The penis is a remarkable organ essential not only for reproductive functions but also for urination and sexual pleasure. This guide explores its intricate anatomy, vital roles in human physiology, common conditions that affect its health, and the latest treatment and wellness strategies. Whether you are seeking medical insight or practical health tips, this comprehensive resource provides evidence-based information to help you understand and maintain optimal penile health. With a blend of detailed anatomical descriptions, diagnostic techniques, and lifestyle recommendations, this guide is designed to empower readers with the knowledge necessary for informed decisions about sexual and overall well-being.
Table of Contents
- Penis Structural Composition and Anatomy
- Penis Functional Physiology and Roles
- Common Penile Disorders and Conditions
- Diagnostic Strategies for Penile Health
- Therapeutic and Treatment Modalities for Penis Issues
- Nutritional Support and Supplements for Penis Wellness
- Lifestyle and Preventative Measures for Penis Health
- Trusted Resources and Educational Tools
- Frequently Asked Questions
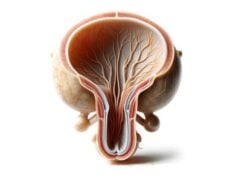
Penis Structural Composition and Anatomy
The penis boasts a complex architecture consisting of several distinct external and internal structures, each playing a crucial role in its overall function. Understanding its anatomy not only deepens our appreciation for its design but also aids in recognizing potential issues when they arise.
External Components
Shaft:
The shaft, or body, is the elongated cylindrical part of the penis. It is covered by skin and houses three essential columns of erectile tissue. Two of these, known as the corpora cavernosa, run along the dorsal (upper) side, while the corpus spongiosum occupies the ventral (underside) and contains the urethra.
- Corpora Cavernosa: These paired structures are the powerhouse of penile erection. Each column is encased in a tough, fibrous sheath called the tunica albuginea. During sexual arousal, the corpora cavernosa become engorged with blood, resulting in the rigidity required for penetration.
- Corpus Spongiosum and Glans: The single corpus spongiosum surrounds the urethra and extends distally to form the glans penis. The glans is the bulbous, highly sensitive tip that is abundant in nerve endings. In uncircumcised males, the glans is protected by the foreskin, a retractable fold of skin that not only covers but also helps retain moisture.
Foreskin (Prepuce):
In uncircumcised men, the foreskin serves as a natural cover for the glans, shielding it from environmental irritants and helping to preserve its sensitivity. However, in some cultures and medical scenarios, circumcision—the surgical removal of the foreskin—is performed for hygienic, religious, or health-related reasons.
Internal Architecture
Erectile Tissue:
At the heart of the penis’ function is its erectile tissue, which is pivotal for achieving and maintaining an erection.
- Tunica Albuginea: This dense, fibrous layer envelops the corpora cavernosa, acting as a containment barrier that traps blood during an erection. Its elasticity and strength are fundamental in maintaining rigidity.
- Urethra: Running through the corpus spongiosum, the urethra is a dual-purpose tube that transports both urine and semen. Its passage through the erectile tissue is critical for synchronizing the processes of urination and ejaculation.
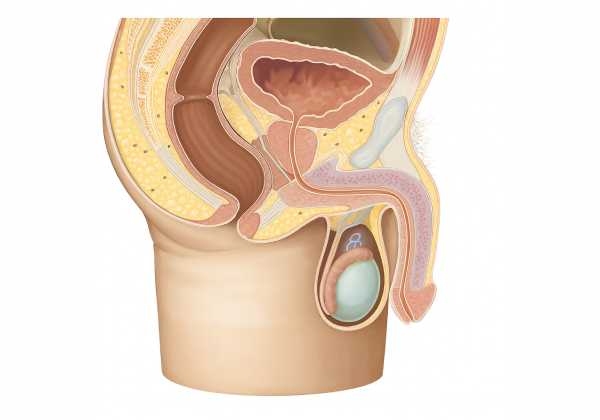
Vascular Network
A rich network of arteries and veins supplies the penis, ensuring that adequate blood flow is maintained for both resting and erect states.
Arterial Supply:
- Internal Pudendal Arteries: These are the primary suppliers of blood to the penis. Once they branch, they form several arteries:
- Dorsal Arteries: These run along the top surface, providing blood to the skin, glans, and urethra.
- Deep (Cavernous) Arteries: These penetrate deep into the corpora cavernosa, fueling the erectile tissues.
- Bulbourethral Arteries: Supplying the corpus spongiosum and bulb, these arteries are crucial for the proper functioning of the entire structure.
Venous Drainage:
- Deep Dorsal Vein: This vein collects deoxygenated blood from the erectile tissues and glans, eventually draining into the prostatic venous plexus.
- Superficial Dorsal Vein: This network drains the skin and subcutaneous tissues of the penis.
