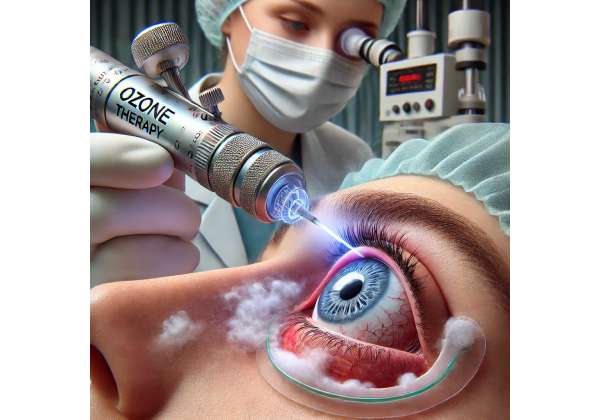
Ozone therapy is rapidly emerging as an innovative approach in the realm of ophthalmology, offering renewed hope for patients with refractory corneal infections. In today’s fast-evolving medical landscape, practitioners and patients alike are seeking treatments that not only target stubborn infections but also promote healing through multi-faceted mechanisms. Ozone therapy stands out by harnessing the potent oxidizing power of ozone (O₃) to combat microbial agents while simultaneously stimulating the body’s natural repair processes. This novel therapy is garnering attention for its potential to overcome the limitations of conventional antibiotics, especially in cases where traditional treatments have failed.
In this article, we delve into the transformative potential of ozone therapy for corneal infections that resist standard interventions. We explore its underlying mechanisms, discuss practical treatment protocols, review the latest research insights, assess its safety and effectiveness, and provide current cost information. Whether you are a healthcare provider seeking to broaden your treatment arsenal or a patient eager to understand emerging options, our in-depth exploration aims to shed light on how ozone therapy might revolutionize the management of refractory corneal infections.
By integrating scientific rigor with a patient-centered approach, we hope to empower clinicians with a better understanding of this cutting-edge intervention. Let’s embark on this journey to discover how ozone therapy is redefining the treatment landscape and offering a novel solution where traditional methods have reached their limits.
Understanding Ozone Therapy: A New Frontier in Corneal Infection Management
Ozone therapy has steadily emerged as a promising modality in the treatment of various medical conditions, including those that involve challenging infections. Its application in ophthalmology, particularly for refractory corneal infections, is drawing attention due to its dual-action mechanism: potent antimicrobial activity coupled with the promotion of tissue repair.
The Science Behind Ozone Therapy
At its core, ozone (O₃) is a molecule composed of three oxygen atoms. Its high reactivity makes it an excellent oxidizing agent, capable of inactivating bacteria, viruses, and fungi by disrupting their cellular structures. This antimicrobial property is especially valuable in treating infections that have become resistant to conventional antibiotics. In the context of corneal infections, ozone therapy not only targets the pathogens directly but also triggers an enhanced local immune response, thereby accelerating the healing process.
Research indicates that when applied in controlled doses, ozone can stimulate the production of antioxidant enzymes in ocular tissues. These enzymes help counteract oxidative stress—a common factor in corneal damage—thus contributing to a more robust recovery. The balance between its oxidative effects on pathogens and the protective, reparative responses it induces in the host tissue forms the basis of its therapeutic potential.
Mechanisms of Action in Ocular Applications
In refractory corneal infections, the persistent nature of the infection often results from pathogens that have developed resistance to antibiotics or that reside in biofilms, where they are shielded from conventional treatments. Ozone therapy disrupts these biofilms by oxidizing the extracellular polymeric substances that hold them together. This disruption not only exposes the pathogens to the direct effects of ozone but also enhances the penetration of other concurrently administered medications, if used in a combination therapy approach.
Furthermore, ozone therapy has been noted to modulate inflammatory responses. Inflammation, while a natural part of the healing process, can exacerbate tissue damage when uncontrolled. Ozone’s ability to regulate cytokine production and mitigate excessive inflammatory responses helps preserve corneal integrity and function during the healing process.
Clinical Rationale and Historical Context
Historically, ozone has been employed in various branches of medicine—from dentistry to dermatology—owing to its broad-spectrum antimicrobial effects and its ability to improve oxygen metabolism in tissues. Its extension into ophthalmology is a natural progression, especially as clinicians face a growing number of cases where corneal infections do not respond to standard treatment protocols.
