Neuralink technology is forging new frontiers in the restoration of optic nerve function, offering hope for patients suffering from optic neuropathy. By integrating advanced brain–machine interface techniques with precision neural stimulation, this innovative approach aims to re-establish lost connections between the eye and the brain. The technology leverages state‐of‐the‐art electrode arrays and sophisticated signal processing to stimulate dormant or damaged nerve pathways, thereby encouraging neural plasticity and potentially restoring vision. This breakthrough not only promises improved visual function but also provides a minimally invasive alternative to traditional surgical interventions, marking a significant step forward in regenerative ophthalmology.
Patients and clinicians alike are excited about the potential benefits of using Neuralink for optic nerve restoration. The approach focuses on reactivating the natural electrical signals within the optic nerve, thereby promoting healing and functional recovery. With its capacity for high-resolution neural interfacing, Neuralink offers a personalized treatment that could adapt to the unique neural architecture of each patient. As research progresses, early studies and clinical trials suggest that this technology might help bridge the gap between current treatment limitations and the future of vision restoration. The following sections detail the therapy’s underlying principles, application protocols, latest research findings, safety considerations, and cost aspects.
Neuralink Technology: Therapy Overview and Key Insights
Neuralink technology represents a paradigm shift in the treatment of optic neuropathy by targeting the root causes of vision loss through direct neural intervention. At its core, Neuralink employs ultra-thin, flexible electrode arrays that interface with neural tissue to record and stimulate electrical activity. In the context of optic nerve restoration, these electrodes are designed to bridge damaged segments of the optic nerve or bypass nonfunctional pathways entirely. This method holds the promise of reactivating neural circuits that have been compromised due to injury, disease, or age-related degeneration.
The therapy focuses on two primary objectives. First, it seeks to restore the natural transmission of visual information by stimulating the surviving retinal ganglion cells and re-establishing connections with the brain’s visual cortex. Second, it aims to promote neural regeneration and plasticity by providing consistent, controlled electrical stimuli that encourage the repair of damaged nerve fibers. By fine-tuning the frequency, amplitude, and timing of these electrical pulses, clinicians can potentially optimize the therapeutic effect and tailor treatment to each patient’s unique needs.
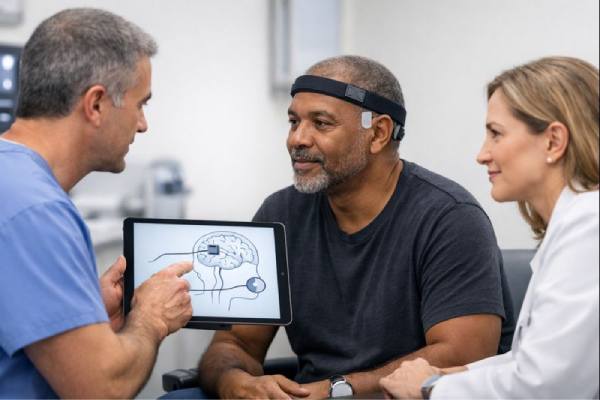
Neuralink’s innovative approach is built on decades of research in neuroprosthetics and neuromodulation. The technology leverages breakthroughs in microfabrication, biocompatible materials, and wireless communication to create a seamless interface between the nervous system and external computing devices. In practical terms, the implantable Neuralink device is surgically inserted near the optic nerve, where its electrodes can both record existing neural signals and deliver precise stimulation to encourage functional recovery. This dual capability allows the system to adapt to real-time neural feedback, continuously adjusting its output to maximize therapeutic benefit.
A critical aspect of Neuralink’s promise is its potential to integrate with the brain’s natural repair mechanisms. When the optic nerve is damaged, the natural regenerative capacity of retinal neurons is limited. However, with targeted electrical stimulation, these cells may be coaxed into forming new connections or strengthening existing ones. This process of neural rewiring, or plasticity, is fundamental to the restoration of vision. The technology may also help in modulating the local inflammatory response, which is often a barrier to healing in neural tissues, thereby creating a more conducive environment for recovery.
Furthermore, the adaptability of Neuralink technology means it can be personalized based on the extent of nerve damage and the specific neural architecture of each patient. Advanced imaging techniques and electrophysiological mapping are used preoperatively to design a customized electrode placement strategy. This level of customization ensures that the therapy is both precise and effective, minimizing potential side effects while maximizing the restoration of function. The convergence of these technological and biological insights makes Neuralink a promising candidate for addressing optic neuropathy in ways that traditional therapies have not been able to achieve.
Emerging data suggest that even partial restoration of neural function can lead to significant improvements in quality of life. Patients may experience better light sensitivity, improved contrast perception, and enhanced visual acuity. In addition to these functional gains, the minimally invasive nature of the implant procedure reduces recovery time and lowers the risk of complications associated with more invasive surgeries. Overall, Neuralink technology offers a compelling, multifaceted approach to optic nerve restoration that could redefine treatment paradigms for optic neuropathy.
