What is Noninfectious Endophthalmitis?
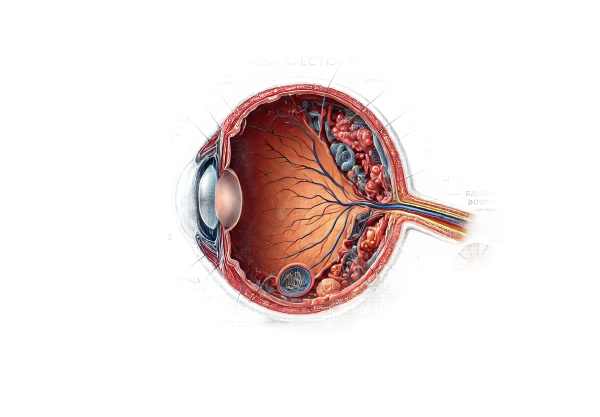
Non-infectious endophthalmitis is an inflammatory condition of the eye that affects intraocular tissues such as the vitreous and aqueous humors. In contrast to infectious endophthalmitis, which is caused by bacterial, fungal, or viral infections, non-infectious endophthalmitis is caused by non-infectious factors such as an allergic reaction, autoimmune response, or reaction to surgical procedures or medications. If not diagnosed and treated promptly, this condition can cause significant visual impairment.
Comprehensive Study of Non-Infectious Endophthalmitis
Non-infectious endophthalmitis is a complicated and multifaceted condition that can result from a variety of causes. Understanding the pathophysiology, clinical presentation, risk factors, and potential complications is critical for accurate diagnosis and treatment.
Pathophysiology
Non-infectious endophthalmitis causes inflammation of the intraocular structures in the absence of an infectious agent. Several mechanisms can cause this inflammation:
- Immune-Mediated Response: The body’s immune system may mistakenly attack intraocular tissues, causing inflammation. This can happen with autoimmune diseases like Behçet’s disease, sarcoidosis, and Vogt-Koyanagi-Harada (VKH) syndrome.
- Surgical Procedures: Inflammation can develop after ocular surgeries such as cataract extraction, vitrectomy, and intraocular lens implantation. This postoperative inflammation is commonly known as sterile endophthalmitis.
- Medications: Some medications, particularly intravitreal corticosteroids or anti-VEGF agents used to treat conditions such as macular degeneration, can cause a non-infectious inflammatory response.
- Trauma: Ocular trauma can cause an inflammatory response as the body tries to repair the damaged tissues.
Clinical Features
The clinical manifestation of non-infectious endophthalmitis varies greatly depending on the underlying cause and severity of the inflammation. Common symptoms include:
- Decreased Vision: Patients frequently experience a sudden decrease in vision, which can range from minor blurring to complete vision loss.
- Eye Pain: Pain in the affected eye is a common symptom, although the severity varies.
- Redness: Inflammation of the conjunctiva and episclera can cause the eye to appear red.
- Photophobia: Light sensitivity is common, making patients uncomfortable in brightly lit environments.
- Floaters: Inflammatory cells and debris in the vitreous can cause floaters or spots in patients’ vision.
Etiology
Non-infectious endophthalmitis can result from a variety of etiological factors, including
- Autoimmune Disorders: Behçet’s disease, sarcoidosis, and VKH syndrome can all result in intraocular inflammation.
- Post-Surgical Inflammation: Sterile endophthalmitis can develop after ocular surgeries, with inflammation typically appearing days to weeks later.
- Medications: Intravitreal injections with corticosteroids (e.g., triamcinolone acetonide) and anti-VEGF agents (e.g., bevacizumab) can cause non-infectious inflammation.
- Ocular Trauma: Injuries to the eye can cause an inflammatory response during the healing process.
Complications
Non-infectious endophthalmitis can cause a variety of complications if not treated promptly:
- Chronic Uveitis: Persistent inflammation can lead to chronic uveitis, which causes long-term damage to intraocular structures.
