Traumatic cataract is an ocular condition in which the crystalline lens of the eye becomes opaque as a result of an injury. Unlike age-related cataracts, which form gradually over time, traumatic cataracts can form quickly after a direct impact, penetrating injury, or blunt trauma to the eye. This condition can affect people of any age and is especially common in areas where eye protection during work or sports is not common.
Traumatic cataracts can develop as a result of a variety of eye injuries, including mechanical trauma, chemical burns, radiation exposure, and electrical shock. A traumatic cataract may cause blurred vision, double vision, glare, halos around lights, and visible whiteness or cloudiness in the pupil. In severe cases, the injury may result in additional complications such as glaucoma, retinal detachment, or intraocular inflammation, further impairing vision.
Early diagnosis and treatment of traumatic cataracts are critical for avoiding long-term visual impairment and maintaining quality of life. Ophthalmologists usually use a combination of patient history, visual acuity tests, slit-lamp examinations, and imaging studies to determine the extent of the cataract and any associated ocular damage. Understanding the underlying mechanisms and consequences of traumatic cataracts is critical for creating effective treatment plans and improving patient outcomes.
Standard Traumatic Cataract Treatment Methods
Traumatic cataracts require a comprehensive approach that addresses both the cataract and any associated ocular injuries. Early intervention is critical for preventing future complications and restoring vision. Standard treatment methods for traumatic cataracts usually include the following:
Medical Management
When the cataract does not significantly impair vision or when immediate surgery is not possible, medical management may be used to control inflammation and manage associated symptoms. Anti-inflammatory medications, such as corticosteroid eye drops, can help reduce swelling and pain. Mydriatic drops can also help dilate the pupil and improve visual comfort.
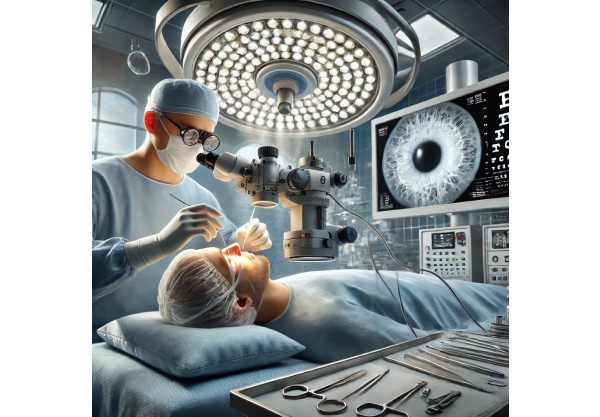
Surgical Treatment
Surgery is the only treatment for traumatic cataracts, especially when vision is severely impaired. The primary surgical procedure is cataract extraction and intraocular lens (IOL) implantation. The type and severity of the trauma determine the specific surgical approach.
- Phacoemulsification: This is the most common cataract removal technique, which involves using ultrasound energy to emulsify the opacified lens and then aspirating it out of the eye. An artificial IOL is used to restore vision. This method is preferable when the cataract is well-defined and there is little ocular damage.
- Extracapsular Cataract Extraction (ECCE): When the lens is too dense or the eye has been severely traumatized, ECCE may be used. This entails creating a larger incision to remove the cataract in one piece before implanting the IOL.
- Intracapsular Cataract Extraction (ICCE): This older technique is rarely used nowadays, but it may be required in extreme cases where both the lens and the surrounding capsule must be removed. The IOL is then positioned in front of the iris.
Post-operative Care
Postoperative care is critical for full recovery, and it includes the use of antibiotic and anti-inflammatory eye drops to prevent infection and inflammation. Patients should avoid strenuous activities, wear protective eyewear, and schedule regular follow-up appointments to monitor healing and ensure proper IOL positioning.
Innovative Techniques for Treating Traumatic Cataract
Recent advancements in traumatic cataract treatment have significantly improved patient outcomes by providing more precise, minimally invasive, and highly effective options. These innovations cover a wide range of topics, including surgical techniques, intraocular lens technology, and adjunct therapies.
