What is Orbital Pseudotumor?
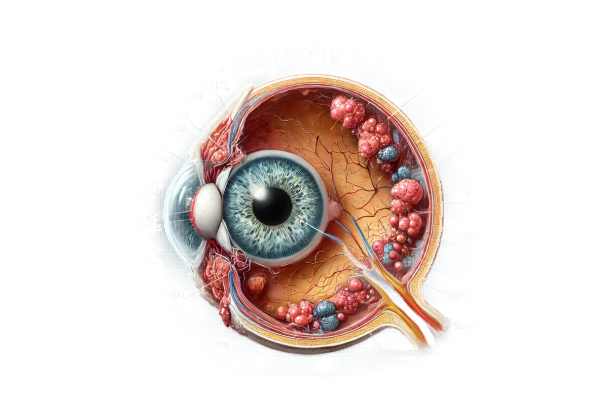
Orbital pseudotumor, also known as idiopathic orbital inflammation, is a non-specific inflammatory condition of the orbit, the bony cavity that houses the eye. Unlike true tumors, orbital pseudotumors are not cancerous, but they can produce symptoms similar to orbital tumors, such as pain, swelling, proptosis (eye bulging), and vision changes. The cause of this inflammation is unknown, which is why it is known as “idiopathic.” Prompt diagnosis and treatment are critical for preventing permanent damage to ocular structures and preserving vision.
Detailed Exploration of Orbital Pseudotumor Orbital pseudotumor
is a condition that causes inflammation in the orbit, affecting tissues such as extraocular muscles, lacrimal gland, orbital fat, and optic nerve. The exact cause is unknown, and it is considered an exclusionary diagnosis, which means that other possible causes of orbital inflammation must be eliminated first.
Epidemiology
Orbital pseudotumors can affect people of all ages, but they are most common in adults aged 30 to 50. There is no significant gender bias, though some studies indicate a slight female advantage. The condition is fairly uncommon, accounting for only 5-10% of all orbital disorders.
Pathophysiology
The pathophysiology of orbital pseudotumors includes an inflammatory process that can be localized or diffuse within the orbit. This inflammation causes immune cell infiltration, edema, and fibrosis, which lead to the disease’s clinical manifestations. The inflammation may be granulomatous or non-granulomatous, with the latter being more common. The cause of the inflammation is unknown, but it is thought to be associated with an abnormal immune response.
Clinical Presentation
The symptoms of orbital pseudotumor vary greatly depending on the tissues involved and the level of inflammation. Common clinical characteristics include:
- Pain: Severe, often sudden onset orbital pain exacerbated by eye movement.
- Proptosis: Forward displacement of the eye, either unilaterally or bilaterally.
- Diplopia: Double vision caused by the involvement of extraocular muscles, resulting in dysfunction.
- Eyelid Swelling: Eyelid edema that can be severe and cause ptosis (upper eyelid drooping).
- Redness and warmth: Indications of inflammation in the skin and conjunctiva.
- Decreased Vision: This occurs when the optic nerve is involved or when there is a lot of pressure on the ocular structures.
- Lacrimal Gland Enlargement: Swelling of the lacrimal gland can result in discomfort and tearing.
Types of Orbital Pseudotumor
Orbital pseudotumor can appear in several forms, depending on the primary site of inflammation:
- Diffuse Orbital Inflammation: Causes widespread inflammation throughout the orbit, affecting a variety of structures.
- Myositis: Inflammation of one or more extraocular muscles, causing painful eye movements and diplopia.
- Dacryoadenitis is an inflammation of the lacrimal gland that causes swelling in the upper outer quadrant of the orbit.
- Perineuritis: Involvement of the optic nerve sheath, which can cause vision problems and optic neuropathy.
- Sclerosing Pseudotumor: Characterised by dense fibrosis, which leads to a more chronic and progressive course.
Differential Diagnosis
Orbital pseudotumor must be distinguished from other conditions that can cause similar symptoms, including:
- Thyroid Eye Disease: Typically characterized by bilateral proptosis and thyroid dysfunction.
- Orbital Cellulitis: An infection that causes pain, redness, and swelling, along with systemic symptoms such as fever.
- Orbital Tumors: Both benign and malignant tumors can reproduce the mass effect and proptosis seen in pseudotumors.
- Sarcoidosis: A systemic granulomatous disease that can affect the orbit and cause pseudotumors.
