The ovaries are central to the female reproductive system, responsible for producing oocytes (eggs) and secreting essential hormones that regulate the menstrual cycle and support pregnancy. These small but powerful organs also influence overall hormonal balance and health throughout a woman’s life. In this guide, we delve into the intricate anatomy of the ovaries, explore their vital physiological roles, and discuss common disorders—from benign cysts to ovarian cancer. We also review advanced diagnostic methods, modern treatments, and evidence-based lifestyle practices and supplements that can help maintain ovarian health and enhance fertility.
Table of Contents
- Ovarian Structure
- Physiology & Functions
- Ovarian Disorders
- Diagnostic Methods
- Treatment Strategies
- Nutritional & Supplementary Support
- Lifestyle & Preventive Practices
- Reliable Resources
- Frequently Asked Questions
Ovarian Structure
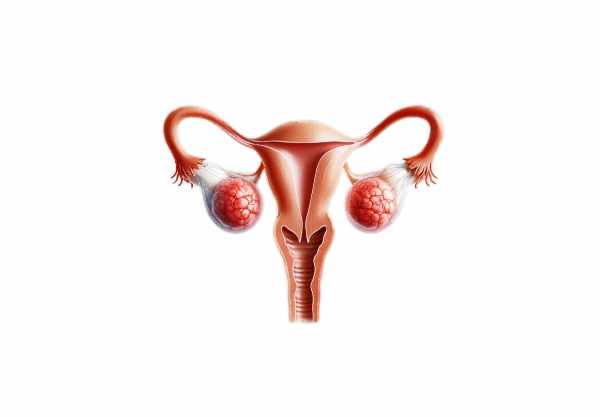
The ovaries, small paired organs located in the pelvic cavity, exhibit a sophisticated anatomy essential for reproductive function. Each ovary, roughly 3 cm in length, 1.5 cm in width, and 1 cm in thickness, is suspended by the mesovarium—a fold of peritoneum that attaches them to the broad ligament of the uterus.
Macroscopic Anatomy
- Location and Attachment:
The ovaries reside on either side of the uterus, secured by the ovarian ligament medially and the suspensory ligament (infundibulopelvic ligament) laterally. These attachments not only maintain the ovaries’ position but also serve as conduits for blood vessels, nerves, and lymphatics. - Surface Characteristics:
The ovarian surface is covered by the germinal epithelium, a simple cuboidal cell layer. Beneath this lies the tunica albuginea, a dense connective tissue capsule that offers protection and structural support. The surface often appears uneven due to the presence of developing follicles.
Internal Organization
- Cortex and Medulla:
The ovary is divided into two main regions: the cortex, which is the outer layer containing ovarian follicles at various developmental stages, and the medulla, composed of loose connective tissue that houses blood vessels, lymphatic channels, and nerves. - Follicular Architecture:
Within the cortex, ovarian follicles progress through distinct stages: - Primordial Follicles:
Present at birth, each contains a primary oocyte enveloped by a single layer of flattened granulosa cells. - Primary Follicles:
These develop from primordial follicles, marked by a transformation of granulosa cells into a single layer of cuboidal cells and the formation of the zona pellucida around the oocyte. - Secondary Follicles:
Characterized by multiple layers of granulosa cells and the formation of an antrum—a fluid-filled cavity. - Tertiary (Graafian) Follicles:
Mature follicles with a large antrum, ready for ovulation, and surrounded by a cumulus oophorus that supports the oocyte.
Vascular and Neural Supply
- Arterial Network:
The ovaries receive blood primarily via the ovarian arteries, direct branches of the abdominal aorta. These vessels traverse the suspensory ligament and anastomose with branches from the uterine arteries, ensuring robust blood flow. - Venous Return:
Venous blood is drained by the ovarian veins; the right ovarian vein empties into the inferior vena cava, while the left drains into the left renal vein. - Lymphatic Drainage and Innervation:
Lymphatic vessels follow the ovarian arteries to para-aortic lymph nodes. The ovaries are innervated by both sympathetic fibers (via the ovarian plexus) and parasympathetic fibers from the pelvic splanchnic nerves, regulating blood flow, hormone secretion, and follicular development.
Physiology & Functions
The ovaries are vital not only for fertility but also for regulating a wide array of hormonal processes that influence overall health. Their functions extend from oocyte production to the synthesis of hormones that orchestrate the menstrual cycle and support pregnancy.
