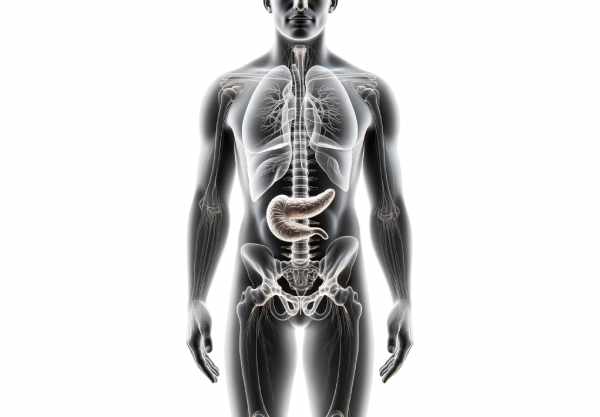
The pancreas is a vital organ located in the upper abdomen that plays a dual role in the body’s digestive and endocrine systems. It produces digestive enzymes essential for breaking down food and secretes hormones that regulate blood sugar levels. Its proper functioning is crucial for overall metabolic homeostasis and nutrient absorption. In this guide, we explore the intricate anatomy of the pancreas, delve into its complex physiological functions, review common disorders that affect it, and discuss a range of modern treatments and lifestyle practices designed to support pancreatic health.
Table of Contents
- Anatomy & Structure
- Physiological Mechanisms
- Common Disorders
- Diagnostic Approaches
- Treatment Options
- Nutritional Support
- Lifestyle & Preventive Practices
- Trusted Resources
- Frequently Asked Questions
Anatomy & Structure
The pancreas is a retroperitoneal, elongated organ that stretches horizontally across the posterior abdominal wall. It is divided into four distinct regions: the head, neck, body, and tail—each with unique relationships to surrounding structures.
Macroscopic Features
- Head:
The broad head is nestled in the curve of the duodenum and partly encircled by it. The uncinate process, a projection from the lower head, curves around vital blood vessels such as the superior mesenteric vessels. - Neck:
A short, narrow segment lies between the head and the body. It is positioned anterior to the confluence of the splenic and superior mesenteric veins, which join to form the portal vein. - Body:
Extending leftward from the neck, the body lies posterior to the stomach and in front of the splenic vein and left kidney. This portion contains the majority of the exocrine tissue responsible for enzyme production. - Tail:
The tail is the narrow, tapering end of the pancreas that reaches the splenic hilum. Unlike the other parts, the tail is intraperitoneal, enclosed by the splenorenal ligament.
Microscopic Architecture
The pancreas is a compound gland composed of both exocrine and endocrine tissues.
Exocrine Component
- Acinar Cells:
Organized in lobules, these cells synthesize digestive enzymes—amylase, lipase, and proteolytic enzymes (trypsinogen and chymotrypsinogen). They secrete their enzyme-rich fluid into a network of ducts. - Ductal Cells:
These cells line the interconnecting ducts that channel pancreatic secretions toward the duodenum. They secrete a bicarbonate-rich fluid, which neutralizes gastric acid entering the small intestine. - Main Duct System:
The small ducts coalesce to form the main pancreatic duct (Wirsung duct), which typically joins the common bile duct at the hepatopancreatic ampulla (ampulla of Vater). An accessory duct (Santorini) may also be present.
Endocrine Component
- Islets of Langerhans:
Scattered throughout the pancreas, these clusters comprise several cell types: - Beta Cells: Produce insulin, critical for reducing blood glucose levels.
- Alpha Cells: Secrete glucagon, which increases blood glucose.
- Delta Cells: Release somatostatin to modulate insulin and glucagon secretion.
- PP Cells: Secrete pancreatic polypeptide, which helps regulate both endocrine and exocrine pancreatic activities.
- Epsilon Cells: Produce ghrelin, the appetite-stimulating hormone.
Vascular and Lymphatic Networks
- Blood Supply:
The pancreas is richly vascularized. The head is supplied by the superior and inferior pancreaticoduodenal arteries, while the body and tail receive blood from branches of the splenic artery. Venous drainage is primarily via pancreatic veins that feed into the portal vein. - Lymphatic Drainage:
Lymph from the pancreas drains into the para-aortic, celiac, and superior mesenteric lymph nodes, playing a role in immune surveillance.
