What is sickle cell retinopathy?
Sickle cell retinopathy is a serious ocular condition that affects people who have sickle cell disease (SCD), a genetic blood disorder defined by the production of abnormal hemoglobin known as hemoglobin S. This condition causes red blood cells to become rigid and crescent-shaped, limiting their ability to navigate small blood vessels and leading to a variety of complications, including those affecting the eyes. Sickle cell retinopathy develops when these malformed red blood cells obstruct the tiny blood vessels in the retina, which is the light-sensitive tissue at the back of the eye that controls vision.
The retina requires a constant supply of oxygen-rich blood to function properly. Ischemia (lack of blood flow) and subsequent neovascularization (abnormal blood vessel growth) occur when sickled cells block the retinal blood vessels. These fragile, new vessels can easily bleed, resulting in vitreous hemorrhage and retinal detachment, both of which are major causes of vision loss in sickle cell retinopathy patients. Symptoms of this condition may include floaters, blurred vision, and, in severe cases, sudden vision loss.
Sickle cell retinopathy is typically divided into two stages: nonproliferative and proliferative. The non-proliferative stage is characterized by the occlusion of retinal vessels and the formation of “salmon patch” hemorrhages and “black sunburst” lesions, whereas the proliferative stage is distinguished by the formation of abnormal blood vessels and fibrovascular tissue, which can result in tractional retinal detachments. Early detection and treatment are critical for preventing progression to the proliferative stage and preserving vision in patients.
Traditional Approaches to Sickle Cell Retinopathy Management
Sickle cell retinopathy requires a multidisciplinary approach involving ophthalmologists, hematologists, and primary care physicians. The primary goals of treatment are to control the underlying sickle cell disease, monitor the progression of retinopathy, and avoid or manage complications that could impair vision. Medical therapy, laser photocoagulation, and surgical interventions are all common treatment options.
Medical treatment focuses on managing sickle cell disease to reduce the frequency of vaso-occlusive crises and hemolytic events, which can worsen retinopathy. Hydroxyurea, a medication that boosts fetal hemoglobin production, is frequently used to reduce the number of sickling episodes. Furthermore, blood transfusions may be used to reduce the proportion of sickle cells in the bloodstream, improving blood flow and oxygen delivery to the retina. Pain management, hydration, and infection control are all important aspects of sickle cell disease treatment.
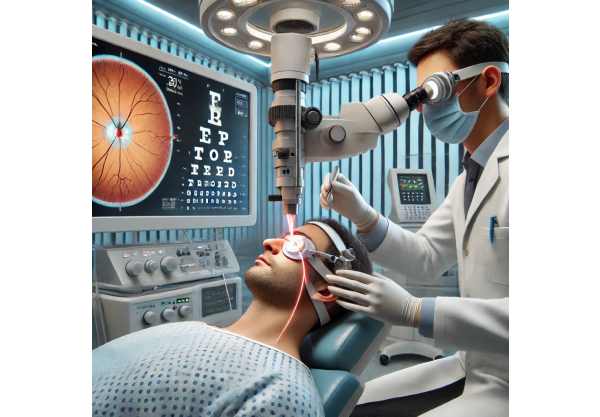
Laser photocoagulation is the standard treatment for proliferative sickle cell retinopathy. This procedure uses a laser to create small burns in the peripheral retina, which help to shrink abnormal blood vessels and prevent further neovascularization. Laser photocoagulation reduces the retina’s oxygen demand, which reduces the stimulus for abnormal vessel growth and the risk of vitreous hemorrhage and retinal detachment. The procedure is typically performed as an outpatient and can be repeated as needed.
In severe cases of proliferative sickle cell retinopathy, surgical procedures such as vitrectomy may be required. Vitrectomy is a surgical procedure that involves removing the vitreous gel from the eye in order to clear any blood that has leaked from abnormal vessels and relieve traction on the retina. In patients with vitreous hemorrhage or retinal detachment, this procedure can help restore vision. Surgery, on the other hand, carries risks such as infection and additional retinal damage and is typically considered when less invasive treatments fail.
Regular monitoring and follow-up are critical components of managing sickle cell retinopathy. Patients with sickle cell disease should have regular eye exams, including dilated fundus examinations and imaging studies like optical coherence tomography (OCT) and fluorescein angiography, to detect early signs of retinopathy and track disease progression. Early intervention can greatly improve outcomes and prevent severe vision loss in these patients.
