What is Optic Nerve Head Avulsion?
Optic nerve head avulsion is a severe ocular condition characterized by the traumatic separation of the optic nerve fibers from the optic disc. Significant blunt trauma to the eye frequently causes this injury, which results in a complete or partial detachment of the optic nerve head. The condition is associated with profound vision loss and necessitates prompt diagnosis and treatment to address associated complications while preserving remaining vision.
Detailed Investigation of Optic Nerve Head Avulsion
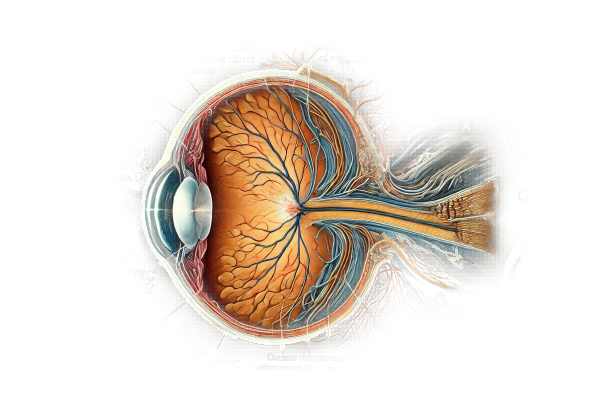
Anatomy and Function of the Optic Nerve
The optic nerve is an essential component of the visual system, transmitting visual information from the retina to the brain. Over a million nerve fibers converge at the optic disc, where they exit the eye to form the optic nerve. These fibers are most susceptible to traumatic injury at the optic nerve head, which is located on the optic disc.
Causes and Mechanisms of Injury
Optic nerve head avulsion is most commonly caused by severe blunt trauma to the eye or head. The mechanisms that contribute to this condition include:
- Blunt Trauma: A direct impact to the eye or head can cause a sudden and forceful movement of the globe, resulting in a shearing force on the optic nerve head. Common scenarios include car accidents, sports injuries, and physical assaults.
- Falls: Accidental falls, particularly those from great heights, can generate enough force to cause optic nerve head avulsion.
- Penetrating Trauma: Although less common, penetrating injuries can result in avulsion if the optic nerve head is directly struck.
- iatrogenic causes: In rare cases, surgical procedures involving the eye or orbit can result in optic nerve head avulsion, especially if there is excessive manipulation or force applied to the eye.
Clinical Presentation
Patients with optic nerve head avulsion usually present with sudden and severe vision loss in the affected eye. The clinical presentation may include:
- Profound vision loss: The most common and obvious symptom is a significant reduction in vision, which can range from severe visual impairment to complete blindness in the affected eye.
- Pain: Patients may experience ocular or periocular pain as a result of the trauma.
- Ocular Hemorrhage: The trauma may result in subconjunctival hemorrhage, hyphema (blood in the anterior chamber), or vitreous hemorrhage.
- Afferent Pupillary Defect: A relative afferent pupillary defect (RAPD) is a common finding, indicating severe optic nerve dysfunction.
- Retinal Findings: A fundoscopic examination can reveal retinal hemorrhages, macular edema, and other signs of retinal trauma.
Pathophysiology
The pathophysiology of optic nerve head avulsion involves the disruption of the delicate optic nerve fibers as they exit the eye. The shearing force of blunt trauma can cause these fibers to tear away from the optic disc, causing immediate and irreversible damage to the optic nerve. This separation disrupts the transmission of visual information from the retina to the brain, causing significant vision loss.
Secondary damage can occur due to:
- Ischemia: Trauma can disrupt the blood supply to the optic nerve head, resulting in ischemic damage and further loss of nerve function.
- Inflammation: The traumatic injury may cause an inflammatory response, which contributes to additional damage and edema in the affected area.
- Retinal Damage: Related retinal injuries, such as hemorrhages and edema, can worsen vision loss and complicate the clinical picture.
Complications
Avulsion of the optic nerve head can cause a number of immediate and long-term complications.