Femtosecond Laser Assisted Cataract Surgery (FLACS)
Femtosecond laser-assisted cataract surgery (FLACS) marks a significant improvement in cataract surgery precision and safety. This technology employs a laser to perform critical steps of cataract surgery, including corneal incisions, capsulotomy, and lens fragmentation. Benefits of FLACS include:
- Precision: The laser makes highly accurate and reproducible incisions, resulting in better surgical outcomes.
- Safety: FLACS reduces the need for manual incisions and ultrasonic energy, lowering the risk of complications and eye trauma.
- Efficiency: The laser softens the lens beforehand, making it easier to remove and shortening the overall surgery time.
FLACS is especially useful in cases of traumatic cataracts, where precision is critical to preventing further damage to the already injured eye.
Advanced intraocular lenses (IOLs)
The development of advanced intraocular lenses (IOLs) has transformed cataract surgery outcomes, giving patients better visual acuity and reducing their need for glasses. New developments in IOL technology include:
- Multifocal and Extended Depth of Focus (EDOF) IOLs: These lenses offer clear vision at a variety of distances, improving overall visual quality and reducing the need for corrective lenses.
- Toric IOLs: Designed for patients with astigmatism, toric IOLs correct the refractive error and improve visual outcomes.
- Accommodative IOLs: These lenses mimic the eye’s natural focusing ability, resulting in improved near and distance vision.
These advanced IOLs are especially beneficial for patients with traumatic cataracts because they can treat not only the cataract but also any pre-existing refractive errors, providing complete visual rehabilitation.
Minimal Invasive Glaucoma Surgery (MIGS)
Traumatic cataracts are frequently associated with secondary glaucoma as a result of the injury’s increased intraocular pressure. Minimally invasive glaucoma surgery (MIGS) techniques have emerged as effective options for treating this complication in conjunction with cataract surgery. MIGS procedures, such as the iStent and the Xen Gel Stent, are designed to reduce IOP with minimal tissue disruption, providing benefits such as:
- Lower Surgical Risk: MIGS procedures require fewer incisions and cause less trauma to the eye than traditional glaucoma surgeries.
- Faster Recovery: Patients usually have shorter recovery times and fewer postoperative complications.
- Compatibility with Cataract Surgery: MIGS can be performed alongside cataract surgery, treating both conditions in the same procedure.
Biocompatible Ocular Devices
The development of biocompatible ocular devices has improved the management of traumatic cataracts and associated injuries. These devices, such as artificial iris implants and capsular tension rings, help to stabilize the eye during and after surgery. Key advantages include:
- Enhanced Stability: Capsular tension rings help to maintain the lens capsule’s integrity, especially in cases of zonular weakness or trauma-related damage.
- Improved Aesthetics and Functionality: Artificial iris implants can restore the appearance and function of the eye when the natural iris is damaged, thereby improving both cosmetic and visual outcomes.
Gene Therapy & Regenerative Medicine
Emerging fields like gene therapy and regenerative medicine show promise for the future of traumatic cataract treatment. Researchers are investigating the potential of gene editing technologies such as CRISPR-Cas9 to repair trauma-induced genetic damage and prevent cataract formation. Furthermore, stem cell therapy is being studied to regenerate damaged ocular tissues and restore normal lens function.
- Gene Therapy: By targeting specific genes involved in the development of traumatic cataracts, gene therapy attempts to prevent or reverse cataract formation at the molecular level.
- Stem Cell Therapy: Stem cell-based treatments may replace damaged lens cells, promoting the regeneration of a clear, functional lens.
Personalized Medicine
Personalized medicine is increasingly important in the treatment of traumatic cataracts. Advances in genetic testing and biomarker identification enable personalized treatment plans based on an individual’s genetic and biochemical profile. This approach may lead to:
- Customized Treatment Plans: By understanding a patient’s genetic predispositions and injury responses, clinicians can create more effective and personalized treatment plans.
- Enhanced Predictive Power: Personalized medicine can help predict the likelihood of developing traumatic cataracts following an injury, allowing for early intervention and prevention.
