Blepharospasm is a chronic neurological condition marked by involuntary, repetitive contractions of the muscles around the eyes. These spasms often begin subtly but can progress to frequent blinking and even forceful closure of the eyelids, interfering with daily activities and reducing quality of life. While its precise cause remains unclear, blepharospasm is classified as a focal dystonia and can significantly impact vision, driving, reading, and social interactions. Fortunately, a growing range of medical, surgical, and technological advances now offer hope for better symptom control, improved independence, and enhanced well-being for those living with this challenging disorder.
Table of Contents
- Understanding Blepharospasm: Definition, Underlying Causes & Epidemiology
- Conventional Therapy Options and Medical Management
- Surgical Interventions and Minimally Invasive Procedures
- Advances in Technology and Novel Approaches
- Clinical Trials, Research, and Future Perspectives
- Frequently Asked Questions
Understanding Blepharospasm: Definition, Underlying Causes & Epidemiology
Blepharospasm is a type of focal dystonia that causes involuntary, often forceful, contractions of the orbicularis oculi muscles surrounding the eyes. Over time, these spasms can result in frequent blinking, eye discomfort, and episodes of eyelid closure that make it difficult to keep the eyes open. While mild symptoms may be overlooked, advanced cases can lead to significant visual impairment and affect independence.
Key Aspects:
- Primary (essential) blepharospasm: Occurs without an identifiable underlying disease; believed to result from dysfunction in brain areas controlling movement, such as the basal ganglia.
- Secondary blepharospasm: Can develop after eye trauma, infections, certain medications, or neurological disorders like Parkinson’s disease.
Epidemiology:
- Prevalence estimates range from 5 to 133 cases per million people.
- Most commonly affects adults between ages 50–70, with a higher incidence in women.
- Frequently misdiagnosed as “dry eye” or psychological in origin in early stages.
Risk Factors & Triggers:
- Genetic predisposition (family history may increase risk)
- Chronic eye irritation (dry eye, allergies, environmental stressors)
- Psychological stress, fatigue, or bright lights can exacerbate symptoms.
Natural History:
- Blepharospasm often starts with increased blinking or eye irritation, progressing over months or years.
- Symptoms may fluctuate, worsening with fatigue or anxiety.
Practical Advice:
Early recognition is vital. If you notice persistent, uncontrolled blinking or difficulty keeping your eyes open, consult a neurologist or ophthalmologist with expertise in movement disorders.
Conventional Therapy Options and Medical Management
For most patients with blepharospasm, non-surgical treatments provide the initial and often most effective symptom relief.
Primary Treatments:
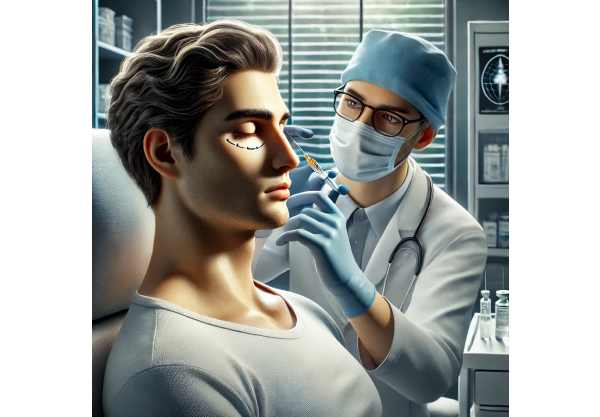
- Botulinum toxin (Botox) injections:
- The gold standard, these injections relax overactive eyelid muscles, significantly reducing spasms for 3–4 months per session.
- Performed in the doctor’s office, injections are tailored to the severity and location of muscle involvement.
- Common brands include Botox, Dysport, Xeomin, and Myobloc.
- Oral medications:
- Occasionally used as adjuncts, particularly in those who do not fully respond to botulinum toxin.
- Options include benzodiazepines (clonazepam), anticholinergic agents (trihexyphenidyl), or muscle relaxants.
- Effectiveness varies, and side effects can limit use, especially in older adults.
- Supportive Measures:
- Use sunglasses or tinted lenses to reduce light sensitivity (photophobia).
- Apply warm compresses or artificial tears to minimize irritation.
- Practice stress management techniques—such as meditation, biofeedback, or cognitive behavioral therapy—as stress can worsen spasms.
Lifestyle and Practical Tips:
- Keep a symptom diary to identify personal triggers.
- Minimize screen time or take frequent breaks when using digital devices.
- Maintain good sleep hygiene, as fatigue often amplifies symptoms.
Patient Counseling:
Open communication with your care team ensures prompt adjustments if your treatment loses effectiveness or if side effects arise.
Surgical Interventions and Minimally Invasive Procedures
Surgical options are reserved for individuals who do not achieve adequate relief from conservative measures, particularly botulinum toxin injections.
Key Surgical Techniques:
- Myectomy:
- Surgical removal of some or all of the eyelid muscles responsible for spasms (usually the orbicularis oculi).
- May be partial (removing part of the muscle) or extensive (targeting most of the involved muscle tissue).