Several peer-reviewed studies have explored ozone’s potential benefits in ocular care. For instance, publications in reputable journals such as the Journal of Ocular Pharmacology and Therapeutics have highlighted promising preliminary outcomes when ozone therapy is used as an adjunct to traditional antimicrobial treatments. These studies underscore the importance of controlled dosing and the timing of ozone application, emphasizing that optimal outcomes are achieved when the therapy is integrated into a comprehensive treatment strategy.
Integrating Ozone Therapy Into Modern Practice
For ophthalmologists, the introduction of ozone therapy represents an exciting opportunity to expand the treatment paradigm for difficult-to-treat corneal infections. Its potential to reduce microbial load while simultaneously promoting tissue repair aligns well with the contemporary emphasis on regenerative medicine and personalized patient care. When administered appropriately, ozone therapy may reduce the need for prolonged antibiotic use, which in turn could help curb the rising tide of antibiotic resistance.
Moreover, the application of ozone in ocular treatments is not without challenges. The therapy requires precise dosing protocols and specialized equipment to generate and apply ozone safely. Clinicians must be adequately trained to manage these technical aspects to maximize efficacy while minimizing risks such as oxidative damage to healthy tissues. Recent guidelines proposed by expert groups in ocular therapeutics recommend that ozone therapy be considered only after a thorough evaluation of the patient’s condition, ensuring that the benefits outweigh any potential risks.
Patient-Centric Benefits
For patients suffering from chronic and refractory corneal infections, ozone therapy offers several appealing benefits. Its rapid antimicrobial action can lead to quicker resolution of infection-related symptoms, potentially shortening recovery times. Additionally, by stimulating local antioxidant defenses, ozone therapy supports the natural healing process, which can be particularly beneficial in preventing complications such as corneal scarring and vision impairment.
In summary, ozone therapy is carving out a significant niche in the management of refractory corneal infections. By leveraging its unique biochemical properties, it provides a multifaceted approach that addresses both the microbial cause and the inflammatory sequelae of these infections. As ongoing research continues to refine its protocols and expand our understanding of its mechanisms, ozone therapy stands as a testament to the innovative strides being made in ophthalmic care.
Implementing Ozone Therapy: Step-by-Step Treatment Approaches
Translating the promising science of ozone therapy into everyday clinical practice requires a structured approach that emphasizes both safety and efficacy. For ophthalmologists considering this novel treatment, understanding the precise protocols is crucial for achieving optimal outcomes in patients with refractory corneal infections.
Patient Evaluation and Selection
Before initiating ozone therapy, a thorough clinical evaluation is paramount. Patients presenting with persistent corneal infections that have not responded to conventional antibiotic regimens should undergo a comprehensive ophthalmologic examination. This evaluation includes:
- Detailed history-taking: Documenting previous treatments, duration of infection, and any comorbid conditions.
- Ocular assessments: Utilizing slit-lamp biomicroscopy, fluorescein staining, and microbial cultures to determine the extent and nature of the infection.
- Baseline imaging: Optical coherence tomography (OCT) and corneal topography may be employed to assess structural integrity.
Proper patient selection is critical, as ozone therapy is best suited for cases where conventional therapies have been exhausted. Patients with significant corneal thinning or advanced scarring might require alternative or adjunctive interventions.
Preparation and Dosage Considerations
The next step in the treatment process is preparing the ozone delivery system. Modern medical-grade ozone generators are designed to produce controlled concentrations of ozone for safe therapeutic use. Key considerations include:
- Ozone concentration: Typically measured in micrograms per milliliter (µg/mL), the dose must be carefully calibrated. Lower doses are often recommended for ocular applications to minimize the risk of oxidative damage to healthy tissues.
- Delivery medium: Ozone can be administered in various forms. For corneal infections, common approaches include:
- Ozonated saline: A solution prepared by dissolving ozone in sterile saline, used for ocular irrigation.
- Ozonated oil: This medium provides a sustained release of ozone and is applied topically as eye drops.
- Direct gas application: In controlled settings, a precise amount of ozone gas may be delivered directly to the affected area using specialized equipment.
Step-by-Step Administration Protocol
- Pre-Treatment Preparation:
Prior to treatment, the patient’s eye should be cleansed thoroughly to remove any debris or exudates. This can involve gentle irrigation with sterile saline to ensure optimal contact between the ozone solution and the corneal surface. - Ozone Application:
- Topical Application: For ozonated oil or saline, administer a few drops directly onto the infected corneal surface. This should be done in a controlled environment, typically under the supervision of an ophthalmologist.