Oocyte Production and Ovulation
- Oogenesis:
Oocyte production (oogenesis) begins during fetal development. Primordial germ cells develop into primary oocytes that become arrested in prophase I of meiosis. Although a woman is born with millions of these cells, only a few hundred thousand remain at puberty. - Follicular Maturation:
With each menstrual cycle, a group of follicles is recruited under the influence of follicle-stimulating hormone (FSH). Among these, one follicle typically matures into a Graafian follicle, ready to release an oocyte during ovulation. - Ovulation:
An increase in luteinizing hormone (LH) triggers the rupture of the mature follicle and the release of the oocyte into the peritoneal cavity. The oocyte is then captured by the fimbriae of the fallopian tube, initiating the potential for fertilization.
Hormone Production
- Estrogen:
Synthesized mainly by granulosa cells, estrogen is critical for the development of female secondary sexual characteristics, regulation of the menstrual cycle, and maintenance of reproductive tissues. - Progesterone:
Produced by the corpus luteum after ovulation, progesterone prepares the uterine lining for implantation, supports early pregnancy, and suppresses further ovulation during the luteal phase. - Inhibin and Activin:
These peptide hormones, secreted by granulosa cells, regulate FSH secretion via feedback mechanisms. Inhibin suppresses FSH release, while activin promotes it, thereby playing an essential role in follicular development.
The Menstrual Cycle
The menstrual cycle reflects the dynamic hormonal interplay orchestrated by the ovaries and can be divided into three phases:
- Follicular Phase:
Begins with menstruation and continues until ovulation. FSH stimulates the growth of ovarian follicles, leading to increased estrogen production and the thickening of the endometrial lining. - Ovulation:
A surge in LH causes the dominant follicle to rupture, releasing a mature oocyte, marking the peak of fertility. - Luteal Phase:
The corpus luteum forms and secretes progesterone, stabilizing the endometrium for potential implantation. If fertilization does not occur, the corpus luteum regresses, leading to a drop in hormone levels and the onset of menstruation.
Role in Pregnancy
During early pregnancy, the corpus luteum remains active and continues to produce progesterone to support the endometrium until the placenta takes over hormone production. This hormonal support is crucial for maintaining a pregnancy during its initial stages.
Life Stage Variations
- Puberty:
The onset of puberty triggers the activation of the hypothalamic-pituitary-ovarian axis, leading to the development of secondary sexual characteristics and the commencement of menstrual cycles. - Menopause:
As ovarian function declines with age, the reduction in estrogen and progesterone production leads to the cessation of menstruation and various systemic changes such as hot flashes, mood swings, and an increased risk of osteoporosis.
Ovarian Disorders
The ovaries can be affected by various conditions that impact reproductive health and overall well-being. Early detection and management are key to effective treatment and improved quality of life.
Ovarian Cysts
Ovarian cysts are fluid-filled sacs that commonly develop during the menstrual cycle. They can be categorized into:
- Functional Cysts:
These include follicular cysts (resulting from a follicle that fails to rupture) and corpus luteum cysts (formed when the corpus luteum fills with fluid). They are typically benign and resolve spontaneously. - Pathological Cysts:
These cysts, such as dermoid cysts, endometriomas, and cystadenomas, may require surgical intervention if they cause pain, become excessively large, or show signs of malignancy.
Polycystic Ovarian Syndrome (PCOS)
PCOS is a prevalent endocrine disorder characterized by:
- Multiple Small Follicles:
Ultrasound images often reveal numerous small, undeveloped follicles in the ovaries. - Hormonal Imbalances:
Elevated androgen levels can cause hirsutism, acne, and irregular menstrual cycles. - Metabolic Issues:
Insulin resistance and obesity are common, increasing the risk of type 2 diabetes and cardiovascular disease. - Management:
Treatment includes lifestyle modifications, hormonal therapies (oral contraceptives), and insulin sensitizers such as metformin.
Ovarian Cancer
Ovarian cancer is a serious and potentially life-threatening condition that is often diagnosed at an advanced stage due to vague early symptoms. It includes several types:
- Epithelial Ovarian Cancer:
The most common form, originating in the surface epithelium of the ovary. - Germ Cell Tumors:
Rare tumors that arise from the cells that produce eggs, typically affecting younger women. - Sex Cord-Stromal Tumors:
Tumors derived from the ovarian stroma, including granulosa cell tumors, which may secrete hormones.
Early detection through routine screenings, imaging, and biomarker tests is crucial for effective treatment, which may involve surgery, chemotherapy, and targeted therapies.
