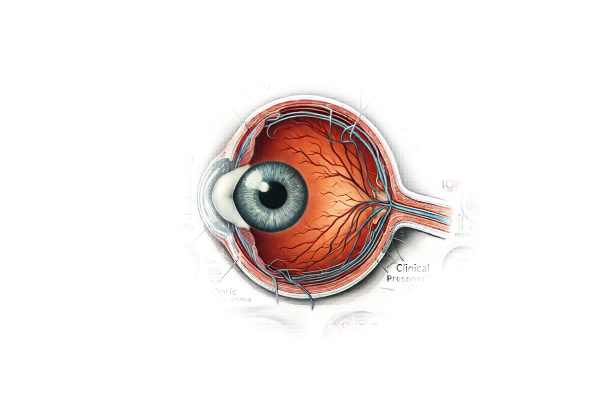
What is Normal Tension Glaucoma?
Normal-tension glaucoma (NTG), also known as low-tension or normal-pressure glaucoma, is a type of glaucoma that causes optic nerve damage despite normal intraocular pressure (IOP). Unlike other types of glaucoma, in which high IOP is a significant risk factor, NTG patients have normal IOP levels (10-21 mmHg). The exact cause of NTG is unknown, but it is thought to be associated with vascular factors and optic nerve susceptibility. Early detection and management are critical for avoiding progressive vision loss.
Detailed Analysis of Normal-Tension Glaucoma
Normal-tension glaucoma is a multifaceted condition that causes progressive optic neuropathy and visual field loss despite having normal IOP. Understanding the pathophysiology, risk factors, clinical presentation, and potential complications is critical for accurate diagnosis and treatment.
Pathophysiology
The pathophysiology of NTG is complex and not completely understood. Several hypotheses have been proposed to explain the optic nerve damage observed in NTG patients.
- Vascular Dysregulation: One theory holds that NTG is primarily a vascular disease. Poor blood flow to the optic nerve can cause ischemia and subsequent nerve damage. Systemic hypotension, nocturnal hypotension, and vasospastic disorders (such as migraines or Raynaud’s phenomenon) are thought to contribute to decreased blood flow.
- Optic Nerve Susceptibility: Some people may have an inherently more fragile optic nerve, making them more vulnerable to damage even at normal IOP. Genetic factors, structural variations in the optic nerve head, and impaired autoregulation of blood flow are all possible contributing factors.
- Mechanical Factors: Even if IOP is within the normal range, it may still be too high for some susceptible optic nerves. This relative increase in pressure may result in mechanical stress and damage over time.
Risk Factors
Several risk factors have been associated with the development and progression of NTG.
- Age: NTG primarily affects older adults, and the risk rises with age.
- Race: NTG is more common in people of Japanese descent, but it can affect people of any ethnicity.
- Family History: A family history of glaucoma raises the possibility of developing NTG.
- Cardiovascular Disease: Hypertension, atherosclerosis, and nocturnal hypotension are associated with NTG.
- Vasospastic Disorders: Migraines and Raynaud’s phenomenon are associated with NTG, possibly due to their effect on blood flow.
- Myopia: Nearsightedness (myopia) is a risk factor for NTG.
Clinical Features
NTG shares many clinical features with other types of glaucoma, but has some distinct characteristics.
- Optic Nerve Damage: Patients have typical glaucomatous changes to the optic nerve head, such as cupping and thinning of the neuroretinal membrane. These changes happen despite normal IOP levels.
- Visual Field Defects: Progressive loss of peripheral vision is a defining feature of NTG. Patients may experience blind spots (scotomas) in their visual field, which can worsen over time if not managed.
- Normal Intraocular Pressure: IOP measurements are within the normal range, distinguishing NTG from other types of glaucoma with elevated IOP.
Differential Diagnosis NTG should be distinguished from other conditions that may present similarly.
- Primary Open-Angle Glaucoma (POAG): POAG causes elevated IOP and similar optic nerve damage, but it differs from NTG due to the higher pressure levels.
