What is Optic Nerve Meningioma?
Optic nerve meningioma is a rare, usually benign tumor that develops from the meninges, the protective layers that surround the optic nerve. The location and growth patterns of these tumors can cause progressive vision loss and other ocular symptoms. Despite their slow growth rate, optic nerve meningiomas can have a significant impact on visual function and quality of life, necessitating careful diagnosis and management.
Detailed Examination of Optic Nerve Meningioma
Anatomy and Pathophysiology
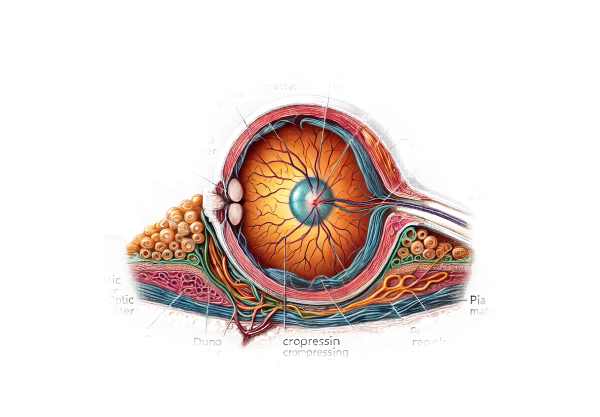
The optic nerve transports visual information from the retina to the brain. The dura mater, arachnoid mater, and pia mater are the three layers that surround it. Meningiomas develop from arachnoid cap cells found in these layers. When these tumors grow around the optic nerve, they can put pressure on the nerve fibers, resulting in progressive vision loss.
The most common age group for optic nerve meningiomas is middle-aged adults, with women having a higher prevalence. These tumors make up about 2% of all orbital tumors and roughly 4% of intracranial meningiomas.
Causes and Risk Factors
The exact cause of optic nerve meningiomas is unknown, but several risk factors and genetic conditions are associated with their development:
- Genetic Mutations: – NF2 gene mutations linked to neurofibromatosis type 2 increase the risk of developing meningiomas, including those near the optic nerve.
- Radiation Exposure: Previous exposure to radiation, especially in the head and neck region, is a known risk factor for meningiomas.
- Gender: – Women are more likely than men to develop meningiomas, potentially due to hormonal influences.
Clinical Presentation
The symptoms of optic nerve meningioma vary according to the tumor’s size and location. Common clinical characteristics include:
- Progressive vision loss: The most common symptom is a slow loss of vision in one eye. This can begin as a slight decrease in visual acuity and progress to severe vision impairment.
- Optic Atrophy: – Chronic pressure on optic nerve fibers can cause a pale optic disc, indicating optic atrophy.
- Proptosis: – Tumor growth within the orbit can cause forward displacement of the eye (proptosis).
- Optic Disc Swelling: – Optic disc swelling (papilledema) may indicate increased intracranial pressure or direct tumor compression.
- Visual Field Defects: – Patients may experience visual field defects, including loss of peripheral vision or blind spots (scotomas).
- Pain: – Although uncommon, some patients may experience pain or discomfort around the affected eye.
Pathophysiology
Optic nerve meningiomas primarily cause mechanical compression of the optic nerve fibers and surrounding structures. The tumor’s growth within the confined space of the optic canal or the orbit can result in
- Compression of the optic nerve can cause ischemia, resulting in nerve damage.
- Inflammation: – Chronic compression can cause an inflammatory response, worsening nerve damage.
- Axonal Degeneration: Prolonged pressure on optic nerve fibers can cause axonal degeneration and loss of neural function, leading to progressive vision loss.
Complications
If left untreated, optic nerve meningiomas can cause a number of complications:
- Permanent Vision Loss: – Damage to the optic nerve can lead to irreversible vision loss.
- Intracranial Extension: – Tumors may spread intracranially, affecting other nerves and brain structures.
- Secondary Glaucoma: Tumor growth can cause increased intraocular pressure, compromising vision.
