Neovascularization of the vitreous is a serious ocular condition characterized by the formation of new, abnormal blood vessels in the vitreous humor, a gel-like substance that fills the eye. These new blood vessels are often fragile and prone to bleeding, resulting in complications like vitreous hemorrhage, retinal detachment, and vision loss. This condition is frequently caused by retinal ischemia, which occurs when there is insufficient blood flow and oxygen to the retina, resulting in the release of vascular endothelial growth factor. In order to compensate, VEGF stimulates the formation of new blood vessels.
Neovascularization of the vitreous is frequently associated with retinal diseases such as proliferative diabetic retinopathy, retinal vein occlusion, and sickle cell retinopathy. Patients may exhibit symptoms such as floaters, blurred vision, and, in severe cases, sudden vision loss due to hemorrhage. A thorough ophthalmic examination is required to determine the extent of neovascularization and associated retinal changes, which may include fundus photography, fluorescein angiography, and optical coherence tomography (OCT). Understanding the underlying mechanisms and risk factors is critical for successful management and treatment of this vision-threatening condition.
Traditional treatment of vitreous neovascularization
Managing and treating vitreous neovascularization requires a multifaceted approach that aims to reduce abnormal blood vessel growth, prevent complications, and preserve vision. Standard treatments include:
Medical Management
Medical treatment primarily focuses on inhibiting VEGF activity to prevent the formation of new abnormal blood vessels. This is accomplished through:
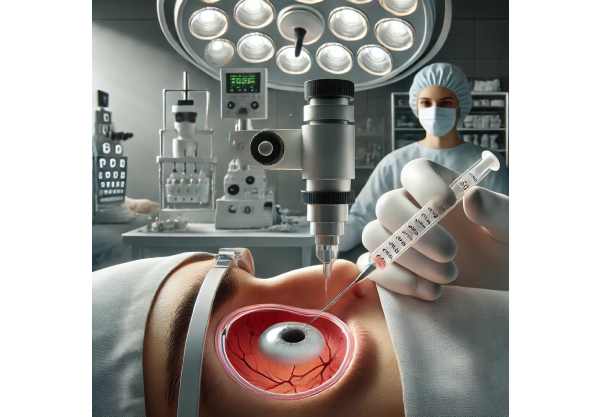
- Anti-VEGF injections: Treatment consists primarily of intravitreal injections of anti-VEGF agents such as bevacizumab (Avastin), ranibizumab (Lucentis), and aflibercept (Eylea). These agents bind to VEGF, which inhibits its effects and reduces neovascularization. Regular injections are frequently required to maintain therapeutic levels and slow disease progression.
- Corticosteroids: In cases where inflammation is significant, intravitreal corticosteroid injections (e.g., triamcinolone acetonide) may be used. Corticosteroids reduce inflammation and may have an additional effect on neovascularization.
Laser Treatments
Laser therapy is an important part of treatment, especially for addressing the underlying ischemic retinal disease.
- Panretinal Photocoagulation (PRP): PRP uses laser burns on the peripheral retina to reduce ischemic drive and subsequent VEGF production. This treatment is especially effective in cases of proliferative diabetic retinopathy and other ischemic retinal diseases.
- Focal Laser Therapy For localized neovascularization, focal laser treatment can be used to target and ablate abnormal blood vessels, lowering the risk of vitreous hemorrhage.
Surgical Interventions
In advanced cases with significant complications, surgical intervention may be required.
- Vitriectomy: This surgical procedure involves the removal of the vitreous humor and its replacement with a saline solution or gas bubble. Vitrectomy is commonly used to treat vitreous hemorrhage, remove fibrovascular tissue, and repair retinal detachments. It can also help to reduce neovascular membrane-induced traction on the retina.
- Endolaser Photocoagulation: During vitrectomy, endolaser photocoagulation can be used to treat neovascularization and stabilize the retina.
Innovative Approaches to Vitreous Neovascularization
Recent advances in the treatment of vitreous neovascularization have significantly improved patients’ prognoses. These innovations include novel pharmacological therapies, advanced surgical techniques, and cutting-edge technologies that aim to improve management effectiveness and safety.
Extended-Release Drug Delivery System
Extended-release drug delivery systems represent a significant advance in the treatment of vitreous neovascularization. These systems provide sustained release of medications, which improves treatment adherence and efficacy
- Anti-VEGF Implants with Sustained Release Devices like the Port Delivery System (PDS) with ranibizumab are intended to release anti-VEGF medication over several months. This reduces the need for frequent intravitreal injections, resulting in more consistent drug levels and better neovascularization management. Clinical trials have shown that these implants are effective at maintaining vision and reducing treatment burden.