Endometriosis
Endometriosis occurs when tissue resembling the uterine lining grows outside the uterus, commonly affecting the ovaries. This can result in:
- Chronic Pelvic Pain:
Especially during menstruation. - Infertility:
Due to adhesions and scarring. - Menstrual Irregularities:
Abnormal bleeding patterns. - Management:
Treatment options include hormonal therapies, pain management, and, in some cases, surgical removal of ectopic endometrial tissue.
Premature Ovarian Insufficiency (POI)
Also known as premature menopause, POI occurs when the ovaries lose function before age 40.
- Symptoms:
Irregular or absent menstrual cycles, hot flashes, and infertility. - Causes:
Genetic factors, autoimmune disorders, or medical treatments such as chemotherapy. - Management:
Hormone replacement therapy (HRT) and fertility preservation techniques may be considered.
Ovarian Torsion
Ovarian torsion is an emergency condition in which an ovary twists around its supporting ligaments, compromising its blood supply.
- Presentation:
Sudden, severe pelvic pain, nausea, and vomiting. - Treatment:
Prompt surgical intervention to untwist the ovary and restore blood flow is essential to prevent tissue death.
Diagnostic Methods for Ovarian Disorders
A variety of diagnostic techniques are employed to accurately assess ovarian conditions. Early and precise diagnosis is crucial for optimal treatment outcomes.
Clinical Evaluation
- Medical History and Physical Exam:
A detailed history of menstrual patterns, pain, and other symptoms is taken, followed by a pelvic examination to palpate the ovaries and detect any masses or tenderness.
Imaging Techniques
- Ultrasound:
The primary imaging modality for ovarian evaluation, transvaginal ultrasound offers high-resolution images that can detect cysts, tumors, and other structural abnormalities. Doppler ultrasound can assess blood flow to detect conditions like torsion. - Magnetic Resonance Imaging (MRI):
MRI is used to provide detailed images of ovarian structures, especially useful for complex masses or when malignancy is suspected. - Computed Tomography (CT) Scan:
CT scans are employed, particularly in staging ovarian cancer, to evaluate the extent of disease and potential metastases.
Laboratory Testing
- Hormonal Assays:
Blood tests measure levels of FSH, LH, estradiol, progesterone, and androgens. Abnormal hormone levels can indicate conditions such as POI or PCOS. - Tumor Markers:
CA-125, HE4, and other biomarkers help in the diagnosis and monitoring of ovarian cancer. - Genetic Testing:
Testing for BRCA1, BRCA2, and other gene mutations is recommended for women with a family history of ovarian or breast cancer.
Laparoscopy and Biopsy
- Laparoscopy:
A minimally invasive procedure that allows direct visualization of the ovaries and pelvic cavity. It is useful for diagnosing endometriosis, ovarian cysts, and other conditions. - Biopsy:
Tissue samples obtained during laparoscopy or under image guidance are examined histologically to confirm diagnoses, particularly in suspected ovarian cancers.
Advanced Diagnostic Modalities
- Positron Emission Tomography (PET) Scan:
PET scans help assess metabolic activity of ovarian lesions and detect metastatic disease. - Molecular Profiling:
Next-generation sequencing (NGS) and other molecular tests provide detailed genetic information about ovarian tumors, facilitating personalized treatment strategies.
Treatment Strategies for Ovarian Conditions
Ovarian disorder management requires an individualized approach, considering factors such as age, symptom severity, reproductive goals, and overall health. Treatment options range from conservative medical management to surgical interventions and advanced therapies.
Medical Management
Hormonal Therapy
- Oral Contraceptives:
Birth control pills are used to regulate menstrual cycles, reduce ovarian cyst formation, and alleviate symptoms associated with PCOS and endometriosis. - Progesterone Therapy:
Progesterone supplements help manage irregular cycles and endometrial hyperplasia. - GnRH Agonists:
These drugs suppress ovarian hormone production and are used in severe cases of endometriosis or fibroids.
Insulin Sensitizers
- Metformin:
Often prescribed for women with PCOS, metformin improves insulin sensitivity, regulates menstrual cycles, and may enhance ovulatory function.
Pain Management
- NSAIDs and Analgesics:
Medications such as ibuprofen are used to manage pelvic pain associated with ovarian cysts and endometriosis.
Surgical Interventions
Minimally Invasive Procedures
- Laparoscopy:
A key diagnostic and therapeutic tool, laparoscopy enables the removal of ovarian cysts (cystectomy), treatment of endometriosis, and management of adhesions while preserving ovarian tissue. - Ovarian Cystectomy:
Removal of cysts while sparing the ovary, preserving fertility and hormonal function. - Oophorectomy:
In cases of malignancy or severe ovarian disease, the removal of one or both ovaries may be necessary.