Innervation
The pancreas receives autonomic innervation:
- Sympathetic Fibers: Originating from the celiac and superior mesenteric plexuses, they regulate blood flow and modulate enzyme secretion.
- Parasympathetic Fibers: Derived from the vagus nerve, these fibers stimulate digestive enzyme release and insulin secretion.
Physiological Mechanisms
The pancreas serves dual roles in digestion and hormonal regulation, making it essential to both nutrient processing and metabolic control.
Exocrine Functions
Digestive Enzyme Production
- Acinar Secretion:
Acinar cells produce inactive precursor enzymes (zymogens) such as trypsinogen, chymotrypsinogen, amylase, and lipase. These enzymes remain inactive within the pancreas to prevent autodigestion. - Activation in the Duodenum:
Upon reaching the duodenum, the enzyme enterokinase converts trypsinogen into trypsin, which then activates other digestive enzymes, facilitating the breakdown of proteins, carbohydrates, and fats.
Bicarbonate Secretion
Ductal cells secrete bicarbonate-rich fluid, which neutralizes the acidic chyme from the stomach. This adjustment creates an optimal pH environment for digestive enzymes to function effectively in the small intestine.
Endocrine Functions
Hormonal Regulation
The islets of Langerhans secrete hormones directly into the bloodstream to regulate blood sugar levels and energy metabolism.
- Insulin:
Produced by beta cells, insulin facilitates the uptake of glucose into cells and promotes glycogen synthesis, thereby lowering blood sugar levels. - Glucagon:
Secreted by alpha cells, glucagon stimulates glycogenolysis and gluconeogenesis in the liver, raising blood glucose levels during fasting. - Somatostatin:
Delta cells produce somatostatin, which modulates the secretion of insulin, glucagon, and gastrointestinal hormones, maintaining a balance in nutrient absorption and metabolism. - Pancreatic Polypeptide & Ghrelin:
These hormones further fine-tune digestive processes and energy homeostasis.
Integration of Exocrine and Endocrine Roles
The pancreas coordinates its exocrine and endocrine functions to maintain metabolic homeostasis. Neural and hormonal signals, such as those from the vagus nerve and gastrointestinal hormones (e.g., cholecystokinin and secretin), trigger the release of digestive enzymes and bicarbonate in response to food intake while simultaneously regulating blood glucose levels.
Common Pancreatic Disorders
A range of disorders can affect the pancreas, impairing its digestive and hormonal functions. Recognizing these conditions early is critical for effective management and improving patient outcomes.
Pancreatitis
Acute Pancreatitis
- Etiology:
Most commonly caused by gallstones or excessive alcohol consumption, acute pancreatitis presents with sudden, severe abdominal pain, nausea, vomiting, and fever. - Complications:
It can lead to pancreatic necrosis, abscess formation, and systemic inflammatory response syndrome (SIRS). - Management:
Treatment includes supportive care (fluids, pain management), nutritional support, and sometimes antibiotics.
Chronic Pancreatitis
- Pathophysiology:
Persistent inflammation, often due to long-term alcohol abuse or genetic factors, leads to irreversible damage to pancreatic tissue. - Symptoms:
Chronic abdominal pain, malabsorption, weight loss, and diabetes may develop. - Treatment:
Management involves enzyme replacement, pain control, and lifestyle modifications.
Pancreatic Cancer
- Types:
The most common is epithelial ovarian cancer, but pancreatic cancer can also include rare types like neuroendocrine tumors. - Risk Factors:
Smoking, chronic pancreatitis, family history, and certain genetic mutations increase risk. - Symptoms:
Weight loss, jaundice, abdominal pain, and digestive issues are typical. - Treatment:
Often involves a combination of surgery (e.g., Whipple procedure), chemotherapy, radiation therapy, and targeted therapy.