- Most beneficial for severe, drug-resistant cases.
- Selective neurectomy:
- Targeted cutting of facial nerve branches that supply the affected muscles, rarely performed today due to the effectiveness of botulinum toxin.
- Deep brain stimulation (DBS):
- Investigational and reserved for the most severe, treatment-resistant cases.
- Electrodes are implanted in specific brain regions to modulate abnormal signals.
Perioperative Considerations:
- Surgery requires careful patient selection and preoperative evaluation to exclude other movement disorders.
- Recovery can vary; swelling and bruising may occur but typically resolve within weeks.
Potential Complications:
- Eyelid drooping (ptosis), incomplete eyelid closure, dry eye symptoms, or changes in facial appearance.
- Close follow-up is essential to monitor healing and address any issues early.
Practical Advice:
Always consult with a surgeon experienced in facial dystonia surgery. Consider second opinions and ask about less invasive options before proceeding.
Advances in Technology and Novel Approaches
Recent years have seen exciting progress in the diagnosis and treatment of blepharospasm, expanding options and improving quality of care.
Diagnostic Advances:
- High-speed videography:
- Used to analyze blink patterns, assess treatment response, and support precise diagnosis.
- Electromyography (EMG):
- Guides targeted botulinum toxin injections by mapping muscle activity in real time.
Therapeutic Innovations:
- New botulinum toxin formulations:
- Longer-acting or less immunogenic variants offer hope for extended relief with fewer injections.
- Drug delivery technologies:
- Microsphere and sustained-release systems may allow more precise dosing and reduce treatment frequency.
Neuromodulation & Digital Tools:
- Transcranial magnetic stimulation (TMS):
- Noninvasive stimulation of the brain is being studied for difficult cases.
- Wearable blink-monitoring devices:
- Help patients track symptom patterns and optimize therapy timing.
Emerging Therapies:
- Gene therapy:
- In early research phases, aiming to correct underlying neural signaling dysfunctions.
- AI-assisted therapy planning:
- Artificial intelligence models help predict individualized responses to therapy and support shared decision-making.
Practical Advice:
Ask your provider about clinical trial options and whether emerging therapies might be right for you. Technological advances often arrive first at academic centers.
Clinical Trials, Research, and Future Perspectives
The landscape for blepharospasm management continues to evolve as ongoing research uncovers new insights and solutions.
Key Areas of Research:
- Genetics:
- Studies aim to identify risk genes and hereditary patterns, potentially enabling preventive strategies in the future.
- Pharmacology:
- Trials are evaluating new oral and injectable medications targeting different pathways involved in dystonia.
- Surgical innovations:
- Improvements in myectomy and neuromodulation are being tested for safety and efficacy.
Patient-Centered Outcomes:
- Researchers are developing better ways to measure daily functioning and quality of life, ensuring that new treatments align with patient goals.
- Patient advocacy groups increasingly partner with researchers to guide trial priorities.
How to Get Involved:
- Ask your healthcare provider or visit clinical trial registries to learn about ongoing studies.
- Participate in registries or support groups, which often have the latest updates on research and care resources.
Future Directions:
- Integration of digital health tools and AI for remote symptom tracking, early intervention, and tailored therapy.
- Ongoing search for disease-modifying therapies that target the root cause—not just the symptoms—of blepharospasm.
Practical Advice:
Stay informed about clinical trials and research breakthroughs. New options are on the horizon that could dramatically improve symptom control and independence.
Frequently Asked Questions
What is the best treatment for blepharospasm?
Botulinum toxin injections are currently the most effective and widely used treatment, offering relief for most patients within days and lasting for several months per injection.
Is blepharospasm a permanent condition?
Blepharospasm is usually chronic, but symptom severity can vary. Many people manage symptoms well with ongoing treatment, and research continues for longer-lasting solutions.
Can blepharospasm be cured with surgery?
Surgery can help severe cases unresponsive to medications or injections, but it is not a guaranteed cure and may not eliminate all symptoms. Careful selection and postoperative care are vital.
What triggers blepharospasm symptoms?
Common triggers include bright lights, fatigue, stress, eye irritation, and sometimes certain medications. Identifying and minimizing triggers can help reduce symptom frequency and intensity.
Are there new treatments for blepharospasm?
Yes, ongoing research explores longer-acting medications, innovative surgical approaches, and digital health tools for monitoring and therapy optimization.
Is blepharospasm related to other neurological diseases?
Blepharospasm can occur alone or alongside other dystonias and movement disorders. Occasionally, it may be linked to conditions like Parkinson’s disease.
How can I find support or connect with others living with blepharospasm?
National dystonia and blepharospasm support groups provide resources, connect you with others, and share news about treatment advances and clinical trials.
Disclaimer:
This article is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always consult your healthcare provider with questions about a medical condition.
If you found this guide helpful, please share it on Facebook, X (formerly Twitter), or your preferred social platform—and follow us for future updates! Your support helps us continue producing in-depth, evidence-based health content.