- Permanent vision loss: The most serious complication is permanent vision loss in the affected eye, which can have a significant impact on the patient’s quality of life.
- Retinal Detachment: Trauma severe enough to cause optic nerve head avulsion can also result in retinal detachment, which is a serious condition requiring immediate surgical intervention.
- Vitreous hemorrhage: Bleeding into the vitreous cavity can obscure the fundus view, complicating the injury’s assessment and management.
- Secondary Glaucoma: Trauma and inflammation can cause increased intraocular pressure, which can further impair vision.
Prognosis
The prognosis for optic nerve head avulsion is generally poor due to the severity of the injury. Vision loss is usually permanent, with little or no recovery. The severity of the initial trauma, the presence of associated injuries, and the promptness of diagnosis and management all influence the overall outcome.
Diagnostic methods
To confirm the diagnosis and assess the extent of the injury, an extensive clinical evaluation is required, as well as the use of advanced imaging techniques.
Clinical Evaluation
- Patient History: – Provide a detailed history of the trauma, including injury mechanism, symptom onset, and any visual or neurological changes. Information about the force and direction of the impact can help predict the likelihood of optic nerve head avulsion.
- Ophthalmic Examination: – Visual Acuity Test: Assessing visual acuity can determine the extent of vision loss in the affected eye.
- Pupil Examination: Looking for a relative afferent pupillary defect (RAPD) can indicate severe optic nerve damage.
- **Fundoscopy: A direct examination of the optic disc and retina can reveal signs of avulsion, such as hemorrhages, retinal tears, and pallor.
Imaging Studies
- Optical Coherence Tomography (OCT):
- OCT produces high-resolution cross-sectional images of the optic nerve head and retina, allowing for a thorough evaluation of the structural integrity of the optic nerve fibers. It can help detect disruptions and other signs of trauma to the optic disc.
- Magnetic Resonance Imaging (MRI): – MRI of the brain and orbits helps visualize the optic nerve and surrounding structures. It can assist in determining the extent of the injury, associated hemorrhages, and any other intracranial or orbital abnormalities. Gadolinium-enhanced MRI can reveal additional information about blood flow and tissue integrity.
- Computerized Tomography (CT) Scan: CT scans are particularly effective at detecting fractures and bony injuries in the orbit and skull. They can also aid in the detection of any foreign bodies or other structural damage associated with the trauma.
Additional Tests
- Visual Field Testing: Automated perimetry can assess visual field loss and identify areas with preserved vision.
- Fluorescein Angiography: – This imaging technique involves injecting a fluorescent dye into the bloodstream to see the retinal and choroidal circulation. It can aid in detecting any vascular abnormalities or areas of ischemia associated with the trauma.
Differential Diagnosis
Several other conditions can present with symptoms similar to optic nerve head avulsion, necessitating a careful differential diagnosis:
- Optic Neuritis: Inflammation of the optic nerve can cause sudden vision loss and pain with eye movement. Clinical history and imaging findings are used to differentiate patients.
- Retinal Detachment: Retinal detachment is frequently a complication of optic nerve head avulsion, but it can also occur independently. Prompt imaging and clinical evaluation can help distinguish between the two conditions.
- Orbital Fractures: Fractures of the orbit can cause similar symptoms, so imaging studies are essential for accurate diagnosis and treatment.
Optic Nerve Head Avulsion Treatment
Standard Treatment Options
The treatment of optic nerve head avulsion is primarily concerned with addressing associated complications, alleviating symptoms, and preserving any remaining vision. Given the severity of the condition, treatment frequently necessitates a collaborative effort involving ophthalmologists, neurologists, and other specialists.
- Immediate Management: – Stabilization: Immediate attention is necessary to stabilize the patient, especially in severe trauma cases. This may include addressing any life-threatening injuries and ensuring the patient is stable enough for further ophthalmic evaluation.
- Pain management: Analgesics and anti-inflammatory medications may be used to alleviate pain and inflammation.