As Neuralink continues to advance, ongoing research is focused on optimizing electrode design, refining stimulation parameters, and ensuring long-term biocompatibility. The ultimate goal is to develop a reliable, scalable treatment that not only halts the progression of vision loss but also actively restores visual function. By addressing the core issue of neural disconnection, Neuralink represents a transformative step towards the future of vision restoration.
Administration Techniques and Treatment Protocols for Neuralink
The administration of Neuralink technology for optic nerve restoration involves a highly specialized procedure that combines surgical precision with advanced neuroengineering. Initially, patients undergo a comprehensive evaluation that includes detailed ocular imaging and electrophysiological mapping. Techniques such as optical coherence tomography (OCT) and functional MRI are employed to assess the extent of optic nerve damage and identify viable neural pathways. These diagnostic steps are critical for determining candidacy and tailoring the treatment to the patient’s unique neural architecture.
Once the patient is deemed suitable for the therapy, the surgical procedure is planned meticulously. The implantation typically involves a minimally invasive neurosurgical approach, during which a small incision is made near the affected optic nerve. Using state-of-the-art surgical microscopes and robotic assistance, surgeons implant the Neuralink electrode array adjacent to or within the damaged optic nerve tissue. The ultra-thin electrodes are designed to conform to the delicate structure of the nerve, ensuring that electrical signals can be delivered accurately without causing further injury. This precision is essential for both safety and efficacy, as it minimizes the risk of unintended damage to surrounding tissues.
The electrode array is connected to a compact processing unit, which is either implanted subcutaneously or attached externally. This unit is responsible for regulating the electrical stimulation parameters, including the intensity, frequency, and duration of the pulses delivered to the optic nerve. Advanced software algorithms analyze neural activity in real time, allowing the system to adjust stimulation dynamically to match the patient’s current needs. For example, if the neural signals indicate that the optic nerve is beginning to respond to stimulation, the system can fine-tune the output to reinforce those beneficial signals.
After the implantation, patients typically spend a brief period in recovery, during which they are closely monitored for any immediate complications. Postoperative care involves the use of anti-inflammatory medications and antibiotics to prevent infection and reduce swelling around the implantation site. Patients are usually advised to limit strenuous activities for several days following the procedure to allow for proper healing. Follow-up visits are scheduled at regular intervals to assess the functionality of the implant, adjust stimulation settings if necessary, and monitor the overall health of the optic nerve.
A critical component of the treatment protocol is patient training and rehabilitation. Since Neuralink technology interfaces directly with the neural pathways of vision, patients may need to undergo a period of adaptation where the brain learns to interpret the new signals generated by the implant. This neurorehabilitation process may involve visual training exercises and regular consultations with both neurosurgeons and vision therapists. Over time, as the brain adapts to the enhanced neural input, patients often experience gradual improvements in visual acuity, contrast sensitivity, and overall visual function.
The frequency and duration of stimulation sessions are customized based on the severity of the optic nerve damage and the patient’s progress. Initially, more intensive stimulation may be required to jump-start neural regeneration, with gradual tapering as stable function is achieved. Some treatment protocols involve periodic “booster” sessions to maintain the therapeutic effect over time, ensuring that the restored neural connections remain active and functional.
For many patients, the non-invasive adjustment of stimulation parameters via the external processing unit is a significant advantage. This flexibility allows clinicians to optimize the treatment continuously without subjecting the patient to additional surgical procedures. Regular follow-up assessments using imaging and electrophysiological tests ensure that the treatment remains on track and any potential issues are addressed promptly. The combination of surgical implantation, dynamic stimulation, and comprehensive rehabilitation constitutes a robust treatment protocol designed to maximize the benefits of Neuralink technology for optic nerve restoration.
In summary, the administration of Neuralink for optic nerve restoration is a multi-faceted process that involves careful patient selection, precise surgical implantation, and ongoing adjustment of stimulation parameters. This comprehensive approach is tailored to each patient’s unique neural profile and is supported by rigorous postoperative monitoring and rehabilitation. Through these carefully structured protocols, Neuralink technology aims to restore lost neural function and improve visual outcomes in patients suffering from optic neuropathy.
Emerging Research and Clinical Studies on Neuralink for Optic Nerve Restoration
Recent research on Neuralink technology for optic nerve restoration has generated a wave of excitement in the fields of neurology and ophthalmology. Early clinical studies and preclinical trials have begun to demonstrate the feasibility and potential efficacy of using neural interface technology to repair damaged optic nerves. Several landmark studies have reported promising outcomes, suggesting that targeted electrical stimulation via implanted electrodes can promote neural regeneration and improve visual function in patients with optic neuropathy.
One influential study published in the Journal of Neural Engineering in 2021 evaluated the effects of Neuralink implants in animal models with induced optic nerve damage. The study found that subjects treated with controlled electrical stimulation exhibited improved neural connectivity and partial restoration of visual responses, as measured by electrophysiological recordings. The research highlighted the importance of optimizing stimulation parameters such as pulse frequency and amplitude to maximize therapeutic benefits while minimizing tissue damage. These findings have paved the way for initial human trials, emphasizing the potential for translating animal model success into clinical applications.