- Secondary Glaucomas: These glaucomas are caused by other ocular or systemic conditions, such as uveitis, trauma, or steroid use, resulting in increased IOP and optic nerve damage.
- Non-Glaucomatous Optic Neuropathy: Conditions such as ischemic optic neuropathy, optic neuritis, and compressive optic neuropathy can all cause optic nerve damage, but they have different causes and treatments.
Complications
Untreated or poorly managed NTG can cause serious complications:
- Progressive Vision Loss: The primary complication of NTG is a gradual loss of peripheral vision, which can eventually impair central vision if not treated.
- Blindness: Advanced NTG can cause severe vision impairment or blindness, significantly lowering the patient’s quality of life.
- Impact on Daily Activities: NTG-related vision loss can interfere with daily activities such as reading, driving, and recognizing faces, increasing reliance on others and decreasing independence.
Prognosis
The prognosis for NTG varies depending on the stage of diagnosis and the effectiveness of the management plan. Early detection and consistent management can slow the progression of optic nerve damage, preserving vision. However, NTG is a chronic condition that requires ongoing monitoring and treatment to reduce the risk of vision loss.
Diagnostic methods
A comprehensive approach, including clinical evaluation, imaging studies, and functional tests, is required to accurately diagnose normal-tension glaucoma. These methods aid in the confirmation of the diagnosis, determining the extent of optic nerve damage, and distinguishing NTG from other ocular disorders.
Clinical Evaluation
A thorough clinical evaluation is the first step in diagnosing NTG. Key elements of the evaluation include:
- Patient History: Obtaining detailed information about the patient’s symptoms, medical history, glaucoma family history, and any cardiovascular or vasospastic disorders.
- Visual Acuity Test: Evaluates the patient’s vision to see if there are any reductions in visual acuity.
- Intraocular Pressure Measurement: Using tonometry to confirm that IOP levels are within the normal range (10-21 mmHg).
Ophthalmic Examination
- Gonioscopy is a procedure that uses a special lens to examine the anterior chamber angle of the eye. This distinguishes NTG from other types of glaucoma involving angle closure mechanisms.
- Slit-Lamp Examination: Using a slit-lamp microscope, examine the eye’s structures, including the cornea, iris, and lens, to detect any abnormalities.
Imaging Studies
- Optical Coherence Tomography (OCT): OCT can produce high-resolution cross-sectional images of the optic nerve head and retinal nerve fiber layer. This imaging technique is useful for determining the extent of optic nerve damage and monitoring disease progression.
- Confocal Scanning Laser Ophthalmoscopy: This imaging technique generates detailed topographic images of the optic nerve head, allowing for accurate measurements of optic disc cupping and rim area.
- Scanning Laser Polarimetry: This technique determines the thickness of the retinal nerve fiber layer, revealing important information about nerve fiber loss.
Functional Tests
- Visual Field Testing: Also known as perimetry, this test evaluates the patient’s visual field to identify peripheral vision loss or scotomas. Automated perimetry is a popular method for measuring visual field defects and tracking changes over time.
- Pachymetry: Measuring the thickness of the cornea can aid in the accurate interpretation of IOP readings, as corneal thickness influences pressure measurements.
Additional Diagnostic Considerations
- Blood Pressure Monitoring: Because vascular factors are involved in NTG, monitoring blood pressure, particularly nocturnal hypotension, is critical. Ambulatory blood pressure monitoring can be used to track blood pressure fluctuations over 24 hours.
- Cardiovascular Assessment: Assessing cardiovascular health and identifying any underlying conditions, such as atherosclerosis or vasospastic disorders, can reveal potential contributing factors to NTG.
Normal-tension glaucoma treatment Options
The goal of treating normal-tension glaucoma (NTG) is to reduce intraocular pressure (IOP) in order to slow the progression of optic nerve damage and preserve vision. Even though NTG patients have normal IOP levels, lowering pressure can be beneficial. Medication, laser therapy, and surgical procedures are all possible treatment options. Emerging therapies show promise for future management.