Diabetes Mellitus
Type 1 Diabetes
- Mechanism:
An autoimmune destruction of beta cells leads to insulin deficiency. - Presentation:
Typically appears in childhood or adolescence with symptoms such as excessive thirst, frequent urination, and weight loss. - Management:
Requires lifelong insulin therapy and careful monitoring of blood glucose levels.
Type 2 Diabetes
- Pathophysiology:
Characterized by insulin resistance and relative insulin deficiency, it is often associated with obesity and sedentary lifestyles. - Symptoms:
Develop gradually and include fatigue, frequent urination, and blurred vision. - Management:
Involves lifestyle modifications, oral medications, and sometimes insulin therapy.
Cystic Fibrosis
- Impact on the Pancreas:
Genetic mutations cause thick, viscous secretions that obstruct pancreatic ducts, leading to chronic pancreatitis, malabsorption, and diabetes. - Management:
Involves pancreatic enzyme replacement, nutritional support, and management of respiratory complications.
Pancreatic Insufficiency
- Cause:
Often results from chronic pancreatitis, cystic fibrosis, or pancreatic cancer. - Manifestations:
Poor nutrient absorption, steatorrhea (fatty stools), weight loss, and nutritional deficiencies. - Treatment:
Pancreatic enzyme replacement therapy (PERT) and dietary modifications are key to managing this condition.
Pancreatic Cysts and Pseudocysts
- Cysts:
Fluid-filled sacs that may be benign (functional cysts) or have malignant potential. Dermoid cysts, endometriomas, and cystadenomas are examples. - Pseudocysts:
Collections of pancreatic fluid and necrotic tissue that typically follow acute pancreatitis. - Management:
Small cysts often resolve on their own, while larger or symptomatic cysts may require drainage or surgical removal.
Pancreatic Neuroendocrine Tumors (PNET)
- Characteristics:
Rare tumors that originate from the endocrine cells of the pancreas. They may secrete hormones (functional) or not (non-functional). - Clinical Impact:
Functional tumors can cause hormone-related symptoms such as hypoglycemia or gastrinoma syndrome. - Treatment:
Options include surgical resection, targeted therapies, and hormone-inhibiting medications.
Hereditary Pancreatitis
- Etiology:
A genetic disorder caused by mutations in genes such as PRSS1 and SPINK1, leading to recurrent episodes of pancreatitis starting in childhood. - Risks:
Increases the likelihood of chronic pancreatitis and pancreatic cancer. - Management:
Focuses on pain control, nutritional support, and monitoring for long-term complications.
Diagnostic Methods for Pancreatic Conditions
A comprehensive approach to diagnosing pancreatic disorders involves clinical evaluation, imaging, laboratory testing, and sometimes invasive procedures.
Clinical Assessment
- Medical History and Physical Examination:
A detailed history focuses on symptoms like abdominal pain, weight loss, and changes in digestion. Physical examination may reveal tenderness, palpable masses, or signs of malnutrition.
Imaging Studies
- Ultrasound:
Often the first-line imaging modality due to its non-invasive nature, ultrasound can identify cysts, masses, and signs of inflammation. - Endoscopic Ultrasound (EUS):
Provides high-resolution images of the pancreas by inserting an endoscope with an ultrasound probe through the stomach and duodenum. It is especially useful for small lesions and guiding fine-needle aspiration (FNA). - CT Scan:
CT imaging offers detailed cross-sectional views of the pancreas, making it ideal for detecting tumors, pancreatitis complications, and planning surgical interventions. - MRI/MRCP:
MRI, and specifically MRCP (Magnetic Resonance Cholangiopancreatography), generates detailed images of the pancreatic and bile ducts, useful for diagnosing ductal obstructions and complex cystic lesions. - PET Scan:
PET scans assess the metabolic activity of pancreatic tissues, aiding in cancer diagnosis and staging.
Laboratory Tests
- Enzyme Levels:
Elevated serum amylase and lipase levels are indicative of acute pancreatitis. - Liver Function Tests:
These tests can help identify bile duct obstructions and related pancreatic issues. - Tumor Markers:
CA 19-9 and CEA levels can be elevated in pancreatic cancer, though they are not definitive on their own. - Hormonal Assays:
Measurements of insulin, glucagon, and other hormones are used when endocrine dysfunction is suspected.
