Scleral ectasia is a rare, progressive ocular condition that causes the sclera, the eye’s white outer layer, to thin and bulge. This condition can cause significant visual impairment and discomfort. The sclera supports and protects the eye, and any compromise in its integrity can lead to serious complications such as scleral rupture, retinal detachment, and secondary glaucoma.
Scleral ectasia may be congenital or acquired. Congenital conditions are frequently associated with connective tissue disorders such as Marfan syndrome, Ehlers-Danlos syndrome, and osteogenesis imperfecta. Acquired scleral ectasia can occur as a result of severe myopia, trauma, inflammatory diseases, or surgical procedures such as scleral buckling to repair retinal detachments. Patients with scleral ectasia typically exhibit symptoms such as decreased vision, eye pain, and visible changes in the shape of the eye.
A comprehensive eye examination is required to diagnose scleral ectasia, which includes visual acuity tests, slit-lamp examination, and imaging techniques such as ultrasound biomicroscopy (UBM) and anterior segment optical coherence tomography (AS-OCT). These imaging modalities assist in determining the extent of scleral thinning and deformation. Early diagnosis and management are critical for preventing progression and promptly addressing any complications. Because the condition is so complex, treatment frequently necessitates a collaborative effort among ophthalmologists, rheumatologists, and other specialists.
Effective Management of Scleral Ectasia
Scleral ectasia management and treatment entails a combination of medical, surgical, and supportive approaches aimed at stabilizing the condition, preserving vision, and alleviating symptoms. The treatment strategy is based on the severity of the condition and the underlying cause.
- Medical Management: The initial treatment of scleral ectasia frequently includes addressing any underlying systemic or ocular conditions that contribute to scleral thinning. Anti-inflammatory medications, such as corticosteroids or immunosuppressive agents, may be required for patients with associated inflammatory diseases. Controlling inflammation is critical for preventing further scleral damage.
- Protective Eyewear: Patients at high risk of scleral rupture due to severe thinning should wear protective eyewear to avoid trauma. This is especially important for people with congenital connective tissue disorders, as the sclera is naturally weak.
- Scleral Reinforcement: Scleral reinforcement surgery is a traditional method for treating scleral ectasia. This entails grafting donor sclera, fascia lata, or synthetic materials onto the thinned sclera to provide structural support. This procedure may help prevent further thinning and lower the risk of complications. However, it is a complicated procedure that may not be appropriate for all patients.
- Scleral Patch Grafting: Scleral patch grafting, like scleral reinforcement, involves applying a patch to the thinned area to reinforce the sclera. This can be accomplished with autologous tissue (from the patient), allogeneic tissue (from a donor), or synthetic materials. The goal is to strengthen the scleral wall and prevent further progression.
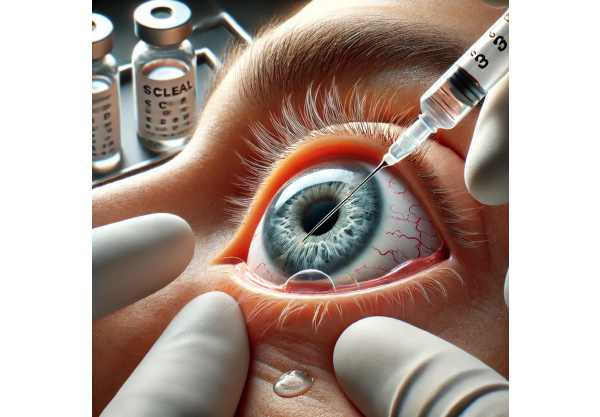
- Corneal Cross-Linking (CXL): Although primarily used for keratoconus, corneal cross-linking has also been investigated as a treatment for scleral ectasia. CXL works by applying riboflavin (vitamin B2) to the eye and activating it with ultraviolet light, which strengthens collagen fibers and increases tissue rigidity. This method shows promise in stabilizing scleral ectasia by improving the sclera’s biomechanical properties.
- Intraocular Pressure Management: High intraocular pressure (IOP) can aggravate scleral ectasia. Managing IOP with medications or surgical interventions is critical for reducing mechanical stress on the sclera. To reduce IOP, glaucoma medications like beta-blockers, prostaglandin analogs, and carbonic anhydrase inhibitors may be prescribed.
- Visual Rehabilitation: Patients with scleral ectasia frequently have significant vision impairment. Visual rehabilitation, such as corrective lenses, contact lenses, or low vision aids, can help improve visual function and overall quality of life. Rigid gas permeable (RGP) or scleral lenses are especially effective at improving visual acuity by forming a smooth refractive surface over the irregular cornea.