- Glaucoma: Inflammation can raise intraocular pressure, causing secondary glaucoma.
- Cataract Formation: Chronic inflammation can hasten cataract formation, resulting in additional vision impairment.
- Retinal Detachment: Severe inflammation can cause traction on the retina, possibly resulting in retinal detachment.
Differential Diagnosis
Accurate diagnosis of non-infectious endophthalmitis requires differentiation from other conditions that may present with similar symptoms, including:
- Infectious Endophthalmitis: Bacterial, fungal, or viral infections can cause intraocular inflammation, which is frequently associated with hypopyon (pus in the anterior chamber).
- Panophthalmitis: Severe, widespread inflammation of the entire eye, usually caused by an infection.
- Uveitis: Inflammation of the uvea (the middle layer of the eye) can cause similar symptoms but may not affect the vitreous and aqueous humors as much as endophthalmitis.
Prognosis
The prognosis for non-infectious endophthalmitis is dependent on the underlying cause and the timing of treatment. Early diagnosis and appropriate treatment are critical for preserving vision and avoiding complications. Most patients respond well to treatment, though some may have recurring episodes of inflammation that necessitate long-term management.
Assessing Non-Infectious Endophthalmitis
Non-infectious endophthalmitis is diagnosed using a combination of clinical, imaging, and laboratory tests. These diagnostic methods help to confirm the diagnosis, identify the underlying cause, and distinguish it from infectious endophthalmitis.
Clinical Evaluation
A thorough clinical examination is the first step in diagnosing non-infectious endophthalmitis. This includes:
- Patient History: Provide a detailed account of the patient’s symptoms, recent ocular procedures, medication use, and any underlying systemic diseases.
- Visual Acuity Test: Determines the degree of vision loss.
- Slit-Lamp Examination: Using a slit-lamp microscope, examine the anterior and posterior segments of the eye. This aids in detecting signs of inflammation, such as anterior chamber cells and flare, keratic precipitates, and vitreous haze.
- Fundoscopy: Examine the retina and optic nerve head for signs of inflammation, hemorrhages, or exudates.
Imaging Studies
Imaging studies provide detailed visualization of intraocular structures and can help assess the extent of inflammation:
- Optical Coherence Tomography (OCT): OCT produces high-resolution cross-sectional images of the retina and vitreous, allowing for precise measurements of retinal thickness, macular edema, and vitreous inflammation.
- Ultrasound B-Scan: B-scan ultrasonography is useful for evaluating the posterior segment, particularly when media opacities (e.g., vitreous hemorrhage) impair vision. It can detect vitreous debris, retinal detachment, and choroidal thickening.
Lab Tests
Laboratory tests can help identify underlying systemic conditions and differentiate between non-infectious and infectious causes.
- Blood Tests: Complete blood count (CBC), erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), and autoimmune disease-specific serologies (e.g., antinuclear antibodies, angiotensin-converting enzyme levels) can all provide useful information.
- Aqueous and Vitreous Sampling: In some cases, aqueous humor or vitreous samples may be obtained for cytological analysis in order to rule out infectious agents and confirm the condition’s inflammation.
Available Treatment Options for Noninfectious Endophthalmitis
The primary goal of non-infectious endophthalmitis treatment is to reduce inflammation, manage symptoms, and avoid complications. Treatment options vary according to the underlying cause and severity of the inflammation.
Corticosteroids
- Systemic Corticosteroids: Oral corticosteroids, such as prednisone, are frequently used to treat inflammation. The dosage and duration vary according to the severity of the condition and the patient’s response to treatment.
- Intravitreal Corticosteroids: For more localized and severe inflammation, intravitreal corticosteroids such as triamcinolone acetonide or dexamethasone implants can have a direct anti-inflammatory effect on the affected tissues.
- Topical Corticosteroids: When the inflammation is mild, topical corticosteroid eye drops can be used to treat anterior segment inflammation.
