Scleromalacia perforans is a severe, progressive form of scleritis that causes thinning and degeneration of the sclera, the white outer layer of the eye, with no significant inflammation. This condition is frequently associated with autoimmune diseases, specifically rheumatoid arthritis. Unlike other types of scleritis, scleromalacia perforans usually causes only minor pain and redness, which can lead to a delay in diagnosis and treatment.
Scleromalacia perforans’ pathophysiology is characterized by chronic autoimmune destruction of scleral tissue. Autoantibodies and immune complexes target the sclera, degrading collagen and extracellular matrix components. Over time, this causes the sclera to thin and areas of scleral melting or perforation to form, compromising the eye’s structural integrity.
Patients with scleromalacia perforans frequently report blurred vision, increased sensitivity to light (photophobia), and a noticeable thinning or bluish discoloration of the sclera. In severe cases, the condition can cause complications such as uveal prolapse, in which the inner layers of the eye bulge through the weakened sclera, and secondary infections.
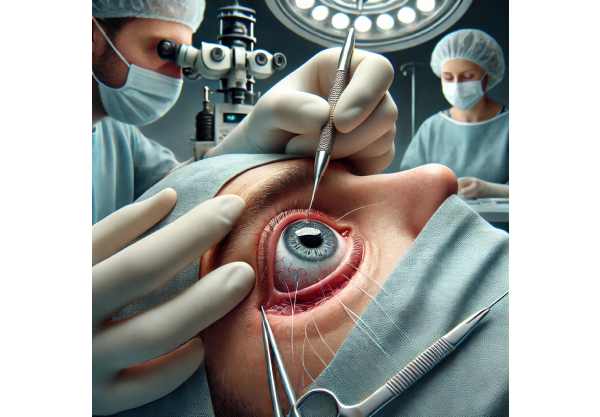
A thorough clinical examination by an ophthalmologist, including slit-lamp biomicroscopy to assess the extent of scleral thinning, is typically required to diagnose scleromalacia perforans. Imaging studies, such as ultrasound biomicroscopy (UBM) and optical coherence tomography (OCT), are critical for determining the extent of scleral involvement and making treatment decisions. Laboratory tests to detect underlying autoimmune conditions, such as rheumatoid factor and anti-citrullinated protein antibodies (ACPAs), are also useful in the diagnostic process.
Standard Treatments for Scleromalacia Perforans
Scleromalacia perforans requires a multifaceted approach to management and treatment that focuses on controlling the underlying autoimmune disease, preserving scleral integrity, and avoiding complications. Given the severity and progression of the disease, early intervention and ongoing monitoring are critical.
- Systemic Immunosuppression: Because scleromalacia perforans is frequently associated with systemic autoimmune diseases, systemic immunosuppression is the primary treatment strategy. Corticosteroids, methotrexate, azathioprine, and mycophenolate mofetil are popular medications for controlling the underlying autoimmune response and slowing the progression of scleral thinning. Biologic agents like rituximab and infliximab may also be used in refractory cases.
- Topical Steroids and Immunomodulators: In addition to systemic treatment, topical steroids and immunomodulators can be applied directly to the eye to reduce inflammation and promote healing. However, because scleromalacia perforans has a low inflammatory component, their use is limited.
- Scleral Reinforcement Surgery: Surgical intervention is frequently required to strengthen the thinning sclera and prevent perforation. Scleral reinforcement surgery involves grafting materials such as donor sclera, fascia lata, or synthetic grafts onto the sclera’s weakened areas. This procedure aims to restore the eye’s structural integrity and prevent future complications. To achieve the best possible results, careful surgical planning and technique are required.
- Scleral Patch Grafting: Scleral patch grafting, like scleral reinforcement, involves applying a patch to the thinned sclera to provide additional support. This can be accomplished with autologous tissue (from the patient), allogeneic tissue (from a donor), or synthetic materials. Scleral patch grafting is frequently used in conjunction with systemic immunosuppression to improve long-term outcomes.
- Antibiotic Prophylaxis: If the sclera is significantly thinned and at risk of perforation, prophylactic antibiotics may be recommended to prevent secondary infections. This is especially important for patients who have a history of recurring infections or who are immunocompromised.