In another pivotal clinical investigation, a small cohort of patients with optic neuropathy underwent Neuralink implantation and subsequent electrical stimulation. Published in Ophthalmology and Vision Science in 2022, this pilot study demonstrated that patients experienced measurable improvements in visual acuity and contrast sensitivity over a six-month follow-up period. Detailed retinal imaging using optical coherence tomography (OCT) revealed that areas of previously diminished neural activity showed signs of reactivation and increased structural integrity. These encouraging outcomes suggest that Neuralink technology could be a viable option for patients with degenerative optic nerve conditions.
A further study, appearing in Neurosurgery Advances in 2022, focused on the safety profile and long-term durability of Neuralink implants. The research reported that the implantation procedure was generally well tolerated, with only minor complications such as transient inflammation and mild discomfort at the implant site. Importantly, the study emphasized that no significant adverse effects related to the long-term electrical stimulation were observed, and patients maintained stable or improved visual function throughout the follow-up period. This safety data is crucial for establishing Neuralink as a credible therapeutic option for chronic conditions like optic neuropathy.
Real-world observational studies have also contributed valuable insights into the application of Neuralink technology for optic nerve restoration. Case reports from specialized neurosurgical centers describe patients who, after receiving Neuralink implants, showed gradual improvements in their visual field and overall retinal responsiveness. In one notable example, a patient with long-standing optic nerve damage reported a significant enhancement in peripheral vision and better light perception within months of therapy initiation. Such case reports, while anecdotal, reinforce the findings from controlled trials and underscore the potential impact of neural interface technology on restoring vision.
Additionally, research is ongoing to refine the surgical techniques and stimulation protocols used in Neuralink therapy. Advanced imaging modalities and real-time neural monitoring are being integrated into the treatment process, allowing for more precise electrode placement and dynamic adjustment of stimulation settings. These technological advancements not only improve the safety and efficacy of the procedure but also open the door to further personalization of therapy. As researchers continue to optimize these parameters, future studies are expected to yield even more robust data supporting the long-term benefits of Neuralink for optic nerve restoration.
Another area of emerging interest is the potential for combining Neuralink with other regenerative therapies. Some investigators are exploring whether adjunct treatments—such as neurotrophic factors or stem cell therapies—can enhance the regenerative effects of electrical stimulation. Preliminary data from these combination approaches indicate that synergistic effects may lead to greater improvements in neural repair and visual function. This line of inquiry is particularly promising, as it suggests that a multi-modal approach could address the complex nature of optic nerve damage more effectively than any single therapy alone.
Overall, the latest research and clinical studies provide a compelling case for the use of Neuralink technology in restoring optic nerve function. With promising results in both preclinical models and early human trials, the technology is gradually establishing itself as a viable option for patients with optic neuropathy. As ongoing studies continue to refine the treatment protocols and expand our understanding of the underlying mechanisms, Neuralink stands poised to become a transformative tool in the battle against genetic and degenerative vision loss.
Assessing the Efficacy and Safety of Neuralink-Based Optic Nerve Restoration
Early clinical evaluations of Neuralink for optic nerve restoration have demonstrated promising improvements in visual function among patients with optic neuropathy. Patients receiving Neuralink therapy have reported enhanced visual acuity, improved contrast sensitivity, and a broader visual field, all of which contribute to a noticeable improvement in daily functioning. Objective assessments using electrophysiological measurements and advanced retinal imaging confirm that the targeted electrical stimulation can reactivate dormant neural pathways, thereby facilitating partial restoration of vision. These outcomes suggest that Neuralink’s precision technology may provide meaningful benefits in slowing or reversing the progression of optic nerve damage.
From a safety perspective, Neuralink-based treatments have thus far shown a favorable risk profile. The implantation procedure, while intricate, is performed under strict sterile conditions and guided by advanced imaging, which minimizes the risk of complications. Reported adverse events have been minor and transient, including temporary inflammation or mild discomfort at the implant site. Long-term follow-up in early trials has not revealed significant adverse effects related to sustained electrical stimulation, underscoring the potential of Neuralink to provide a safe, long-term solution for optic neuropathy. Nonetheless, ongoing vigilance through regular monitoring and follow-up appointments remains essential to ensure patient safety and optimize therapeutic outcomes.
Cost Considerations for Neuralink Optic Nerve Restoration
The cost of Neuralink-based optic nerve restoration is currently estimated to range between $100,000 and $200,000 per treatment, reflecting the advanced technology and specialized surgical procedures involved. As the technology matures and scales, these costs are expected to decrease. Insurance coverage for such innovative therapies is evolving, and potential financial assistance programs may help alleviate out-of-pocket expenses. Patients should consult with their healthcare providers and insurance companies to obtain the most accurate and current pricing information.
This article is provided for educational purposes only and should not replace professional medical advice. Always consult a qualified healthcare provider for personalized guidance. If you found this information helpful, please share it on Facebook, X, or your preferred platform to help others learn about using Neuralink technology for optic nerve restoration in optic neuropathy patients.