- Wegener’s Granulomatosis: A vasculitic condition associated with orbital inflammation.
Complications
If not treated promptly, orbital pseudotumor can cause several complications, including:
- Vision Loss caused by optic nerve compression or ischemia.
- Chronic Pain: Persistent inflammation can cause long-term pain and discomfort.
- Fibrosis: Chronic inflammation can lead to fibrosis and scarring, resulting in permanent structural changes in the orbit.
- Strabismus: Eye misalignment caused by extraocular muscle involvement, resulting in persistent double vision.
Prognosis
The prognosis for patients with orbital pseudotumors varies according to their severity and response to treatment. Many patients respond positively to corticosteroids and other immunosuppressive therapies, resulting in symptom resolution. However, some cases may become chronic or recurring, necessitating ongoing treatment.
Understanding the specifics of orbital pseudotumor, such as its epidemiology, pathophysiology, clinical presentation, differential diagnosis, and potential complications, is critical for healthcare providers to accurately diagnose and manage this condition.
Diagnostic Techniques for Orbital Pseudotumor
Clinical evaluation, imaging studies, and, in some cases, biopsy are all required to accurately diagnose orbital pseudotumor. To confirm the diagnosis, it is critical to rule out any other potential causes of orbital inflammation.
Clinical Evaluation
The first step in diagnosing orbital pseudotumor is a thorough clinical evaluation.
- Patient History: A thorough account of the onset, duration, and progression of symptoms. It is critical to note any associated systemic symptoms or previous cases of orbital inflammation.
- Physical exam: A thorough examination of the eyes and orbit, including visual acuity testing, ocular motility evaluation, and screening for proptosis, eyelid swelling, and conjunctival injection.
Imaging Studies
Imaging is critical for determining the extent of inflammation and ruling out other conditions.
- Computed Tomography (CT): CT scans produce detailed cross-sectional images of the orbit, allowing for the detection of mass effects, bone involvement, and the severity of inflammation. CT is especially useful for detecting calcifications and determining the relationship between the inflammation and surrounding structures.
- MRI (Magnetic Resonance Imaging): MRI provides superior soft tissue contrast and is critical for determining the size, shape, and extent of the inflammation, particularly its involvement with the optic nerve, extraocular muscles, and other intracranial structures. MRI can distinguish between various tissue types and produce detailed images of the inflammatory process.
- Ultrasound: Orbital ultrasound can be used to help determine the size, shape, and vascularity of an inflammatory mass. It is a non-invasive, quick imaging technique that can help guide future diagnostic procedures.
Biopsy
In some cases, a biopsy may be required to confirm the diagnosis and rule out other possible causes of orbital inflammation.
- Incisional biopsy: A small incision is used to obtain a sample of affected tissue. The biopsy is then histologically examined to detect inflammatory cells, fibrosis, and other hallmarks of orbital pseudotumor.
- Fine-Needle Aspiration: A less invasive technique that uses a fine needle to extract a sample of the inflammatory mass for cytological analysis.
Additional Tests: – Blood Tests: Routine blood tests, such as complete blood count (CBC) and inflammatory markers (e.g., ESR, CRP), can assess a patient’s overall health and detect systemic inflammation or infection.
- Autoimmune Panel: Tests for autoimmune markers (e.g., ANA, ANCA) may be performed to rule out systemic autoimmune diseases that cause orbital inflammation.
- Thyroid Function Tests: Due to the overlap with thyroid eye disease, assessing thyroid function is critical to rule out this condition.
Orbital Pseudotumor Treatment
The primary goal of treating orbital pseudotumor is to reduce inflammation, relieve symptoms, and avoid complications. Because the condition is idiopathic, immunosuppressive therapies are frequently used to treat it. Here are the primary approaches to managing orbital pseudotumor:
Corticosteroids 1. Systemic Corticosteroids: Prednisone, an oral corticosteroid, is the primary treatment for orbital pseudotumors. They are extremely effective at reducing inflammation and alleviating symptoms. The typical starting dose is high and gradually tapered over weeks to months, depending on the patient’s response.
- Intervenous Corticosteroids: In severe cases, high-dose intravenous corticosteroids (e.g., methylprednisolone) may be used to quickly control inflammation before switching to oral steroids.
