Special staining techniques and immunohistochemical markers can be used to distinguish between different types of tumors.
Additional Diagnostic Tools
- Tear Film Analysis: Analyzing the tear film can provide information about the tumor’s functional impact on tear production and quality. Tear break-up time (TBUT) and osmolarity measurements are useful in diagnosing dry eye syndrome and related conditions.
- Lacrimal Scintigraphy: This nuclear medicine imaging technique involves injecting a radioactive tracer into the tear film and then imaging sequentially to monitor tear production and drainage. It aids in determining the functional impact of the tumour on tear dynamics.
Lacrimal Gland Tumor Treatment
The type, size, location, and whether the tumor is benign or malignant all influence treatment for lacrimal gland tumors. Early and accurate diagnosis is critical for effective treatment planning, which could include surgery, radiation therapy, chemotherapy, or a combination of these methods. Here, we look at the available treatment options, emphasizing innovative and emerging therapies.
Surgical Treatment
- Excisional Biopsy and Resection: For benign tumors like pleomorphic adenomas, the best treatment option is complete surgical excision. The goal is to completely remove the tumor to prevent recurrence. Small, localized malignant tumors can also be removed surgically.
- Debulking Surgery: When complete resection is not possible due to the tumor’s size or location, debulking surgery can be used to reduce the tumor burden. This approach is frequently combined with other treatments, such as radiation or chemotherapy.
- Orbital Exenteration: For advanced malignant tumors that have spread to surrounding tissues, an extensive surgical procedure known as orbital exenteration may be required. To completely clear the tumor, the eye and surrounding orbital contents are removed.
Radiation Therapy
- External Beam Radiation Therapy (EBRT): EBRT is a common adjuvant treatment for malignant lacrimal gland tumors. It can help control local tumour growth and lower the risk of recurrence following surgical resection. EBRT is especially effective against tumors with perineural invasion, such as adenoid cystic carcinoma.
- Brachytherapy is the process of placing radioactive sources near or within a tumor. Brachytherapy delivers a high dose of radiation to the tumor while minimizing exposure to healthy tissues. It is less commonly used, but it can be useful in certain situations.
Chemotherapy
- Systemic Chemotherapy: Chemotherapy can be used to treat malignant tumors, particularly if there is evidence of metastases. It entails administering cytotoxic drugs to eliminate cancer cells. Chemotherapy may be used alone or in conjunction with surgery and radiation therapy.
- Targeted Therapy: Targeted therapies employ drugs that specifically target molecular pathways involved in tumor growth and progression. These treatments may be effective for certain types of lacrimal gland tumors that express specific molecular targets.
Innovative and Emerging Therapies
- Immunotherapy: Immunotherapy uses the body’s immune system to combat cancer. Checkpoint inhibitors and other immunotherapeutic agents are being investigated for their potential use in treating lacrimal gland tumors, particularly those that are resistant to conventional treatments.
- Gene Therapy: Gene therapy seeks to correct genetic mutations or introduce new genes to combat cancer cells. Gene therapy approaches for treating lacrimal gland tumors are being investigated.
- Photodynamic Therapy (PDT): PDT consists of administering a photosensitizing agent that selectively accumulates in tumor cells, followed by exposure to a specific wavelength of light. This process generates reactive oxygen species, which kill tumor cells. PDT is being studied for its ability to treat lacrimal gland tumors with minimal damage to nearby tissues.
- Nanotechnology-Based Therapies: Nanotechnology provides novel methods for delivering drugs directly to tumor cells while minimizing side effects. Nanoparticles can be designed to deliver chemotherapeutic agents, targeted therapies, or gene therapies to lacrimal gland tumors.
Integrating traditional treatments with innovative and emerging therapies allows healthcare providers to provide a comprehensive and personalized approach to managing lacrimal gland tumors. This approach seeks to maximize treatment efficacy while minimizing side effects and improving patient outcomes.
Effective Methods for Improving and Avoiding Lacrimal Gland Tumors
- Regular Eye Examinations: Schedule regular eye exams to catch any problems early. Early detection of lacrimal gland tumors can lead to better treatment outcomes.
- Protect Your Eyes: Wear protective eyewear when participating in activities that pose a risk of eye injury, such as sports, construction work, or other hazardous activities. Reducing trauma can lower the risk of tumor development.
- Avoid Radiation Exposure: Limit your exposure to radiation, including medical imaging tests. When necessary, implement protective measures to reduce radiation exposure to the eyes.
- Healthy Lifestyle Choices: Eat a nutritious diet, exercise regularly, and avoid smoking. These lifestyle changes can lower the risk of cancer and improve overall health.
- Genetic Counseling: If you have a family history of lacrimal gland tumors or other cancers, seek genetic counseling. Understanding your genetic risk allows you to take proactive steps to monitor and manage your health.
- Manage Chronic Inflammation: Treat chronic inflammatory conditions like sarcoidosis or thyroid eye disease. Chronic inflammation may increase the likelihood of tumor development.
- Monitor for Symptoms: Keep an eye out for swelling, pain, or changes in vision. Early notification of these symptoms to an eye care professional can result in a timely diagnosis and treatment.
- Reduce Environmental Exposures: Limit your exposure to environmental toxins and pollutants that can raise the risk of cancer. When working with hazardous substances, take appropriate precautions.
- Follow Up on Eye Injuries: If you have an eye injury, seek medical attention right away and follow up as recommended. Proper management of eye injuries can help to avoid complications that may lead to tumor development.
Trusted Resources
Books
- “Diseases of the Lacrimal System” by John D. Dartt
- “Principles and Practice of Lacrimal Surgery” by Mohammad Javed Ali