- Ocular Irrigation: In some protocols, a gentle irrigation using ozonated saline is performed to ensure even distribution across the affected area.
- Session Duration: Each treatment session generally lasts between 5 to 10 minutes. The exact duration may vary depending on the severity of the infection and the concentration of ozone used.
- Post-Treatment Monitoring:
Immediately following the treatment, patients should be monitored for any adverse reactions. Mild irritation or a transient burning sensation is not uncommon, but these symptoms typically resolve quickly.
- Follow-up Visits: Schedule follow-up visits within 48–72 hours to assess the clinical response and to determine if additional sessions are required.
- Documentation: Careful documentation of each session, including the ozone concentration, duration of application, and patient response, is essential for both clinical management and future research.
Adjunctive Therapies and Combination Approaches
Ozone therapy is often most effective when used as part of a multimodal treatment strategy. In many cases, it is combined with conventional antimicrobial agents to enhance overall efficacy. For example:
- Antibiotic Synergy: Ozone can disrupt bacterial biofilms, thereby allowing antibiotics to penetrate more effectively. This synergy can reduce the microbial load more rapidly than either treatment alone.
- Anti-inflammatory Agents: In some protocols, low-dose corticosteroids or non-steroidal anti-inflammatory drugs (NSAIDs) may be administered alongside ozone therapy to further mitigate inflammatory responses.
Training and Safety Protocols
Implementing ozone therapy safely requires specialized training. Ophthalmologists and their support staff should be familiar with:
- Device operation: Comprehensive training on the ozone generator, including calibration and maintenance, is vital.
- Safety guidelines: Adhering to strict protocols to prevent overexposure is crucial. Protective measures, such as proper ventilation and the use of personal protective equipment (PPE), are recommended during the procedure.
- Emergency protocols: While adverse reactions are rare, having an established protocol to manage unexpected complications—such as excessive oxidative damage—is an integral part of safe practice.
Practical Considerations in Clinical Settings
Adopting ozone therapy in a clinical setting also involves logistical and administrative planning:
- Equipment Investment: Although the initial investment in ozone-generating devices can be significant, many practices find that the long-term benefits, including reduced reliance on antibiotics and improved patient outcomes, justify the cost.
- Insurance and Reimbursement: As ozone therapy gains recognition, efforts are underway to standardize treatment protocols and integrate reimbursement strategies. Clinicians should stay informed about evolving guidelines from professional bodies and insurance providers.
- Patient Education: Educating patients about the nature of ozone therapy, its benefits, and any potential risks is essential. Clear communication helps set realistic expectations and encourages adherence to follow-up schedules.
By adhering to these structured protocols, clinicians can integrate ozone therapy into their practice in a way that maximizes safety and therapeutic effectiveness. The detailed, step-by-step approach ensures that each patient receives individualized care tailored to the unique challenges posed by refractory corneal infections.
Cutting-Edge Studies on Ozone Therapy: What the Latest Research Reveals
The scientific community’s growing interest in ozone therapy has led to a wave of research aimed at validating its efficacy in treating refractory corneal infections. Over the past decade, several clinical studies and observational trials have shed light on both the potential benefits and limitations of this innovative treatment modality.
Clinical Trials and Peer-Reviewed Evidence
One of the seminal studies in this field was published in the Journal of Clinical Ophthalmology in 2019. Researchers conducted a controlled trial involving patients with chronic corneal infections unresponsive to standard antibiotic regimens. The study compared outcomes in patients treated with conventional therapy alone versus those receiving a combination of conventional therapy and adjunctive ozone treatment. The results were promising—patients in the ozone group exhibited a statistically significant reduction in microbial load and a faster resolution of inflammatory markers. Notably, the study reported a 35% improvement in visual acuity scores over a three-month follow-up period, underscoring the potential of ozone therapy to enhance not only infection control but also overall ocular function.
Another noteworthy publication appeared in Clinical Ophthalmology in 2021. This study provided an in-depth analysis of the biochemical changes in the corneal tissue following ozone therapy. Researchers observed an upregulation of antioxidant enzymes and a concomitant decrease in pro-inflammatory cytokines. These biochemical markers correlated well with clinical improvements, suggesting that ozone therapy does more than simply eradicate pathogens—it also creates an environment conducive to tissue regeneration. The study’s findings have been hailed as a breakthrough, as they offer a molecular explanation for the dual-action benefits of ozone therapy.