Advanced Treatments for Sickle Cell Retinopathy
Recent advances in the understanding and treatment of sickle cell retinopathy have resulted in the development of novel therapeutic approaches, providing hope for better management and outcomes. These cutting-edge innovations cover a wide range of strategies, including gene therapy, biologic agents, advanced imaging techniques, and personalized medicine, all of which contribute to more precise and effective treatment of this complex condition.
Genetic Therapy
Gene therapy is a promising field of study for the treatment of sickle cell disease and its complications, including retinopathy. Advances in gene editing technologies, such as CRISPR-Cas9, have allowed researchers to target and correct the genetic mutations that cause sickle cell disease. By editing the genes of hematopoietic stem cells to produce normal hemoglobin rather than hemoglobin S, gene therapy has the potential to provide a long-term cure for sickle cell disease and prevent the development of sickle cell retinopathy.
One method of gene therapy involves inserting a healthy copy of the beta-globin gene into the patient’s hematopoietic stem cells via viral vectors. These modified stem cells are then reintroduced into the patient’s body, where they produce red blood cells containing normal hemoglobin. Clinical trials have yielded promising results, with patients reporting fewer vaso-occlusive crises and better overall health. As gene therapy advances, it has the potential to eradicate the underlying cause of sickle cell retinopathy and provide a long-term solution for affected individuals.
Biological Agents
Biologic agents are a new type of therapy that targets specific pathways in the pathophysiology of sickle cell disease and its ocular complications. The FDA has approved L-Glutamine as a treatment for sickle cell disease. L-Glutamine works by lowering oxidative stress in red blood cells, reducing the frequency of vaso-occlusive crises and improving blood flow to the retina. This agent has shown promise in slowing the progression of sickle cell retinopathy and saving patients’ vision.
Another biologic agent, voxelotor, is a hemoglobin modulator that increases hemoglobin’s affinity for oxygen, lowering hemolysis and improving blood flow. Voxelotor has shown efficacy in reducing the severity of sickle cell disease and may be useful in preventing or slowing the progression of sickle cell retinopathy. Current research is looking into the use of additional biologic agents that target specific inflammatory and vascular pathways involved in the development of retinopathy.
Advanced Imaging Techniques
Imaging advances have transformed the diagnosis and treatment of sickle cell retinopathy by allowing for detailed visualization of the retinal vasculature and precise monitoring of disease activity. Optical coherence tomography angiography (OCTA) is a non-invasive imaging modality that visualizes blood flow in the retina and choroid, revealing important information about the disease’s severity and activity level. OCTA can detect subtle changes in the vasculature that may indicate early disease progression or response to treatment, allowing for timely intervention and better outcomes.
Adaptive optics (AO) is another innovative imaging technique that allows for high-resolution imaging of retinal and choroidal structures at the cellular level. AO improves the ability to detect and monitor microscopic changes in the retina and choroid, revealing the pathophysiology of sickle cell retinopathy and guiding treatment decisions. The addition of AO to other imaging modalities, such as OCT and fundus autofluorescence, improves the accuracy and comprehensiveness of disease assessment.
Anti-VEGF Therapies
Anti-vascular endothelial growth factor (anti-VEGF) therapy has become an essential component in the treatment of a variety of retinal vascular diseases, including diabetic retinopathy and age-related macular degeneration. Recent studies have looked into the potential of anti-VEGF agents in the treatment of proliferative sickle cell retinopathy. These drugs work by inhibiting the activity of VEGF, a protein that encourages the formation of abnormal blood vessels.
Bevacizumab and ranibizumab, two anti-VEGF agents, have shown promise in clinical trials to treat sickle cell retinopathy. Intravitreal injections of these agents can reduce neovascularization, lower the risk of vitreous hemorrhage, and prevent retinal detachments. Anti-VEGF therapy is a less invasive alternative to laser photocoagulation and surgery, with the possibility of fewer side effects and improved retinal function.
Personalized Medicine
The rise of personalized medicine has the potential to change the treatment landscape for sickle cell retinopathy by tailoring therapies to each patient’s genetic and molecular profile. Advances in genomics, proteomics, and metabolomics are allowing for a better understanding of disease mechanisms and the identification of biomarkers that can inform treatment decisions. Personalized medicine approaches seek to maximize treatment efficacy, reduce side effects, and improve overall patient outcomes.
For example, pharmacogenomics, the study of how genes influence an individual’s drug response, can aid in identifying patients who are more likely to benefit from specific therapies or who are at risk of adverse reactions. This information can be used to tailor treatment plans and adjust dosages for the best possible outcomes. As personalized medicine advances, it holds the promise of more effective and targeted therapies for sickle cell retinopathy, ultimately improving affected people’s quality of life.