- Surgical Intervention: • Retinal Detachment Repair: If a retinal detachment occurs, immediate surgical intervention, such as scleral buckle surgery or vitrectomy, is required to reattach the retina and prevent further vision loss.
- Management of Vitreous Hemorrhage Vitrectomy may also be required to remove vitreous hemorrhage that obstructs the fundus view and complicates injury assessment and management.
- Management of Secondary Glaucoma: – Medications: Beta-blockers, alpha agonists, or prostaglandin analogs can manage intraocular pressure and prevent secondary glaucoma.
- Surgical Procedures: If medical treatment is insufficient, surgical procedures such as trabeculectomy or glaucoma drainage implants may be required.
Innovative and Emerging Therapies
- Neuroprotective Agents: – Research into neuroprotective drugs aims to protect remaining optic nerve fibers from damage. These agents, which include brimonidine and citicoline, are being investigated for their ability to slow the progression of optic nerve damage and preserve vision.
- Stem Cell Therapy: – This emerging field has the potential to regenerate damaged optic nerve cells. Although still experimental, early research suggests that stem cell transplantation could help restore some vision by replacing lost or damaged neurons.
- Advances in gene therapy provide hope for treating genetic conditions that lead to optic nerve injuries. Gene therapy, which corrects genetic defects at the molecular level, has the potential to prevent or reduce the effects of optic nerve head avulsion in susceptible individuals.
- Electrical Stimulation: – Transorbital alternating current stimulation (tACS) is being studied for its potential to stimulate optic nerve cells and improve visual function. This non-invasive approach aims to increase neural activity and potentially improve vision outcomes.
Supportive Care and Rehabilitation
- Vision Rehabilitation: – Patients with significant vision loss can benefit from vision rehabilitation services such as low vision aids, orientation and mobility training, and adaptive techniques to improve their quality of life.
- Psychological Support: – Coping with sudden and profound vision loss due to optic nerve head avulsion can be challenging. Psychological support and counseling can help patients and their families address emotional and mental health concerns, as well as provide strategies for managing the condition’s impact.
Long-Term Monitoring
Regular visits to an ophthalmologist are required to monitor the patient’s condition, evaluate the efficacy of treatments, and manage any emerging complications. Periodic visual acuity tests, intraocular pressure measurements, and imaging studies are essential for monitoring changes and adjusting treatment plans as necessary.
Effective Ways to Improve and Prevent Optic Nerve Head Avulsion
- Wear Protective Eyewear: – Wear protective eyewear when participating in activities that may cause eye injury, such as sports, construction, or using power tools.
- Follow safety protocols in high-risk environments to prevent eye and head trauma.
- Use Seatbelts and Helmets: – Wear seatbelts in vehicles and helmets when riding motorcycles, bicycles, or participating in contact sports to prevent head and eye injuries.
- Educate on Risk Factors: – Raising awareness of the risk factors and potential causes of optic nerve head avulsion, particularly among children and athletes.
- Seek immediate medical attention for eye trauma, even if symptoms appear mild. Early intervention can help prevent complications and improve outcomes.
- Regular eye exams can detect underlying conditions that increase the risk of optic nerve injuries and provide timely management.
- Maintaining a healthy lifestyle, such as a balanced diet, regular exercise, and avoiding smoking, can improve overall eye health and reduce the risk of systemic conditions that can worsen ocular injuries.
- Emergency Preparedness: – Know basic first aid and have access to emergency medical services to respond quickly to eye injuries.
- Support Networks: – Connect with support networks and resources for individuals at risk of eye injuries to learn about preventive measures and manage risk factors.
Trusted Resources
Books
- “Clinical Neuro-Ophthalmology: A Practical Guide” by Ambar Chakravarty
- “Trauma and Emergency Care for the Eye” by Robert P. Olympia and Brian K. Reilly
- “Ocular Trauma: Principles and Practice” by Ferenc Kuhn