Advanced Surgical Treatments
- Laparotomy:
Open surgery may be required for large or complex ovarian masses, especially in advanced ovarian cancer. - Debulking Surgery:
In ovarian cancer treatment, debulking involves the surgical removal of as much tumor tissue as possible to enhance the effectiveness of chemotherapy. - Hysterectomy with Salpingo-Oophorectomy:
For advanced ovarian or endometrial cancers, the surgical removal of the uterus, ovaries, and fallopian tubes may be performed.
Fertility Preservation and Assisted Reproduction
For women concerned about fertility preservation, especially before cancer treatments:
- Ovarian Tissue Cryopreservation:
This involves the removal and freezing of ovarian tissue for later transplantation. - Ovulation Induction and IVF:
Treatments like clomiphene citrate or letrozole stimulate the ovaries to produce multiple eggs, which can be harvested for in vitro fertilization (IVF).
Cancer-Specific Treatments
Ovarian Cancer Management
- Surgical Management:
Primary treatment typically involves debulking surgery to remove ovarian tumors and affected tissues. - Chemotherapy:
Post-surgical chemotherapy with drugs like paclitaxel and carboplatin is standard for ovarian cancer. - Targeted Therapy and Immunotherapy:
Newer approaches include PARP inhibitors for BRCA-mutated cancers and monoclonal antibodies targeting specific molecular pathways.
Emerging Therapies
- Precision Medicine:
Tailoring treatment based on the genetic profile of ovarian tumors allows for more targeted and effective therapies. - Gene Therapy:
Experimental approaches aim to modify genetic pathways involved in ovarian cancer, offering potential future treatment options. - Immunotherapy:
Approaches such as immune checkpoint inhibitors are under investigation for their potential to boost the immune response against ovarian cancer.
Nutritional & Supplementary Support for Ovarian Health
Nutritional support and dietary supplements can play a significant role in maintaining ovarian function and overall reproductive health. A well-balanced diet, rich in essential vitamins, minerals, and antioxidants, supports the ovaries’ metabolic and endocrine functions.
Essential Nutrients and Vitamins
- Omega-3 Fatty Acids:
Found in fish oil and flaxseed, omega-3s possess anti-inflammatory properties that may help reduce ovarian cyst formation and promote hormonal balance. - Vitamin D:
Adequate vitamin D levels are associated with improved ovarian function, better menstrual regulation, and reduced risk of PCOS. - B Vitamins:
B6, B12, and folic acid are critical for energy production and hormone metabolism. They help lower homocysteine levels and support overall ovarian function. - Antioxidants (Vitamins C & E):
These vitamins protect ovarian cells from oxidative stress and support overall reproductive health.
Herbal Supplements and Adaptogens
- Inositol (Myo- and D-Chiro-Inositol):
Proven to improve ovarian function in PCOS, inositol aids in insulin regulation and promotes ovulation. - Vitex (Chasteberry):
This herb is used to balance hormonal levels and regulate the menstrual cycle, thereby supporting ovarian health. - Maca Root:
An adaptogenic herb that can help balance hormones, reduce stress, and enhance fertility.
Enzymes and Antioxidants
- Coenzyme Q10 (CoQ10):
A potent antioxidant that boosts cellular energy production and has been shown to improve egg quality, particularly in older women. - Alpha Lipoic Acid:
This antioxidant helps lower oxidative stress and improve insulin sensitivity, benefiting ovarian function. - N-Acetylcysteine (NAC):
NAC supports detoxification and reduces oxidative stress, making it beneficial for women with PCOS.
Hormonal Supplements
- DHEA:
Dehydroepiandrosterone can help improve ovarian reserve and egg quality in women with diminished ovarian function. It is often used in conjunction with fertility treatments.
Lifestyle & Preventive Practices for Ovarian Wellness
Sustaining ovarian health requires a holistic approach that encompasses diet, exercise, stress management, and routine medical care. The following practices can help optimize ovarian function and enhance overall reproductive well-being.
