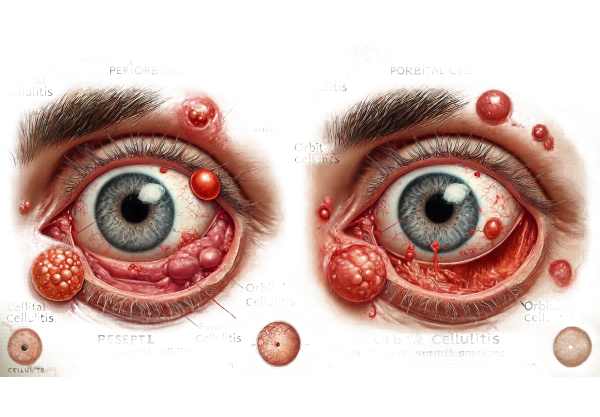
What is Orbital Cellulitis?
Orbital cellulitis is a severe infection that affects the tissues around the eye, such as the eyelids, brows, and cheek. Bacterial infections spread from the sinuses, teeth, or bloodstream are common causes of this condition. If not treated promptly, orbital cellulitis can cause serious complications such as vision loss, meningitis, and a brain abscess. It primarily affects children but can also occur in adults. The condition necessitates immediate medical attention to avoid serious health consequences and maintain ocular function.
Detailed Insights into Orbital Cellulitis
Orbital cellulitis is an infection of the orbit, the bony cavity that houses the eye. It is a potentially fatal condition that requires immediate diagnosis and treatment. There are two types of orbital cellulitis: preseptal (periorbital) and orbital cellulitis. Preseptal cellulitis affects the tissues in front of the orbital septum, whereas orbital cellulitis affects the tissues behind the septum.
Causes and Risk Factors
Bacterial infections are a common cause of orbital cellulitis. The three most common pathogens are Streptococcus pneumoniae, Staphylococcus aureus (including MRSA), and Haemophilus influenzae. These bacteria can enter the orbit via a variety of pathways, including:
- Sinusitis is the most common cause of orbital cellulitis. The infection spreads from the ethmoid or maxillary sinuses into the orbit.
- Trauma: Direct trauma to the eye or surrounding structures can bring bacteria into the orbit.
- Dental Infections: Infections of the teeth or gums may spread to the orbit.
- Skin Infections: Impetigo and erysipelas, both of which affect the eyelids and face, can spread to the orbit.
- Hemogenous Spread: Bacteria can travel to the orbit via the bloodstream from distant sites of infection.
Symptoms
The symptoms of orbital cellulitis vary, but typically include:
- Eye Pain: Typically severe and worsens with eye movement.
- Swelling and redness: in the eyelids and surrounding tissues.
- Proptosis: Bulging of the eyeball.
- Ophthalmoplegia: Muscle involvement results in restricted eye movements.
- Decreased Vision: Caused by pressure on the optic nerve or other ocular structures.
- Fever indicates a systemic response to infection.
- Headache and malaise are common systemic symptoms.
Pathophysiology
Orbital cellulitis occurs when an infection spreads to the orbit, causing inflammation and swelling of the tissues. This inflammation can cause an increase in intraorbital pressure, compressing the optic nerve and other ocular structures. If not treated right away, the infection can spread to intracranial structures, resulting in serious complications like meningitis, brain abscess, and cavernous sinus thrombosis.
Complications
Orbital cellulitis can cause several serious complications, including:
- Vision Loss: Caused by optic nerve damage from increased intraorbital pressure or direct bacterial invasion.
- Meningitis: Infection can spread to the meninges, the protective membranes that surround the brain and spinal cord.
- Brain Abscess: A localized collection of pus within brain tissue.
- Cavernous Sinus Thrombosis is the formation of a blood clot in the cavernous sinus, a large vein at the base of the brain.
- Septicemia: Bacteria enter the bloodstream, causing systemic infection and potentially septic shock.
Differential Diagnosis
It is critical to distinguish orbital cellulitis from other conditions that can cause similar symptoms, such as:
- Preseptal Cellulitis: Infection of tissues anterior to the orbital septum. It does not result in proptosis or ophthalmoplegia.
- Allergic Reactions: Can cause eyelid swelling and redness, but usually without the severe pain and systemic symptoms of orbital cellulitis.
- Thyroid Eye Disease: Can cause proptosis and ophthalmoplegia, but is typically associated with thyroid dysfunction and shows no signs of infection.
- Orbital Tumors: Can cause proptosis and vision changes, but usually develop gradually and without systemic symptoms.
Epidemiology
Orbital cellulitis affects more children than adults, with males having a higher incidence. The condition is more common in the winter, which corresponds to an increase in the incidence of sinus infections. While the introduction of the Haemophilus influenzae type b (Hib) vaccine has significantly reduced the incidence of this pathogen-caused orbital cellulitis, Streptococcus pneumoniae and Staphylococcus aureus continue to be common causes.
Diagnostic Procedures for Orbital Cellulitis
Orbital cellulitis is diagnosed using a combination of clinical, imaging, and laboratory tests. Early and accurate diagnosis is critical for initiating appropriate treatment and avoiding complications.
Clinical Evaluation
The initial assessment consists of a thorough clinical evaluation, including:
- Medical History: Obtaining a thorough history of recent infections, trauma, dental problems, or systemic symptoms.
