Intermediate uveitis is an eye condition that involves inflammation in the middle part of the eye, particularly the vitreous and surrounding tissues. While it can affect anyone, it most often impacts young adults and can lead to serious vision issues if not managed properly. With a range of treatment options—from established medications to advanced surgical interventions and emerging innovations—patients today have more paths to lasting relief than ever before. Let’s explore the current landscape of intermediate uveitis management so you can make informed decisions about your eye health.
Table of Contents
- Condition Overview and Epidemiology
- Conventional and Pharmacological Therapies
- Surgical and Interventional Procedures
- Emerging Innovations and Advanced Technologies
- Clinical Trials and Future Directions
- Frequently Asked Questions
Condition Overview and Epidemiology
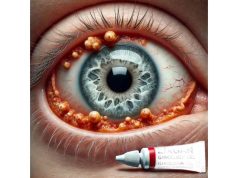
Intermediate uveitis, sometimes referred to as pars planitis or vitritis, is an inflammatory disorder affecting the vitreous, peripheral retina, and the ciliary body in the eye’s middle segment. This form of uveitis is unique because it mainly targets the area just behind the lens, leading to symptoms like floaters and blurry vision rather than redness or eye pain. Understanding this condition’s fundamentals is essential for effective management and timely intervention.
What Is Intermediate Uveitis?
Intermediate uveitis is characterized by the inflammation of the vitreous body and the adjacent structures, such as the pars plana (a part of the ciliary body) and peripheral retina. Unlike anterior or posterior uveitis, this condition tends to center on the mid-eye, often making early detection a challenge.
Pathophysiology:
The condition is considered immune-mediated. In many cases, the exact cause remains unknown (idiopathic), though it may be linked with systemic autoimmune diseases, including multiple sclerosis and sarcoidosis. The inflammation can lead to cellular debris accumulating in the vitreous (vitritis), resulting in hazy vision or spots.
Prevalence and Risk Factors:
Intermediate uveitis is less common than other forms of uveitis, accounting for roughly 5–15% of all uveitis cases globally. It tends to appear in young adults between ages 20 and 40 but can affect children and older adults as well.
Risk factors include:
- Genetic predisposition (e.g., HLA associations)
- Presence of systemic autoimmune or inflammatory diseases
- Family history of autoimmune disorders
Common Symptoms:
- Floaters (dark spots moving across the field of vision)
- Blurred or decreased vision
- Mild ocular discomfort (but often painless)
- Occasional mild redness
Early diagnosis is crucial to preventing complications like cystoid macular edema, cataracts, or glaucoma. If you or a loved one experience persistent floaters or vision changes, consult an eye care professional promptly.
Conventional and Pharmacological Therapies
Conventional management of intermediate uveitis centers on controlling inflammation, preserving vision, and minimizing treatment side effects. This typically involves a combination of medications tailored to disease severity and patient needs. Understanding each treatment’s mechanism and proper usage empowers patients to actively participate in their care plan.
First-Line Therapies: Corticosteroids
Corticosteroids are the mainstay of treatment due to their potent anti-inflammatory effects.
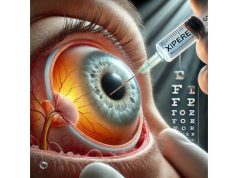
- Local Steroid Injections:
- Periocular (around the eye) or intravitreal (inside the eye) injections deliver steroids directly to the affected area, minimizing systemic exposure.
- Commonly used agents: Triamcinolone acetonide, dexamethasone.
- Systemic Steroids:
- Oral prednisone is reserved for more severe cases or bilateral disease.
- Dosage varies based on severity but usually starts with 0.5–1 mg/kg/day, then tapered based on response.
Immunomodulatory Agents (Steroid-Sparing Drugs):
For chronic, recurrent, or steroid-resistant cases, immunosuppressive medications may be introduced:
- Methotrexate: Weekly oral or injectable doses; requires monitoring of liver function and blood counts.
- Mycophenolate mofetil: Effective for long-term control with a relatively favorable safety profile.
- Azathioprine or Cyclosporine: Alternatives for patients who cannot tolerate or do not respond to other agents.
Biologic Therapies:
These targeted drugs, including anti-TNF-alpha agents (such as adalimumab and infliximab), have revolutionized care for refractory intermediate uveitis:
- Adalimumab: FDA-approved for non-infectious uveitis; administered as a subcutaneous injection every other week.
- Infliximab: Given as intravenous infusions, particularly in cases associated with systemic inflammatory disease.
Adjunctive Measures and Supportive Care:
- Topical Steroids: Used primarily if anterior segment inflammation is present.