Medications
- Prostaglandin Analogues: These are the first-line medications for NTG. Medications such as latanoprost, bimatoprost, and travoprost increase the flow of aqueous humor, lowering IOP.
- Beta Blockers: Drugs like timolol and betaxolol reduce the production of aqueous humor. They frequently work in tandem with prostaglandin analogues.
- Alpha Agonists: Brimonidine reduces aqueous humor production while increasing uveoscleral outflow.
- Carbonic Anhydrase Inhibitors: Both oral and topical forms (such as acetazolamide and dorzolamide) reduce the production of aqueous humor.
- Rho Kinase Inhibitors: Netarsudil is a newer type of medication that reduces IOP by increasing trabecular meshwork outflow.
Laser Therapy
- Selective Laser Trabeculoplasty (SLT): SLT uses a laser to target the trabecular meshwork, increasing aqueous outflow and lowering IOP. It is a reasonably safe and effective treatment for NTG patients.
- Micropulse Laser Therapy: This therapy uses a low-energy laser to target the ciliary body and reduce aqueous humor production while causing minimal tissue damage.
Surgical Interventions
- Trabeculectomy: This surgical procedure creates a new drainage pathway for aqueous humor, resulting in lowered IOP. It is usually considered when medications and laser treatments are insufficient.
- Glaucoma Drainage Devices: Implants such as the Ahmed valve or Baerveldt tube shunt assist in draining excess aqueous humor, lowering IOP.
- Minimally Invasive Glaucoma Surgery (MIGS): Procedures like the iStent, Hydrus microstent, and Trabectome provide less invasive ways to lower IOP by improving aqueous outflow via the trabecular meshwork or other pathways.
Innovative and Emerging Therapies
- Neuroprotective Agents: Researchers are looking into drugs that can protect the optic nerve from damage regardless of IOP. These agents target oxidative stress and apoptosis.
- Gene Therapy: Experimental gene therapy approaches aim to modify genes involved in optic nerve susceptibility and vascular regulation, which could provide long-term solutions for NTG.
- Stem Cell Therapy: Research into stem cell therapy focuses on the regeneration of damaged optic nerve fibers and the restoration of vision.
Effective Ways to Improve and Prevent Normal-Tension Glaucoma
Preventing and managing normal-tension glaucoma requires proactive strategies and lifestyle changes to reduce risk factors and improve eye health. Here are a few effective methods:
- Regular Eye Examinations: Schedule regular eye exams to look for early signs of NTG, especially if you are at a higher risk due to age, family history, or underlying conditions.
- Control Blood Pressure: Maintain healthy blood pressure levels through medication, diet, and exercise. Avoid large fluctuations, especially nocturnal hypotension.
- Manage Cardiovascular Health: Treat cardiovascular risk factors like hypertension, diabetes, and hyperlipidemia with proper medical care and lifestyle changes.
- Avoid Smoking: Quit smoking to improve vascular health and lower your risk of optic nerve damage.
- Exercise Regularly: Regular physical activity promotes overall health and increases blood flow to the optic nerve.
- Protect Your Eyes: Wear protective eyewear when participating in activities that pose a risk of eye injury, which can worsen optic nerve damage.
- Monitor Medications: Be aware of the possible effects of medications on IOP and vascular health. If you have any concerns, consult your healthcare provider.
- Healthy Diet: Eat a well-balanced diet high in antioxidants, vitamins, and minerals to improve eye health. Leafy greens, fish, and nuts are all good sources of nutrition.
Individuals who follow these preventive measures and live a healthy lifestyle can reduce their risk of developing NTG and manage the condition more effectively if diagnosed.
Trusted Resources
Books
- “Clinical Ophthalmology: A Systematic Approach” by Jack J. Kanski
- “The Glaucoma Book: A Practical, Evidence-Based Approach to Patient Care” by Paul N. Schacknow and John R. Samples
- “Optic Nerve Disorders: Diagnosis and Management” by Jane W. Chan