Endoscopic and Invasive Procedures
- ERCP (Endoscopic Retrograde Cholangiopancreatography):
Combines endoscopy and fluoroscopy to visualize the pancreatic and bile ducts, allowing for both diagnosis and therapeutic interventions such as stent placement. - Laparoscopy:
Minimally invasive surgery that enables direct visualization of the pancreas and can facilitate biopsies or therapeutic procedures. - Biopsy and Histopathology:
Tissue samples obtained via FNA or surgical biopsy are examined microscopically to confirm malignancy or other pathological changes.
Advanced Molecular Techniques
- Genetic Testing:
For patients with a family history of pancreatic disease, genetic tests for mutations in BRCA1, BRCA2, PRSS1, SPINK1, and others can provide valuable risk assessment. - Molecular Profiling:
Next-generation sequencing (NGS) of pancreatic tumors helps identify specific mutations for targeted therapy and personalized treatment planning.
Treatment Options
Effective management of pancreatic conditions requires a personalized approach that may include medical therapies, lifestyle modifications, surgical interventions, and advanced treatment strategies.
Medical Therapies
Pain and Symptom Management
- Analgesics:
NSAIDs and acetaminophen are commonly used for mild to moderate pain. Opioids may be necessary for severe pain, particularly in chronic pancreatitis or advanced cancer. - Nerve Blocks:
Techniques like celiac plexus blocks can offer relief for refractory pain.
Pancreatic Enzyme Replacement Therapy (PERT)
- Purpose:
In patients with pancreatic insufficiency, PERT provides digestive enzymes to improve nutrient absorption and alleviate malabsorption symptoms. - Implementation:
Enzyme supplements are taken with meals to aid digestion.
Hormonal and Metabolic Control
- Insulin and Oral Hypoglycemics:
For patients with pancreatic diabetes, managing blood glucose is crucial. Insulin therapy is often required for type 1 diabetes, while oral medications are used in type 2 diabetes. - Dietary Management:
A low-fat, nutrient-dense diet helps reduce the workload on the pancreas and manage symptoms in conditions like chronic pancreatitis.
Surgical Interventions
Pancreatectomy Procedures
- Distal Pancreatectomy:
Removal of the body and tail of the pancreas is indicated for localized tumors or cysts in these regions. - Whipple Procedure (Pancreaticoduodenectomy):
A complex surgery that removes the head of the pancreas along with portions of the duodenum, bile duct, and sometimes the stomach. It is primarily used for pancreatic cancer located in the head of the pancreas. - Total Pancreatectomy:
Reserved for extensive disease, this procedure removes the entire pancreas, often accompanied by removal of surrounding tissues and subsequent hormone management.
Drainage and Decompression Surgeries
- Puestow Procedure (Lateral Pancreaticojejunostomy):
This surgery creates a drainage channel between the pancreatic duct and the jejunum to relieve ductal pressure in chronic pancreatitis. - Cyst Drainage:
Endoscopic, percutaneous, or surgical drainage of pancreatic pseudocysts is employed when cysts cause pain or complications.
Chemotherapy, Radiation, and Targeted Therapies
Chemotherapy
- Regimens:
Drugs like FOLFIRINOX (a combination of fluorouracil, leucovorin, irinotecan, and oxaliplatin) and gemcitabine (often with nab-paclitaxel) are used to treat pancreatic cancer, especially in advanced stages.
Radiation Therapy
- Techniques:
External Beam Radiation Therapy (EBRT) and Stereotactic Body Radiotherapy (SBRT) are used either as adjuvant treatment following surgery or for palliative care in advanced cancer.
Targeted Therapies and Immunotherapy
- PARP Inhibitors:
For patients with BRCA-mutated pancreatic cancer, PARP inhibitors such as olaparib offer targeted treatment options. - EGFR Inhibitors:
Erlotinib is sometimes used in combination with chemotherapy. - Immunotherapy:
Emerging treatments such as immune checkpoint inhibitors and cancer vaccines are under investigation for their potential to improve outcomes in pancreatic cancer.