Immunosuppressive Agents
- Methotrexate: This immunosuppressive medication is frequently prescribed for the long-term treatment of autoimmune-related non-infectious endophthalmitis. It helps to lower immune system activity and prevent recurring inflammation.
- Azathioprine: Another immunosuppressive drug that can help control chronic inflammation and reduce the need for corticosteroids.
- Mycophenolate Mofetil: This medication is effective in treating severe or refractory cases by inhibiting the proliferation of immune cells involved in the inflammatory response.
Biological Agents
- Anti-TNF Agents: Infliximab and adalimumab are biologic therapies that target tumor necrosis factor (TNF), a major mediator of inflammation. These medications are especially effective in treating refractory non-infectious endophthalmitis associated with systemic autoimmune diseases.
- Interleukin Inhibitors: Tocilizumab, a medication that targets interleukins involved in the inflammatory process, provides an additional option for treating severe inflammation.
Adjunctive therapies
- Non-Steroidal Anti-Inflammatory Drugs (NSAIDs): Oral or topical NSAIDs can be combined with corticosteroids to control inflammation and pain.
- Cycloplegic Agents: Eye drops containing atropine or cyclopentolate, which dilate the pupil and paralyze the ciliary muscle, can help relieve pain and prevent the formation of synechiae (adhesions) in the anterior chamber.
Innovative and Emerging Therapies
- Gene Therapy: Researchers are working on gene therapy approaches that aim to modulate the immune response and reduce inflammation at the genetic level. This could provide long-term management of chronic inflammatory conditions.
- Stem Cell Therapy: Researchers are looking into the potential of stem cell therapy to repair and regenerate damaged ocular tissues, which could help restore vision in severe cases of non-infectious endophthalmitis.
- Nanotechnology-Based Drug Delivery: Nanotechnology advances are being investigated in order to create targeted drug delivery systems capable of delivering anti-inflammatory medications to intraocular tissues over time.
Non-infectious endophthalmitis requires a personalized approach that considers the underlying cause, severity of inflammation, and patient response to treatment. Regular follow-up and monitoring are critical for achieving successful outcomes and avoiding complications.
Effective Ways to Treat and Prevent Non-Infectious Endophthalmitis
Preventing and managing non-infectious endophthalmitis entails taking proactive measures to reduce inflammation and treat underlying conditions. Here are a few effective methods:
- Regular Eye Examinations: Schedule routine eye exams to monitor your ocular health, especially if you have underlying conditions that make you prone to inflammation.
- Manage Systemic Diseases: To reduce the risk of ocular inflammation, effectively manage autoimmune diseases and other systemic conditions with appropriate medical care.
- Post-Surgical Care: After ocular surgery, carefully follow the post-operative care instructions to reduce the risk of inflammation. This includes taking prescription medications and going to follow-up appointments.
- Medication Awareness: Be aware of the potential side effects of medications, particularly those given through intravitreal injections. If you notice any unusual symptoms, contact your doctor right away.
- Protect Your Eyes: Wear protective eyewear when engaging in activities that pose a risk of ocular trauma to avoid injury-related inflammation.
- Healthy Lifestyle: To support overall immune function and reduce inflammation risk, follow a healthy lifestyle that includes a balanced diet, regular exercise, and quitting smoking.
- Prompt Treatment: If you experience any symptoms of eye inflammation or vision changes, seek medical attention right away to ensure an early diagnosis and treatment.
- Avoid Self-Medication: Do not self-medicate with over-the-counter eye drops or other treatments without first consulting a medical professional, as this can exacerbate inflammation.
Trusted Resources
Books
- “Clinical Ophthalmology: A Systematic Approach” by Jack J. Kanski
- “Uveitis: Fundamentals and Clinical Practice” by Robert B. Nussenblatt and Scott M. Whitcup
- “Retinal Pharmacotherapy” by Quan Dong Nguyen and Jeffrey S. Heier