- Regular Monitoring: Continuous monitoring is essential for patients with scleral ectasia in order to detect changes in the condition or the onset of complications early. Regular eye exams, including imaging studies, aid in determining the efficacy of treatment and making necessary changes to the management strategy.
Advanced Scleral Ectasia Treatment Techniques
The treatment landscape for scleral ectasia is changing as new therapies and technologies become available. These cutting-edge innovations aim to improve the management of scleral ectasia, giving patients new hope for better outcomes and a higher quality of life.
Gene Therapy: Addressing the Genetic Basis
Given that some cases of scleral ectasia are associated with genetic disorders, gene therapy represents a promising approach to addressing the underlying cause of the condition. Gene therapy is the delivery of functional copies of genes to affected cells in order to correct genetic defects. For example, targeting mutations associated with connective tissue disorders such as Marfan syndrome or Ehlers-Danlos syndrome may help to stabilize the scleral structure. Although still in the experimental stage, ongoing gene therapy research shows great promise for the future treatment of genetic causes of scleral ectasia.
Tissue Engineering and Regenerative Medicine
Advances in tissue engineering and regenerative medicine are providing new treatment options for scleral ectasia. Researchers are looking into the use of stem cells and bioengineered tissues to repair and regenerate damaged scleral tissue.
- Stem Cell Therapy: Mesenchymal stem cells (MSCs) have demonstrated potential for tissue repair and regeneration. MSCs can differentiate into different types of cells and secrete growth factors that promote healing. Preclinical studies show that MSCs can improve scleral integrity and reduce thinning. Clinical trials are required to confirm these findings and determine the safety and efficacy of stem cell therapy for scleral ectasia.
- Bioprinting: Bioprinting technology allows for the creation of customized, three-dimensional tissue constructs using bioinks made of cells and biomaterials. Researchers are looking into using bioprinting to create scleral grafts that are specific to the patient’s anatomy and needs. This method could provide a more precise and personalized treatment option for scleral ectasia, resulting in better graft integration and outcomes.
Advanced Imaging and Diagnostic Tools
Scleral ectasia management requires accurate diagnosis and monitoring. Imaging technology advancements improve the ability to see and assess scleral changes in detail.
- Optical Coherence Tomography (OCT): OCT can produce high-resolution cross-sectional images of the sclera and other ocular structures. Enhanced OCT technologies, such as swept-source OCT and OCT angiography, provide detailed images of scleral thinning and deformation. These tools are extremely useful for diagnosing and monitoring scleral ectasia, making treatment decisions, and detecting complications early on.
- Ultrasound Biomicroscopy (UBM): UBM is a high-frequency ultrasound technique that produces detailed images of the eye’s anterior segment, which includes the sclera. UBM is especially useful for determining the extent of scleral thinning and planning surgical procedures. Advances in UBM technology improve image resolution and diagnostic accuracy, allowing for more effective scleral ectasia management.
Pharmaceutical Innovations
The goal of pharmacological treatments for scleral ectasia is to develop drugs that can strengthen the sclera and prevent progression.
- Collagen Cross-linking Agents: In addition to corneal cross-linking, researchers are looking into pharmacological agents that can cause collagen cross-linking in the sclera. These agents aim to strengthen scleral collagen fibers, thereby increasing tissue rigidity and stability. Various compounds, including riboflavin and other photosensitizers, are being studied for their potential role in scleral cross-linking.
- Anti-Inflammatory and Anti-Fibrotic Agents: Inflammation and fibrosis can cause scleral thinning and weakening. Anti-inflammatory and anti-fibrotic medications are being tested for their ability to reduce these processes and maintain scleral integrity. Corticosteroids, nonsteroidal anti-inflammatory drugs (NSAIDs), and novel anti-fibrotic agents are being studied for their potential use in the treatment of scleral ectasia.
Surgical Innovations
Surgical techniques for scleral ectasia are constantly evolving, with new methods and technologies improving surgical precision and outcomes.
- Minimally Invasive Techniques: Advances in minimally invasive surgical techniques have increased the safety and efficacy of scleral reinforcement procedures. These techniques use smaller incisions and less trauma to the eye, which promotes faster recovery and lowers the risk of complications. Minimally invasive scleral patch grafting and reinforcement techniques are being developed and refined to improve patient outcomes.
- Robotic-Assisted Surgery: Researchers are looking into using robotic systems to help with delicate ocular surgeries such as scleral reinforcement and patch grafting. Robotic-assisted surgery improves precision and control, allowing surgeons to perform intricate maneuvers with high accuracy. This technology has the potential to increase the success rate of complex surgical procedures for scleral ectasia, lower the risk of complications, and improve visual outcomes.