Emerging and Experimental Treatments
- Precision Medicine:
Tailoring therapy based on the genetic profile of the tumor has the potential to significantly improve treatment efficacy. - Gene Therapy:
Experimental approaches are exploring the modification of genetic pathways in cancer cells to halt tumor progression. - Novel Immunotherapies:
These include adoptive cell therapies like CAR-T cells that are being studied for their ability to target and destroy pancreatic cancer cells.
Nutritional & Supplementary Support
Optimal pancreatic health relies heavily on proper nutrition and supplementation. A balanced diet rich in essential nutrients supports pancreatic function, helps reduce inflammation, and aids in the prevention and management of pancreatic disorders.
Essential Nutrients and Vitamins
- Omega-3 Fatty Acids:
Found in fish oil, flaxseed, and chia seeds, omega-3s possess anti-inflammatory properties that may help reduce the risk of pancreatitis and improve metabolic health. - Vitamin D:
Adequate vitamin D levels are linked to improved immune function and may reduce the risk of pancreatic cancer and other disorders. - B Vitamins:
Vitamins such as B6, B12, and folic acid are essential for cellular metabolism and energy production, contributing to the overall function of the pancreas. - Antioxidants (Vitamins C & E):
These protect pancreatic cells from oxidative damage, supporting tissue repair and reducing inflammation.
Herbal Supplements
- Turmeric (Curcumin):
Curcumin is renowned for its potent anti-inflammatory and antioxidant effects. Studies suggest it can protect pancreatic tissue and may reduce the risk of chronic pancreatitis and pancreatic cancer. - Milk Thistle (Silymarin):
Known for its liver-protective properties, milk thistle also supports the pancreas by reducing inflammation and promoting detoxification. - Ginseng:
An adaptogenic herb that helps balance hormones, reduce stress, and improve insulin sensitivity—key factors in maintaining pancreatic health.
Enzymes and Antioxidants
- Pancreatic Enzymes:
Supplementation with pancreatic enzymes (amylase, lipase, protease) can aid digestion in individuals with pancreatic insufficiency. - Alpha-Lipoic Acid:
This powerful antioxidant helps lower oxidative stress and improves glucose metabolism. - Coenzyme Q10 (CoQ10):
CoQ10 supports cellular energy production and shields pancreatic cells from oxidative damage.
Hormonal and Miscellaneous Supplements
- Melatonin:
Besides regulating sleep, melatonin exhibits antioxidant properties and may help protect pancreatic cells. - N-Acetylcysteine (NAC):
NAC supports detoxification and reduces oxidative stress, which is beneficial for overall pancreatic function.
Probiotics
- Role in Gut Health:
Probiotics help maintain a balanced gut microbiome, which indirectly supports the pancreas by promoting proper digestion and reducing systemic inflammation.
Lifestyle & Preventive Practices
A proactive lifestyle is crucial for maintaining pancreatic health and preventing disease. Integrating healthy habits can support both the digestive and endocrine functions of the pancreas.
- Adopt a Balanced Diet:
- Consume a nutrient-rich diet including fruits, vegetables, whole grains, lean proteins, and healthy fats.
- Limit intake of processed foods, sugars, and unhealthy fats that can strain the pancreas.
- Exercise Regularly:
- Engage in at least 150 minutes of moderate exercise per week to maintain a healthy weight and improve insulin sensitivity.
- Physical activity enhances circulation and overall metabolic health.
- Manage Stress Effectively:
- Incorporate stress-reduction techniques such as yoga, meditation, and deep breathing exercises into your daily routine.
- Chronic stress can negatively impact hormone levels and overall pancreatic function.
- Avoid Smoking and Limit Alcohol:
- Smoking and excessive alcohol consumption are major risk factors for pancreatitis and pancreatic cancer.
- Abstaining from these harmful substances is essential for protecting pancreatic cells.
- Stay Hydrated:
- Drink plenty of water to support cellular function and overall metabolic health.
- Proper hydration aids in digestion and the effective functioning of the pancreas.
- Regular Health Check-ups:
- Schedule routine visits with your healthcare provider for monitoring of pancreatic health, especially if you have risk factors.