- Biodegradable Implants: Researchers are working on biodegradable implants that release corticosteroids or anti-VEGF agents gradually over time. These implants provide a long-term therapeutic effect while reducing the need for repeated injections, which can be difficult for patients.
Genetic Therapy
Gene therapy shows great promise for the future of neovascularization treatment. By introducing or modifying genes within the eye, gene therapy can target the underlying causes of abnormal blood vessel growth.
- VEGF Inhibition: Researchers are looking into gene therapies that deliver anti-VEGF genes to the eye, resulting in long-term suppression of VEGF activity. This approach may provide a more long-term solution than repeated anti-VEGF injections while also lowering the risk of neovascularization recurrence.
- Regenerative Approaches: Gene therapies aimed at improving retinal health and function are also under investigation. These therapies, which enhance the retina’s natural regenerative processes, may help restore normal vascularization and improve visual outcomes.
Advancements in Vitrectomy Techniques
Recent advances in vitrectomy techniques have increased the safety and efficacy of this critical surgical intervention:
- Microincision Vitrectomy Surgery (MIVS): MIVS uses smaller gauge instruments (23-, 25-, or 27-gauge) to perform vitrectomy. This minimally invasive approach reduces surgical trauma, accelerates recovery, and lowers the risk of complications. MIVS is especially useful for patients with neovascularization complications like vitreous hemorrhage and retinal detachment.
- Advanced Visualization Systems: Enhanced visualization systems, such as high-definition 3D imaging and intraoperative OCT, offer surgeons real-time, detailed views of the retina and vitreous. These systems increase the precision of surgical interventions, allowing for more effective treatment of neovascularization and its complications.
Combination Therapies
Combining multiple treatment modalities has shown promise in better managing vitreous neovascularization.
- Anti-VEGF/Steroid Combination: The combination of anti-VEGF agents and corticosteroids can have a synergistic effect, reducing inflammation and neovascularization more effectively than either alone. This combination approach is especially useful in cases involving significant inflammatory components.
- Laser and Pharmacological Treatment: Combining laser treatments and pharmaceutical interventions can improve treatment outcomes. PRP, for example, when combined with anti-VEGF injections, can more effectively reduce ischemic drive and control neovascularization.
Personalized Medical Approaches
Personalized medicine is becoming more commonly used in the treatment of vitreous neovascularization. Personalized medicine, which tailors therapies to individual patient characteristics, can improve treatment outcomes.
- Pharmacogenomics: Genetic testing can identify patients who are more likely to respond to certain medications, allowing for more individualized treatment plans. This approach maximizes therapeutic efficacy while minimizing side effects, ensuring that patients receive the best possible care based on their genetic profile.
- Biomarker identification: There is ongoing research to identify biomarkers that predict disease progression and treatment response. These biomarkers can help guide treatment decisions by identifying the most appropriate therapies for each patient and providing more accurate disease activity monitoring.
Telemedicine & Remote Monitoring
The use of telemedicine and remote monitoring technologies has improved access to care and disease management for patients with vitreous neovascularization.
- Remote Imaging and Consultations: Teleophthalmology enables regular patient monitoring through remote imaging and virtual consultations, eliminating the need for frequent in-person visits. This is especially beneficial for patients with mobility issues or who live in remote areas.
- Home-Based Monitoring Devices: Devices that allow for home monitoring of visual acuity and other ocular parameters can aid in the early detection of disease progression. These devices provide healthcare providers with real-time data, allowing for more timely interventions and improved disease management.
Future Directions in Research
Ongoing research is looking into new ways to treat vitreous neovascularization, with several promising directions:
- Nanoparticle-Based Therapy: Nanoparticles can deliver medications directly to specific tissues, increasing drug efficacy and reducing systemic side effects. This technology has the potential to revolutionize the treatment of ocular diseases such as vitreous neovascularization.
- Stem Cell Treatment: Stem cell treatments aim to regenerate damaged retinal and vascular tissues, potentially restoring vision. While still in the experimental stage, this approach shows great promise for the future.
- Artificial Intelligence (AI) for Diagnostics: Artificial intelligence algorithms are being developed to analyze retinal images and detect early signs of neovascularization. These tools can help with diagnosis and monitoring, increasing the accuracy and efficiency of disease management.