- Cycloplegic Agents: Help relieve pain from ciliary spasm and prevent the formation of synechiae (adhesions).
- Ocular Lubricants: Improve comfort, especially in patients with mild irritation or dryness.
Practical Advice for Patients:
- Adhere to your prescribed regimen and never stop corticosteroids abruptly without consulting your physician.
- Report any side effects promptly (such as weight gain, high blood pressure, or mood changes).
- Regular blood tests are needed when on immunosuppressants to monitor for complications.
Choosing the right treatment often requires balancing efficacy and side effects, and it’s common for regimens to be adjusted over time. Collaboration with a uveitis specialist ensures the most up-to-date, personalized care.
Surgical and Interventional Procedures
While many cases of intermediate uveitis can be managed medically, certain situations call for surgical intervention—especially when complications develop or medical therapy proves insufficient. Advances in ophthalmic surgery now offer improved outcomes and faster recovery for patients requiring procedural care.
Indications for Surgery:
- Persistent or recurrent cystoid macular edema unresponsive to medication
- Significant vitreous opacities causing vision loss
- Complications such as retinal detachment, cataract, or glaucoma
Key Surgical Procedures:
- Pars Plana Vitrectomy (PPV):
- What It Is: A minimally invasive procedure that removes the vitreous gel and inflammatory debris, clearing vision and reducing inflammatory stimulus.
- Benefits: Especially helpful for patients with dense vitreous opacities or persistent macular edema.
- Post-Surgical Care: Usually involves continued use of anti-inflammatory medication to prevent recurrence.
- Cataract Surgery:
- Indication: Chronic steroid use or persistent inflammation can accelerate cataract formation.
- Considerations: Pre- and post-operative control of inflammation is critical for optimal results.
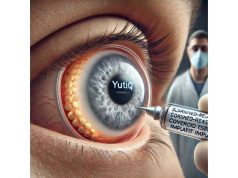
- Implantation of Intravitreal Steroid Devices:
- Examples: Fluocinolone acetonide (Retisert®) and dexamethasone (Ozurdex®) implants deliver a sustained dose of corticosteroid directly to the eye.
- Advantages: Reduce the need for frequent injections or systemic medication.
- Potential Risks: Include increased intraocular pressure or infection, which require close monitoring.
- Glaucoma Surgery:
- For cases where intraocular pressure cannot be controlled by medication alone, surgical intervention (such as trabeculectomy or drainage device implantation) may be necessary.
Laser Treatments:
Laser photocoagulation can be used in rare cases to treat retinal neovascularization or vascular leakage, though it is less commonly required for intermediate uveitis than for other uveitis forms.
Patient-Centered Advice:
- Discuss surgical options thoroughly with your ophthalmologist to understand the risks, benefits, and expected recovery.
- Preparing for surgery includes controlling inflammation beforehand, which may involve a temporary increase in medication.
- Attend all post-operative follow-up appointments, as this is vital to achieving the best possible outcome.
The decision to proceed with surgery is highly individualized, emphasizing the need for shared decision-making between patient and specialist.
Emerging Innovations and Advanced Technologies
The field of uveitis management is experiencing rapid progress, with new technologies and therapies offering hope to patients whose disease proves resistant to conventional treatments. Recent advances focus on precision medicine, improved safety, and better long-term control of inflammation.
Biologic Therapies and Targeted Immune Modulators:
- Interleukin (IL)-6 Inhibitors:
- Agents such as tocilizumab are showing promise in clinical trials for patients unresponsive to TNF inhibitors.
- JAK Inhibitors:
- Small molecule drugs targeting Janus kinase pathways may offer oral alternatives for some patients.
- Anti-VEGF Agents:
- Originally developed for macular degeneration, these drugs (e.g., ranibizumab, aflibercept) are being explored for uveitis-related macular edema.
Gene and Cell-Based Therapies:
- Gene Therapy:
- Experimental approaches aim to introduce genes that modulate immune responses or reduce inflammatory mediators, potentially offering longer-lasting remission.
- Stem Cell Therapy:
- Investigational protocols use mesenchymal stem cells to reduce ocular inflammation, with early studies showing encouraging results in refractory cases.
Next-Generation Drug Delivery Systems:
- Biodegradable Implants:
- Newer implants provide sustained-release corticosteroids or immunomodulators, reducing the need for repeated injections.
- Microneedle Arrays:
- Under study as a less invasive, targeted way to deliver drugs to the back of the eye.