Artificial Intelligence, Machine Learning
Artificial intelligence (AI) and machine learning are transforming the field of traumatic cataract diagnosis and treatment. AI algorithms can analyze large datasets to identify patterns and predict outcomes, resulting in more accurate diagnoses and tailored treatment plans. Applications of artificial intelligence in traumatic cataract care include:
- Automated Diagnosis: AI-powered imaging systems can detect subtle changes in the lens and other ocular structures, allowing for timely and accurate diagnosis.
- Predictive Analytics: Machine learning models can predict the risk of complications and help guide decision-making in complex situations.
- Surgical Assistance: Artificial intelligence systems can help surgeons by providing real-time data and recommendations during cataract surgery, increasing precision and safety.
Telemedicine & Remote Monitoring
The integration of telemedicine and remote monitoring technologies is increasing access to traumatic cataract care, particularly in underserved communities. Telemedicine platforms allow for remote consultations, diagnoses, and follow-up care, reducing the need for in-person appointments. Benefits include:
- Increased Accessibility: Patients in remote or underserved areas can now access expert care without having to travel long distances.
- Continuity of Care: Remote monitoring enables continuous assessment of a patient’s condition, resulting in timely interventions and adjustments to treatment plans.
- Cost-Effectiveness: Telemedicine can lower healthcare costs by reducing the need for frequent in-person visits and hospitalizations.
Nanotechnology and Drug Delivery
Nanotechnology is transforming drug delivery in traumatic cataract treatment by enabling targeted and sustained release of therapeutic agents. Nanoparticles can be engineered to deliver drugs directly to the site of injury, increasing efficacy while decreasing side effects. Applications include:
- Targeted Drug Delivery: Nanoparticles can deliver anti-inflammatory and anti-fibrotic agents to the site of trauma, reducing inflammation and preventing scar formation. This targeted approach maximizes local drug concentrations while minimizing systemic exposure.
- Sustained Release Systems: Nanoparticles and other nanocarriers can be engineered to release therapeutic agents over time, reducing the need for frequent dosing and increasing patient compliance. These sustained release systems can be especially useful in reducing postoperative inflammation and avoiding secondary complications.
Bioengineered Ocular Tissues
Advances in tissue engineering have resulted in the creation of bioengineered ocular tissues, which show promise for repairing and regenerating damaged eye structures in traumatic cataract cases. Bioengineered corneas, lenses, and ocular tissues have the potential to restore normal function and appearance. Innovations in this field include the following:
- Corneal Grafts: Bioengineered corneal grafts made from stem cells and biomaterials can replace damaged corneal tissue while restoring transparency and vision. These grafts provide an alternative to traditional donor corneas, which are frequently in short supply.
- Lens Regeneration: Researchers are investigating the ability of bioengineered lens tissues to regenerate and replace damaged lenses, offering a more natural treatment for traumatic cataracts.
Neuroprotective Agents
Neuroprotective agents are being studied for their ability to protect and preserve the optic nerve and retinal cells after a traumatic eye injury. These drugs aim to prevent secondary damage and promote healing by targeting specific molecular pathways involved in cell survival and inflammation. The potential benefits include:
- Enhanced Recovery: Neuroprotective agents can help restore visual function by protecting retinal and optic nerve cells from damage and promoting regeneration.
- Reduced Complications: By preventing secondary injury processes, these agents can lower the risk of complications like retinal detachment and glaucoma.
Integrated Rehabilitation Programs
Rehabilitation is an essential part of the recovery process for patients with traumatic cataracts. Integrated rehabilitation programs that include physical therapy, occupational therapy, and vision therapy can significantly improve results. These programs focus on:
- Visual Rehabilitation: Techniques such as low-vision therapy and adaptive devices can assist patients in maximizing their remaining vision and adjusting to visual impairments.
- Physical Therapy: Patients recovering from traumatic injuries require exercises and therapies that improve coordination, balance, and overall physical health.
- Psychological Support: Counseling and support groups can assist patients in coping with the emotional and psychological consequences of vision loss and trauma.