- Physical Exam: Look for signs of orbital cellulitis, such as eyelid swelling, redness, proptosis, restricted eye movements, and blurred vision.
- Systemic Examination: Looking for symptoms of a systemic infection, such as fever, headache, or malaise.
Imaging Studies
Imaging studies are necessary for confirming the diagnosis and determining the extent of the infection.
- Computed Tomography (CT): A CT scan of the orbits and sinuses is the preferred imaging method. It can detect abscesses, sinusitis, orbital inflammation, and any infection that has spread intracranially. CT scans produce detailed images of bony structures and can help distinguish between preseptal and orbital cellulitis.
- MRI (Magnetic Resonance Imaging): In some cases, MRI can provide more detailed images of soft tissues and assess the involvement of the optic nerve, brain, and cavernous sinus. An MRI is especially useful when complications like cavernous sinus thrombosis or a brain abscess are suspected.
Lab Tests
Laboratory tests help identify the causative organism and guide antibiotic therapy.
- Blood Culture: Blood samples are collected to identify any bacteria in the bloodstream. Positive blood cultures can detect bacteremia and help determine the best antibiotic treatment.
- The Complete Blood Count (CBC): A CBC may show elevated white blood cell counts, indicating an active infection.
- Cultures and sensitivities: If there is a draining abscess or conjunctival discharge, samples can be taken and cultured to identify the bacteria and their antibiotic sensitivity.
If meningitis is suspected, a lumbar puncture can be used to analyze cerebrospinal fluid for bacteria or inflammatory cells.
- Ophthalmic Ultrasound: In some cases, ultrasound can be used to determine the extent of orbital involvement and to guide abscess aspiration.
Orbital Cellulitis Treatment
Orbital cellulitis is treated with a combination of medications and, in some cases, surgery. Prompt initiation of appropriate therapy is critical for avoiding complications and maintaining vision.
Medical Treatment
- Antibiotics: Intravenous (IV) antibiotics are the primary treatment for orbital cellulitis. Broad-spectrum antibiotics are usually started empirically and then adjusted according to culture and sensitivity results. Common antibiotics include:
- Ceftriaxone or Cefotaxime: These third-generation cephalosporins work against common pathogens such as Streptococcus pneumoniae and Haemophilus influenzae.
- Vancomycin: Added to protect against methicillin-resistant Staphylococcus aureus (MRSA), if suspected or confirmed.
- Metronidazole: It may be included to cover anaerobic bacteria, particularly if a dental infection is suspected.
- Oral Antibiotics: Once the patient has shown significant clinical improvement and is stable, a switch to oral antibiotics can be considered. Antibiotic therapy typically lasts two to three weeks, depending on the severity of the infection and the patient’s response to treatment.
- Supportive Care: Analgesics for pain relief, antipyretics for fever control, and hydration to maintain proper fluid balance are all examples of supportive measures.
Surgical Treatment
Surgical intervention may be required in certain cases of orbital cellulitis, particularly when there are complications or a failure to respond to medical therapy:
- Abscess Drainage: Orbital or subperiosteal abscesses may necessitate drainage. This can be done either externally or endoscopically through the nasal passages, depending on the location of the abscess and the surgeon’s expertise.
- Sinus Surgery: If sinusitis is the root cause, functional endoscopic sinus surgery (FESS) may be required to drain the infected sinuses and improve sinus drainage.
Innovative and Emerging Therapies
- Adjunctive Corticosteroids: Some research suggests that combining corticosteroids with antibiotic therapy can reduce inflammation and improve outcomes. However, their use remains contentious and is usually considered on an individual basis.
- Advanced Imaging Techniques: New imaging technologies, such as diffusion-weighted MRI, can provide more detailed information about the scope of infection and help guide treatment decisions.
- Antibiotic Stewardship Programs: These programs use evidence-based protocols and monitoring to optimize antibiotic use, reduce resistance, and improve patient outcomes.
Effective Ways to Improve and Avoid Orbital Cellulitis
- Maintain good sinus health by regularly managing and treating sinus infections with appropriate medications.
- Use saline nasal spray to keep your nasal passages moist and clear.
- Maintain good dental hygiene by brushing at least twice daily and flossing regularly.
- Schedule regular dental examinations and cleanings.
- Provide immediate wound care by cleaning and protecting any facial or ocular injuries to prevent infection.
- Seek medical attention if you have significant injuries or signs of infection.
- Vaccination: – Update vaccinations for Hib and Streptococcus pneumoniae.
- Avoid contact with infected individuals to prevent sinusitis and orbital cellulitis.
- Monitor and Manage Allergies: – Use prescribed allergy medications to control symptoms and prevent sinus infections.
- Stay Hydrated: – Drink plenty of fluids to keep mucous membranes moist and prevent sinus infections.
- Avoid smoking and secondhand smoke, as it can irritate nasal passages and increase the risk of sinus infections.
Trusted Resources
Books
- “Ocular and Orbital Infections” by Peter J. Kertes and Tien Y. Wong
- “Clinical Ophthalmology: A Systematic Approach” by Jack J. Kanski and Brad Bowling
- “The Wills Eye Manual: Office and Emergency Room Diagnosis and Treatment of Eye Disease” by Adam T. Gerstenblith and Peter D. Pavan-Langston
Online Resources
- American Academy of Ophthalmology (AAO): aao.org
- Centers for Disease Control and Prevention (CDC): cdc.gov
- MedlinePlus: medlineplus.gov