- Adopt a Nutritious Diet:
Consume a balanced diet rich in fruits, vegetables, lean proteins, whole grains, and healthy fats. Focus on antioxidant-rich foods that combat oxidative stress. - Engage in Regular Physical Activity:
Regular exercise promotes hormonal balance, improves insulin sensitivity, and maintains a healthy weight—all crucial for optimal ovarian function. - Manage Stress Effectively:
Stress can disrupt hormonal balance. Practices such as yoga, meditation, and deep breathing exercises can help manage stress and support ovarian health. - Maintain a Healthy Weight:
Achieving and maintaining a healthy weight reduces the risk of PCOS and other ovarian disorders. Weight management through diet and exercise is key to hormonal regulation. - Monitor Menstrual Patterns:
Keeping track of your menstrual cycle can help detect irregularities early. Consistent changes in cycle length or flow may indicate underlying ovarian issues. - Avoid Exposure to Toxins:
Limit exposure to environmental toxins, endocrine disruptors, and chemicals that may adversely affect ovarian function. Opt for natural and organic products when possible. - Regular Gynecological Examinations:
Routine check-ups with your healthcare provider can help monitor ovarian health, detect abnormalities early, and address any concerns promptly. - Stay Hydrated:
Proper hydration is essential for overall cellular health, including the cells within the ovaries. Aim to drink at least eight glasses of water per day. - Consider Supplementation:
If dietary intake is insufficient, consult a healthcare provider about taking supplements such as omega-3s, vitamin D, and antioxidants to support ovarian function. - Avoid Smoking and Limit Alcohol:
Smoking and excessive alcohol consumption negatively impact ovarian health by disrupting hormone balance and reducing fertility. Abstaining or moderating these habits is essential.
Reliable Resources for Ovarian Health
For further reading and support on ovarian health, consider these trusted resources, which offer comprehensive information from both clinical and lifestyle perspectives.
Recommended Books
- “Taking Charge of Your Fertility” by Toni Weschler:
An essential guide to understanding menstrual cycles, fertility, and reproductive health. - “The Woman Code” by Alisa Vitti:
Offers insights into hormonal balance, dietary recommendations, and lifestyle changes for enhancing ovarian and overall reproductive health. - “PCOS SOS: A Gynecologist’s Lifeline to Naturally Restore Your Rhythms, Hormones, and Happiness” by Felice Gersh, M.D.:
Provides practical advice and natural strategies for managing PCOS and supporting ovarian function.
Academic Journals
- Fertility and Sterility:
A leading journal in reproductive medicine, it publishes peer-reviewed research on ovarian function, infertility treatments, and hormonal health. - Journal of Ovarian Research:
Focuses on the latest research in ovarian biology, pathology, and treatment options.
Mobile Applications
- Clue: Period & Cycle Tracker:
A comprehensive app for tracking menstrual cycles, ovulation, and symptoms to help manage reproductive health. - Ovia Fertility & Cycle Tracker:
Provides personalized insights on menstrual health, ovulation, and fertility, along with health tips for optimal ovarian function. - MyFLO Period Tracker:
Created by Alisa Vitti, this app helps women understand their hormonal patterns and offers tailored recommendations for maintaining reproductive health.
Frequently Asked Questions
What are the main functions of the ovaries?
The ovaries produce and release oocytes for fertilization and secrete essential hormones such as estrogen and progesterone that regulate the menstrual cycle, support pregnancy, and maintain overall reproductive health.
How do ovarian follicles develop during the menstrual cycle?
Follicular development begins with primordial follicles, progresses through primary and secondary stages, and culminates in a mature Graafian follicle that releases an oocyte during ovulation. Only one follicle typically reaches maturity each cycle.
What is PCOS, and how does it affect ovarian function?
Polycystic Ovarian Syndrome (PCOS) is an endocrine disorder characterized by multiple small ovarian follicles, hormonal imbalances, and menstrual irregularities. It can lead to symptoms such as hirsutism, acne, and infertility, and is often managed through lifestyle changes and hormonal treatments.
When is surgical treatment required for ovarian disorders?
Surgical interventions may be necessary for large or symptomatic ovarian cysts, severe endometriosis, ovarian torsion, or ovarian cancer. The specific procedure depends on the condition’s severity and the patient’s reproductive goals.
How can lifestyle changes improve ovarian health?
A balanced diet, regular exercise, stress management, and avoiding toxins help maintain hormonal balance and overall ovarian function. Routine health check-ups and proper supplementation also support ovarian health.
Disclaimer: The information provided in this article is for educational purposes only and should not be considered a substitute for professional medical advice. Always consult with a qualified healthcare provider regarding any medical concerns.
If you found this article informative, please share it on Facebook, X (formerly Twitter), or your preferred social media platform. Your support helps spread valuable health insights and encourages others to maintain optimal ovarian health.