Advances in Imaging and Diagnostics:
- Artificial Intelligence (AI) and Machine Learning:
- AI-powered platforms assist in early detection, monitoring treatment response, and predicting flares, supporting clinicians with more precise decision-making.
- Optical Coherence Tomography Angiography (OCTA):
- Allows noninvasive, detailed visualization of retinal blood vessels, aiding early detection of complications.
Patient Empowerment Tools:
- Digital health apps now enable patients to track symptoms, medication adherence, and communicate with their care team, leading to more proactive disease management.
Practical Advice for the Future:
- Stay informed about new clinical trials or advanced treatments; eligibility for innovative therapies may require early referral to a tertiary center.
- Don’t hesitate to ask your care team about the latest options—participating in research may give access to therapies not yet widely available.
The future of intermediate uveitis care is bright, with breakthroughs continually reshaping the treatment landscape.
Clinical Trials and Future Directions
Research into intermediate uveitis is dynamic and far-reaching, with numerous clinical trials shaping tomorrow’s standards of care. Participating in clinical trials may offer early access to novel therapies and contributes to advancing the field for future patients.
Key Areas of Research:
- Novel Biologic and Small Molecule Drugs:
- Trials are underway to test new agents, such as IL-17 and IL-23 inhibitors, for their safety and efficacy in uveitis not controlled by existing drugs.
- Advanced Drug Delivery Systems:
- Investigational sustained-release devices and ocular injections aim to improve convenience and minimize side effects.
- Gene and Cell Therapy Trials:
- Early-phase studies are assessing the potential for gene editing or stem cell transplantation to induce durable remission.
- AI-Based Diagnostic and Monitoring Tools:
- Projects are exploring how artificial intelligence can help personalize treatment and improve early detection of complications.
How to Find and Participate in Clinical Trials:
- Reputable databases (such as clinicaltrials.gov) provide up-to-date listings of ongoing studies, with eligibility criteria and site locations.
- Discuss with your ophthalmologist whether a trial might be suitable; participation is always voluntary, with detailed informed consent.
What’s on the Horizon?
- Personalized, targeted therapies tailored to individual genetic or immune profiles.
- Safer, more effective immunomodulators with fewer side effects.
- Continued integration of technology for remote monitoring and virtual care.
Patient Empowerment:
- Stay curious and proactive; new research may unlock better options for you or your loved ones.
- Join support groups or online communities to connect with others and share experiences navigating treatment advances.
The next generation of intermediate uveitis treatments is being shaped today by dedicated researchers, clinicians, and empowered patients.
Frequently Asked Questions
What are the best treatment options for intermediate uveitis?
The most effective treatments for intermediate uveitis typically start with corticosteroids to reduce inflammation, followed by immunosuppressive medications for chronic cases. Surgery or advanced therapies may be considered if medical management is insufficient.
How is intermediate uveitis diagnosed?
Diagnosis involves a comprehensive eye exam, specialized imaging (such as OCT and fluorescein angiography), and blood tests to rule out systemic diseases. Early diagnosis is key to preventing vision loss.
Can intermediate uveitis cause permanent vision loss?
If left untreated, intermediate uveitis can lead to complications like macular edema, cataracts, or glaucoma, potentially causing irreversible vision impairment. Prompt and ongoing treatment significantly reduces this risk.
Are there any new treatments for intermediate uveitis?
Yes, new biologic drugs, gene therapies, and innovative drug delivery systems are being developed and tested. Some are available through clinical trials or specialty centers, offering hope for patients with difficult-to-treat cases.
How long does treatment for intermediate uveitis usually last?
Treatment duration varies by severity and response. Some patients may need therapy for months, while others require ongoing management. Regular follow-up is important to monitor disease activity and adjust the plan.
Is intermediate uveitis associated with other health conditions?
Intermediate uveitis can occur alone or alongside systemic autoimmune disorders like multiple sclerosis or sarcoidosis. Your doctor may recommend additional tests to check for underlying conditions.
What lifestyle changes can help manage intermediate uveitis?
Maintaining a healthy lifestyle—avoiding smoking, managing stress, and adhering to your prescribed treatment plan—can help control inflammation and protect your vision over time.
Disclaimer:
This guide is intended for educational purposes only and should not be used as a substitute for professional medical advice, diagnosis, or treatment. Always consult with a qualified healthcare provider regarding any questions or concerns you may have about your eye health or medical condition.
We hope you found this guide helpful! If so, please consider sharing it with friends, family, or your social media community on Facebook, X (formerly Twitter), or your favorite platform. Your support helps us continue providing high-quality, accessible health information for everyone—thank you for being part of our journey!