- Cosmetic Concerns: Significant proptosis can cause cosmetic deformities, affecting patients’ self-esteem and quality of life.
Prognosis
Individuals with optic nerve meningioma have a poor prognosis due to a number of factors, including the size and location of the tumor, the rate of growth, and the effectiveness of treatment. Early diagnosis and treatment are critical for maintaining vision and improving outcomes. While optic nerve meningiomas are usually benign and slow-growing, they can have a significant impact on visual function if not treated properly.
Diagnostic methods
Accurate diagnosis of optic nerve meningioma necessitates a multidisciplinary approach that includes clinical evaluation, imaging studies, and, in some cases, histopathology.
Clinical Evaluation
- Patient History: – Detailed patient history is crucial for determining the onset and progression of symptoms. Important considerations include the duration of vision loss, any associated pain or discomfort, and the presence of systemic symptoms that could indicate a more widespread condition.
- Ophthalmic Examination: – Visual Acuity Testing: Evaluates vision clarity to identify visual impairments.
- Fundoscopy: A direct examination of the optic disc to detect signs of atrophy or swelling. A pale optic disc or papilledema can indicate underlying pathology.
- Pupil reactions: An examination of the pupil’s response to light can reveal an afferent pupillary defect, indicating severe optic nerve dysfunction.
Imaging Studies
- The preferred imaging method for diagnosing optic nerve meningioma is magnetic resonance imaging (MRI). It generates high-resolution images of the optic nerve and surrounding structures, allowing for a thorough evaluation of the tumor’s size, location, and extent. Gadolinium-enhanced MRI can help with tumor delineation and vascularity assessment.
- Computerized Tomography (CT) Scan: CT scans are useful in assessing bony changes in the orbit and optic canal. They can also detect calcifications within the tumor that are typical of meningiomas. CT imaging is especially useful when an MRI is either contraindicated or unavailable.
- Orbital Ultrasound: – Ultrasound imaging can reveal more about the tumor’s characteristics and its relationship with surrounding structures. It is an effective adjunctive tool, especially for determining orbital involvement.
Additional Diagnostic Tests
- Automated perimetry can detect and quantify visual field defects, offering objective evidence of optic nerve dysfunction.
- Fluorescein Angiography: – This imaging technique involves injecting a fluorescent dye into the bloodstream to see the retinal and choroidal circulation. It can assist in detecting any vascular abnormalities or areas of ischemia associated with the tumor.
Differential Diagnosis
Several other conditions can cause symptoms similar to optic nerve meningioma, necessitating a careful differential diagnosis:
- Optic Neuritis: – Optic nerve inflammation, often linked to multiple sclerosis, can result in acute vision loss and swelling of the optic disc. Differentiation is based on clinical history, MRI findings, and corticosteroid response.
- Optic Glioma: – Optic gliomas are a type of optic nerve tumor more commonly found in children. MRI results and histopathological examinations can help distinguish between gliomas and meningiomas.
- Orbital Tumors: – Other orbital tumors, like lymphomas or metastatic lesions, may cause similar symptoms. Comprehensive imaging and, if necessary, biopsy contribute to an accurate diagnosis.
- Intracranial Tumors: – Brain or cranial nerve tumors can impair vision. Detailed neuroimaging is required to determine the primary location and extent of the tumor.
Optic Nerve Meningioma Treatment
Standard Treatment Options
The treatment of optic nerve meningioma aims to preserve vision, alleviate symptoms, and control tumor growth. The size and location of the tumor, the patient’s age and overall health, and the degree of visual impairment all influence treatment decisions.
- Observation: – For small, asymptomatic tumors or those with slow growth, a watch-and-wait approach with regular monitoring may be sufficient. This includes regular MRI scans and ophthalmic evaluations to monitor the tumor’s progression and visual function.
- Surgery: – Resection: Larger tumors that cause significant visual impairment or those that grow quickly may be candidates for surgical removal. The goal is to remove as much of the tumor as possible while keeping the optic nerve functional. However, because the tumor is so close to the optic nerve and other vital structures, complete resection can be difficult.