Innervation
The penis is richly supplied with nerves, ensuring both its sensory sensitivity and its ability to function during sexual arousal.
Sensory Innervation:
The dorsal nerve, a branch of the pudendal nerve, provides significant sensory input to the glans, shaft, and foreskin. This network of nerves conveys tactile sensations and plays an integral role in sexual pleasure.
Autonomic Innervation:
- Parasympathetic Fibers: These nerves initiate and sustain an erection by releasing nitric oxide, which dilates blood vessels and enhances blood flow.
- Sympathetic Fibers: In contrast, these fibers are involved in detumescence (the return to a flaccid state) by promoting vasoconstriction after sexual arousal.
Supporting Ligaments and Connective Tissues
Suspensory Ligaments:
These fibrous structures secure the penis to the pubic symphysis, providing stability during both flaccid and erect states. They ensure that the organ remains properly oriented during sexual activity.
Fundiform Ligament:
Originating from the linea alba, the fundiform ligament wraps around the base of the penis. It offers additional support, especially during vigorous physical activity or sexual intercourse.
Microscopic Features
On a microscopic level, the erectile tissue of the penis consists of a network of smooth muscle fibers, sinusoids (blood-filled spaces), and collagen fibers. The interplay between these components allows for rapid changes in blood volume, which is the foundation for the erection process. The cellular matrix, combined with the robust vascular and neural supplies, creates an environment optimized for both sexual function and tissue repair.
Penis Functional Physiology and Roles
The physiological functions of the penis extend well beyond its role in sexual reproduction. This organ is a multifunctional system that orchestrates complex processes like erection, ejaculation, and urination—all of which rely on a finely tuned interplay between neural, vascular, and muscular systems.
Erection Mechanism
Erection is a sophisticated physiological event that involves neural, vascular, and hormonal components. It is initiated by sexual arousal, whether triggered by visual, tactile, or psychological stimuli.
- Neural Activation:
Sexual arousal stimulates the central nervous system. Signals from the brain travel down the spinal cord and activate the parasympathetic nerves innervating the penis. These nerves release nitric oxide, a key chemical messenger. - Vasodilation:
Nitric oxide causes the smooth muscles in the walls of the penile arteries to relax, leading to vasodilation. This process significantly increases blood flow into the corpora cavernosa and corpus spongiosum. - Engorgement and Rigidity:
As blood floods the erectile tissues, the tunica albuginea traps the blood, leading to a sustained erection. The compressed veins restrict the outflow of blood, maintaining the rigidity necessary for sexual intercourse. - Detumescence:
After sexual stimulation subsides, the sympathetic nervous system is activated. This leads to vasoconstriction, reducing blood flow and allowing the penis to return to a flaccid state.
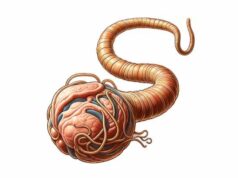
Ejaculation Process
Ejaculation is the culmination of a coordinated series of events involving both the emission and expulsion of semen.
- Emission Phase:
In this phase, secretions from the testes, seminal vesicles, prostate, and bulbourethral glands combine in the urethra. This process is predominantly controlled by sympathetic nervous impulses. - Expulsion Phase:
Following emission, rhythmic contractions of the pelvic floor muscles, including the bulbospongiosus and ischiocavernosus, propel the semen through the urethra and out of the body. This phase is typically experienced as a pleasurable climax and is accompanied by intense sensory feedback.
Urination Function
The penis also serves as the conduit for the excretion of urine from the bladder. Urination is a process that involves the coordinated actions of the bladder muscles and the urethral sphincters.
- Urethral Role:
The urethra, which runs through the corpus spongiosum, allows urine to pass from the bladder to the external environment. This dual-function channel must remain unobstructed and functional for both urination and ejaculation. - Sphincter Control:
Two sphincters—the internal (smooth muscle) and external (skeletal muscle)—regulate the flow of urine. Their coordinated action ensures that urination is a controlled process, maintaining continence until voluntary release occurs.
Sensory and Pleasure Functions
The high concentration of nerve endings in the glans and foreskin makes the penis exceptionally sensitive to tactile stimulation. This sensitivity not only enhances sexual pleasure but also triggers reflexes that are essential for initiating erection and ejaculation.
- Tactile Stimulation:
The myriad of sensory receptors located in the penile skin detect a range of stimuli from gentle touch to more intense pressure. This information is relayed to the brain, contributing to sexual arousal and satisfaction. - Reflex Arcs:
The reflexes involved in erection and ejaculation are designed for rapid response. For instance, the stimulation of the glans can trigger an immediate reflex arc that leads to the engorgement of erectile tissue.
Hormonal Influences
Hormones play an integral role in regulating the functions of the penis. Testosterone, in particular, is vital for the development, maintenance, and proper functioning of this organ. Adequate levels of testosterone not only support libido but also influence the vascular health necessary for achieving and sustaining an erection.