- Regular Monitoring and Follow-up: Patients with scleromalacia perforans require continuous monitoring by an ophthalmologist. Regular follow-up visits and imaging studies are required to monitor disease progression, adjust treatment plans, and detect complications early. Continuous collaboration with rheumatologists and other specialists is also required for effective autoimmune disease management.
- Patient Education and Support: It is critical to educate patients about the nature of scleromalacia perforans, the significance of treatment adherence, and the importance of regular monitoring. Support groups and counseling can also be helpful for patients dealing with this chronic condition.
Breakthrough Therapies for Scleromalacia Perforans
Recent advances in the understanding and treatment of scleromalacia perforans have resulted in novel therapies and diagnostic tools that are revolutionizing the management of this difficult disease. These cutting-edge innovations provide new hope for patients suffering from scleromalacia perforans in terms of outcomes and quality of life.
Advanced Immunomodulatory Therapies
The development of advanced immunomodulatory therapies has transformed the treatment of autoimmune diseases, including scleromalacia perforans. These therapies provide targeted approaches to immune modulation, resulting in effective control of the underlying autoimmune response with fewer side effects than traditional immunosuppressive agents.
- Biologic Agents: TNF inhibitors (infliximab, adalimumab) and B-cell depleting therapies (rituximab) have demonstrated significant efficacy in treating severe and refractory cases of scleromalacia perforans. These agents target specific immune system components, reducing inflammation and preventing additional scleral degradation. Clinical trials have shown that biologic agents can improve ocular outcomes and reduce the need for surgical interventions in patients with scleromalacia perforans.
- JAK Inhibitors: Janus kinase (JAK) inhibitors, including tofacitinib and baricitinib, are emerging as promising treatments for autoimmune diseases. These small molecules inhibit the JAK-STAT signaling pathway, which is critical for immune response. Early research suggests that JAK inhibitors can effectively reduce inflammation and scleral thinning in scleromalacia perforans, providing a new treatment option for patients who do not respond to standard immunosuppressive therapies.
Regenerative Medicine and Tissue Engineering
Advances in regenerative medicine and tissue engineering are enabling novel approaches to restoring scleral integrity in patients with scleromalacia perforans.
- Stem Cell Therapy: Stem cells have the ability to regenerate damaged scleral tissue and promote healing. Mesenchymal stem cells (MSCs) possess immunomodulatory and regenerative properties, making them a promising treatment for scleromalacia perforans. Preclinical studies have demonstrated that MSCs can improve scleral repair and reduce inflammation. Clinical trials are currently underway to determine the safety and efficacy of stem cell therapy in scleromalacia perforans patients.
- Bioengineered Scleral Grafts: Tissue engineering techniques are being used to create bioengineered scleral grafts that have the same structural and functional properties as natural sclera. These grafts are made from biocompatible materials and cellular components, making them both long-lasting and effective for reinforcing thin sclera. Bioengineered scleral grafts have the potential to improve biocompatibility and reduce rejection risk when compared to traditional graft materials.
Advanced Imaging and Diagnostic Tools
Accurate and timely diagnosis is essential for effective scleromalacia perforans management. Imaging technology advancements improve the detection and monitoring of scleral thinning and associated ocular abnormalities.
- High-resolution optical coherence tomography (OCT): OCT can produce high-resolution cross-sectional images of the sclera and other ocular structures. Advanced OCT technologies, such as swept-source OCT and enhanced-depth imaging OCT, provide detailed views of scleral thinning and structural changes. These tools are extremely useful for diagnosing and monitoring scleromalacia perforans, making treatment decisions, and detecting complications early on.
- Ultrasound Biomicroscopy (UBM): UBM is a high-frequency ultrasound technique that produces detailed images of the eye’s anterior segment, which includes the sclera. UBM is especially useful for determining the extent of scleral thinning and planning surgical interventions as needed. Advances in UBM technology improve image resolution and diagnostic accuracy, allowing for more effective scleromalacia perforans management.
- Confocal Microscopy: Confocal microscopy allows for detailed, in-vivo imaging of the ocular surface and anterior segment at the cellular level. This technology can be used to examine the characteristics of scleral tissue in scleromalacia perforans, providing insights into the disease’s pathophysiology and aiding in the differentiation of infectious and non-infectious causes of scleral thinning.