- Early detection of any issues allows for prompt and effective management.
- Monitor Blood Sugar Levels:
- Keeping track of blood glucose can help identify early signs of pancreatic dysfunction or diabetes.
- Regular monitoring is particularly important if you have a family history of pancreatic or metabolic disorders.
- Limit Exposure to Environmental Toxins:
- Reduce exposure to harmful chemicals and endocrine disruptors that may adversely affect pancreatic function.
- Opt for natural, organic products when possible.
- Consider Supplementation:
- Discuss with your healthcare provider the possibility of taking supplements such as omega-3s, vitamin D, and antioxidants to support pancreatic health.
- Supplementation can help fill nutritional gaps and reduce oxidative stress.
- Maintain a Healthy Weight:
- Achieving and sustaining a healthy weight is crucial for optimal pancreatic function and overall metabolic balance.
- Weight management through diet and exercise reduces the risk of insulin resistance and other pancreatic disorders.
Trusted Resources
For further information on pancreatic health, consider these reliable resources that offer in-depth insights, research updates, and practical guidance.
Recommended Books
- “The End of Diabetes” by Joel Fuhrman, M.D.:
Provides insights into preventing and reversing diabetes through dietary and lifestyle changes, with implications for pancreatic health. - “The Blood Sugar Solution” by Mark Hyman, M.D.:
Offers a comprehensive guide to balancing blood sugar and preventing metabolic disorders through nutrition and lifestyle modifications. - “Pancreatic Cancer: A Patient and His Doctor Balance Hope and Truth” by Michael J. Lippe and Steven J. Pantilat, M.D.:
Provides a compassionate look at pancreatic cancer, offering insights into diagnosis, treatment, and patient care.
Academic Journals
- Pancreas Journal:
Publishes peer-reviewed articles on pancreatic diseases, including research on pancreatitis, pancreatic cancer, and diabetes. - Journal of Pancreatic Research:
Focuses on clinical and translational research related to pancreatic biology, pathology, and new treatment approaches.
Mobile Applications
- MySugr:
A diabetes management app that helps track blood sugar levels, diet, and exercise, indirectly supporting pancreatic health. - Diabetes: M:
Offers comprehensive tools for managing diabetes, including glucose tracking, meal planning, and activity logging. - Pancreas:
An informational app dedicated to pancreatic diseases, symptoms, treatment options, and management strategies, ideal for both patients and healthcare professionals.
Frequently Asked Questions
What are the primary functions of the pancreas?
The pancreas plays dual roles: its exocrine portion produces digestive enzymes and bicarbonate-rich fluid to aid in digestion, while its endocrine portion secretes hormones like insulin and glucagon to regulate blood glucose levels and maintain metabolic balance.
How does the pancreas aid in digestion?
The pancreas produces zymogens that are converted into active enzymes in the duodenum, breaking down carbohydrates, proteins, and fats. Ductal cells also secrete bicarbonate to neutralize stomach acid, ensuring an optimal environment for enzyme function.
What is the role of the islets of Langerhans?
The islets of Langerhans are clusters of endocrine cells that produce hormones such as insulin, glucagon, somatostatin, and pancreatic polypeptide. These hormones regulate blood sugar levels and support overall metabolic homeostasis.
What are common causes of pancreatitis?
Pancreatitis can be caused by gallstones, excessive alcohol consumption, certain medications, infections, or trauma. It presents as acute or chronic inflammation of the pancreas and can lead to complications like necrosis or systemic inflammation.
How can lifestyle changes support pancreatic health?
Maintaining a balanced diet, regular exercise, stress management, avoiding smoking and excessive alcohol, and staying hydrated are all crucial for protecting pancreatic cells and supporting overall pancreatic function.
Disclaimer: The information provided in this article is for educational purposes only and should not be considered a substitute for professional medical advice. Always consult with a qualified healthcare provider regarding any medical concerns.
If you found this article informative, please share it on Facebook, X (formerly Twitter), or your preferred social media platform. Your support helps spread valuable health insights and encourages others to maintain optimal pancreatic health.