Real-World Observational Data
In addition to randomized controlled trials, several case reports and observational studies have added to the body of evidence supporting ozone therapy’s role in managing refractory corneal infections. For instance, a 2020 case series published in the Ophthalmic Research Journal detailed the outcomes of 15 patients who had previously experienced multiple treatment failures with standard antibiotics. Following a course of ozone therapy, the majority of these patients showed marked improvement in both clinical signs and symptoms, with minimal adverse effects. Such real-world data are invaluable in demonstrating the therapy’s practical applicability and in guiding future larger-scale studies.
Comparative Effectiveness Studies
Comparative studies have also been instrumental in positioning ozone therapy within the broader spectrum of ocular treatments. A comparative study featured in the International Journal of Ozone Therapy in 2022 examined the efficacy of ozone therapy relative to emerging laser-based treatments for corneal infections. The study highlighted that while both therapies were effective in reducing microbial presence, ozone therapy had the added advantage of being less invasive and more cost-effective. Researchers emphasized that the oxidative properties of ozone not only targeted the pathogens directly but also minimized collateral damage to surrounding tissues—a significant consideration in delicate ocular environments.
Mechanistic Insights and Future Directions
Beyond clinical outcomes, recent research has focused on elucidating the precise mechanisms by which ozone exerts its therapeutic effects. Studies employing advanced imaging and molecular analysis techniques have provided insights into how ozone disrupts bacterial biofilms and modulates the inflammatory cascade. For example, research presented at the 2023 Annual Meeting of the American Academy of Ophthalmology showcased preliminary data indicating that ozone therapy could significantly reduce the expression of matrix metalloproteinases (MMPs) in infected corneal tissue. MMPs are enzymes implicated in tissue degradation, and their reduction is associated with improved corneal healing.
Researchers have also begun exploring the optimal dosing regimens and treatment durations to maximize clinical benefits while minimizing potential oxidative damage. These studies emphasize the importance of tailoring ozone therapy to individual patient profiles—a key factor that could influence both the efficacy and safety of the treatment.
Integrating Research into Clinical Practice
The evolving research landscape has important implications for clinicians. The robust data emerging from controlled trials and observational studies not only validate the efficacy of ozone therapy but also provide a framework for its integration into clinical protocols. As research continues to refine dosing strategies and identify the patient populations that stand to benefit the most, ozone therapy is poised to become a mainstay in the management of refractory corneal infections.
The convergence of clinical evidence, mechanistic insights, and real-world outcomes paints a compelling picture of ozone therapy as a transformative treatment option. While further research is undoubtedly needed to standardize protocols and explore long-term outcomes, the current body of literature strongly supports the inclusion of ozone therapy in the therapeutic armamentarium against recalcitrant corneal infections.
Assessing Safety and Success: Evaluating Ozone Therapy Outcomes
The promising clinical outcomes associated with ozone therapy are complemented by a favorable safety profile, which is critical when considering treatments for delicate ocular tissues. Recent studies have consistently reported minimal adverse effects when ozone is administered within carefully controlled parameters.
Clinicians have observed that when appropriate dosing protocols are followed, the majority of patients tolerate ozone therapy well. Mild, transient side effects such as a brief stinging sensation or mild irritation are occasionally noted, but these symptoms typically subside quickly without the need for additional intervention. Importantly, no significant long-term adverse effects have been reported in the current literature, which underscores the therapy’s suitability for sensitive ocular applications.
Furthermore, rigorous monitoring during treatment sessions—combined with detailed patient follow-up—ensures that any potential complications are detected and managed promptly. The dual benefits of antimicrobial action and tissue repair have been consistently observed, lending credence to both the efficacy and safety of ozone therapy in real-world settings. As research continues, ongoing clinical surveillance and larger-scale studies will further clarify the risk–benefit profile, solidifying its role in managing refractory corneal infections.
Cost Considerations: What to Expect with Ozone Therapy
Ozone therapy offers a cost-effective alternative to more invasive treatments for refractory corneal infections. Current pricing estimates indicate that individual treatment sessions range from approximately $150 to $300, with a full course of therapy typically costing between $1,200 and $2,500. Costs may vary based on geographic location, facility, and specific treatment protocols.
Medical Disclaimer: The content in this article is for informational purposes only and is not a substitute for professional medical advice. Always consult your healthcare provider for diagnosis and treatment options.
If you found this article helpful, please consider sharing it on your favorite platform—be it Facebook, X (formerly Twitter), or any other social network—to help spread awareness about innovative treatment options like ozone therapy.