Immunosuppressive Agents
Additional immunosuppressive agents may be used for patients who are resistant to corticosteroids or require long-term treatment to avoid steroid-related side effects.
- Methotrexate: A steroid-sparing immunosuppressive drug. It reduces inflammation with fewer side effects than long-term steroid use.
- Azathioprine: Another immunosuppressive agent that can help keep patients with orbital pseudotumor in remission.
- Cyclophosphamide: A more potent immunosuppressive drug used in refractory cases, but it carries a higher risk of adverse effects.
Radiation Therapy
When immunosuppressive therapy is either contraindicated or ineffective, low-dose external beam radiation therapy may be considered. Radiation reduces inflammation and can be especially beneficial in chronic or recurring cases.
Biological Agents
Emerging therapies using biologic agents are being investigated for their efficacy in treating orbital pseudotumor:
- Rituximab is a monoclonal antibody that targets CD20 on B-cells and has shown promise in treating refractory cases of orbital pseudotumor, particularly those associated with autoimmune conditions.
- Infliximab and Adalimumab: Tumor necrosis factor (TNF) inhibitors that can replace conventional immunosuppressive therapy.
Surgical Intervention
Surgery is typically reserved for cases where a biopsy is required to confirm the diagnosis or in rare cases where there is a severe structural impact on the orbit.
- Biopsy: Obtaining tissue samples for histopathological diagnosis and ruling out malignancy or other specific inflammatory conditions.
- Debulking Surgery: In severe cases where inflammation causes a large mass effect and compresses ocular structures, surgical debulking may be required to relieve pressure and preserve vision.
Supportive Care
Supportive care measures are essential for managing symptoms and improving quality of life:
- Pain Management: Managing inflammation-related pain with analgesics.
- Ocular Lubricants: Used to relieve dryness and irritation caused by an affected lacrimal gland.
Innovative and Emerging Therapies
Research is underway to identify new therapeutic targets and innovative treatments for orbital pseudotumor.
- Gene Therapy: Future therapies could use gene editing techniques to correct underlying genetic susceptibilities to inflammation.
- Targeted Molecular Therapies: Researchers are looking into drugs that target specific inflammatory pathways involved in the pathogenesis of orbital pseudotumors.
The severity of the condition, the patient’s response to initial therapies, and the presence of any underlying systemic conditions all influence the treatment plan chosen. Close monitoring and a multidisciplinary approach involving ophthalmologists, rheumatologists, and immunologists are essential for successful treatment.
Effective Ways to Improve and Prevent Orbital Pseudotumor
- Regular Eye Examinations: Routine eye exams can detect early signs of orbital inflammation and allow for timely intervention.
- Manage Autoimmune Conditions: If you have an autoimmune disorder, work closely with your doctor to keep it under control, as this may lower your chances of developing orbital pseudotumor.
- Healthy Lifestyle: Eat a well-balanced diet, exercise regularly, and get enough sleep to boost your immune system and lower inflammation.
- Avoid Smoking: Smoking can worsen inflammatory conditions and impair immune function, raising the risk of orbital pseudotumor.
- Stress Management: Yoga, meditation, and mindfulness techniques can help reduce stress, which is known to have an impact on immune response and inflammation.
- Early Treatment of Infections: Treating sinus or orbital infections promptly can prevent chronic inflammation, which may contribute to the development of orbital pseudotumor.
- Protective Eyewear: Wear protective eyewear when participating in activities that pose a risk of eye injury, as trauma can cause inflammatory responses in the orbit.
- Hydration and Nutrition: Stay hydrated and eat a diet rich in anti-inflammatory foods like fruits, vegetables, and omega-3 fatty acids.
- Regular Monitoring: If you have a history of orbital pseudotumor, regular monitoring and follow-up with a healthcare provider can help manage recurrences and adjust treatment as needed.
Trusted Resources
Books
- “Diseases of the Orbit: A Multidisciplinary Approach” by Jack Rootman
- “Orbital Disease: Imaging and Analysis” by Jack Rootman and A.D. Murray
- “Clinical Ophthalmology: A Systematic Approach” by Jack J. Kanski and Brad Bowling
Online Resources
- American Academy of Ophthalmology (AAO): aao.org
- National Eye Institute (NEI): nei.nih.gov
- American Society of Ophthalmic Plastic and Reconstructive Surgery (ASOPRS): asoprs.org