- Debulking: In some cases, the tumor is partially removed (debulked) to reduce its size and alleviate pressure on the optic nerve.
- Radiation Therapy: – Fractionated Radiotherapy: This entails administering small doses of radiation over multiple sessions in order to minimize damage to surrounding tissues while targeting the tumor. It is frequently used for tumors that are not amenable to surgery or as a supplement to surgery.
- Stereotactic Radiosurgery: Techniques like Gamma Knife and CyberKnife deliver highly focused radiation to the tumor while minimizing exposure to surrounding structures. This method is especially effective for small to medium-sized tumors.
Innovative and Emerging Therapies
- Targeted Molecular Therapies: Research into the molecular pathways involved in meningioma growth has resulted in the development of targeted treatments. These drugs seek to inhibit specific proteins or receptors that promote tumor growth. Inhibitors of the platelet-derived growth factor (PDGF) and vascular endothelial growth factor (VEGF) pathways, for example, are under investigation.
- Immunotherapy: – Immunotherapy uses the body’s immune system to target and eliminate tumor cells. Checkpoint inhibitors, which block proteins that prevent the immune system from attacking cancer cells, are being investigated for their potential use in meningiomas.
- Gene Therapy: – Gene therapy alters tumor cells’ genetic material to inhibit growth or increase susceptibility to other treatments. This approach is still in the experimental stages, but it shows promise for the future.
- Neuroprotective Agents: – These drugs aim to preserve optic nerve function and prevent additional damage. Citicoline and brimonidine are being investigated for their ability to improve neural survival and function.
Supportive Care
- Visual Rehabilitation: Patients with significant vision loss can benefit from visual rehabilitation services, such as low vision aids, orientation and mobility training, and adaptive techniques, to improve their quality of life.
- Psychological Support: Managing a chronic condition, such as optic nerve meningioma, can be challenging. Psychological support and counseling can help with emotional and mental health issues, including stress management strategies and overall well-being.
Monitoring and Follow-up
Regular follow-up with a multidisciplinary team, including ophthalmologists, neurologists, and oncologists, is required to monitor the patient’s condition, assess treatment efficacy, and manage any new complications. Periodic visual acuity tests, visual field assessments, and imaging studies are essential for monitoring changes and adjusting treatment plans as necessary.
Effective Ways to Improve and Prevent Optic Nerve Meningioma
- Schedule regular eye exams to detect vision changes and check for signs of optic nerve meningioma. Early detection can result in timely intervention and better outcomes.
- Awareness of Symptoms: Be aware of the symptoms of optic nerve meningioma, which include progressive vision loss, proptosis, and visual field abnormalities. If you experience any of these symptoms, seek medical attention right away.
- Manage Risk Factors: – Minimize exposure to radiation, especially in the head and neck region, which can increase the risk of meningiomas.
- Genetic Counseling: – Genetic counseling can help individuals with a family history of neurofibromatosis type 2 or other genetic predispositions understand their risk of developing optic nerve meningiomas and make informed family planning decisions.
- Maintaining a healthy lifestyle, such as a balanced diet, regular exercise, and avoiding smoking, can improve overall health and reduce the risk of developing tumors.
- Protective Measures: – Reduce exposure to environmental hazards that may cause meningiomas.
- Stay Informed: – Stay up-to-date on the latest research and advances in treating and managing optic nerve meningiomas. Understanding emerging therapies and clinical trials can open up new opportunities for effective management.
- Support Networks: – Connect with support groups and resources for people with optic nerve meningomas. These networks can offer emotional support, practical advice, and information on the most recent treatment options.
Trusted Resources
Books
- “Clinical Neuro-Ophthalmology: A Practical Guide” by Ambar Chakravarty
- “Meningiomas: Diagnosis, Treatment, and Outcome” by Joung H. Lee and Dharampaul S. Masson
- “Neuro-Ophthalmology Illustrated” by Valérie Biousse and Nancy J. Newman