Integration of Functions
The diverse functions of the penis—erection, ejaculation, urination, and sensory perception—are interdependent. Successful sexual function relies on the seamless integration of neural signals, vascular changes, and muscular contractions. Any disruption in this finely tuned system, whether through hormonal imbalances, nerve damage, or vascular issues, can lead to dysfunction and impact overall sexual health.
In summary, the physiology of the penis is a marvel of biological engineering. Its ability to rapidly shift between states of arousal and rest, to combine functions essential for reproduction and excretion, and to provide profound sensory feedback underscores its critical role in both physical and emotional aspects of male health.
Common Penile Disorders and Conditions
The penis, like any organ, can be affected by a variety of disorders. These conditions may be congenital, acquired, infectious, traumatic, or even neoplastic in nature. Early diagnosis and appropriate treatment are essential for managing symptoms and preserving function.
Erectile Dysfunction (ED)
Overview:
Erectile dysfunction is defined as the persistent inability to achieve or maintain an erection sufficient for satisfactory sexual performance. ED can have both physical and psychological causes.
Potential Causes:
- Vascular Issues: Conditions such as atherosclerosis, hypertension, and diabetes can compromise blood flow.
- Neurological Factors: Disorders like multiple sclerosis or nerve injuries may impair the signals necessary for an erection.
- Hormonal Imbalances: Low testosterone levels or thyroid dysfunction can contribute to ED.
- Psychological Factors: Stress, anxiety, depression, and relationship problems may also play significant roles.
- Medications: Certain prescriptions, including antihypertensives and antidepressants, may induce ED as a side effect.
Clinical Manifestations:
- Difficulty initiating an erection.
- Trouble maintaining an erection during sexual activity.
- Reduced sexual desire or libido.
Peyronie’s Disease
Overview:
Peyronie’s disease is characterized by the development of fibrous plaques within the penile tissue, leading to abnormal curvature, pain during erection, and sometimes erectile dysfunction.
Etiology and Risk Factors:
- Trauma or Micro-Injury: Repeated injury or forceful bending of the penis may precipitate scar formation.
- Genetic Predisposition: A family history of connective tissue disorders, such as Dupuytren’s contracture, may increase risk.
- Inflammatory Processes: Chronic inflammation can promote the deposition of fibrous tissue.
Symptoms:
- Noticeable curvature or bending of the penis during erection.
- Painful erections or discomfort.
- Shortening of the penile length.
- Difficulty with sexual intercourse due to the curvature.
Priapism
Overview:
Priapism is defined as a prolonged, often painful erection that persists for hours beyond or without sexual stimulation. This condition is considered a medical emergency.
Common Causes:
- Hematologic Disorders: Sickle cell anemia and leukemia are well-known causes.
- Medication Side Effects: Certain medications used for erectile dysfunction, depression, or blood disorders may trigger priapism.
- Traumatic Injury: Direct trauma to the genital or spinal area can precipitate this condition.
- Substance Use: Recreational drugs, including cocaine and marijuana, have been implicated in priapism.
Clinical Presentation:
- An erection lasting longer than four hours.
- Pain and discomfort in the penile shaft.
- The glans may remain softer compared to the rigid shaft.
- Risk of permanent tissue damage if not treated promptly.
Phimosis and Paraphimosis
Phimosis:
This condition involves the inability of the foreskin to retract fully over the glans, which can lead to hygiene issues and discomfort.
- Causes: Congenital factors, recurrent infections, or inflammatory conditions such as balanitis.
- Symptoms: Difficulty in retracting the foreskin, pain during urination or sexual activity, and ballooning of the foreskin during micturition.
Paraphimosis:
A related but more urgent condition where the retracted foreskin cannot be returned to its original position, leading to swelling and compromised blood flow.
- Symptoms: Marked swelling of the glans and foreskin, pain, and, in severe cases, ischemia that can threaten tissue viability.
Penile Cancer
Overview:
Though rare, penile cancer is a serious condition that typically affects older men. It most often develops in the skin or underlying tissues of the penis.
Risk Factors:
- Human Papillomavirus (HPV) Infection: A significant risk factor.
- Chronic Inflammation: Conditions like phimosis, especially in uncircumcised men with poor hygiene.
- Smoking: Increases the risk of malignant transformation.
- Age: More common in men over the age of 50.
Clinical Indicators:
- Non-healing lesions or sores on the penile skin.
- Changes in skin color or texture.
- Presence of a lump or mass.
- Discharge or bleeding from the penis.
Balanitis
Overview:
Balanitis is the inflammation of the glans penis, often accompanied by inflammation of the foreskin (balanoposthitis). It is common in uncircumcised men and can be exacerbated by poor hygiene.
Causes:
- Infections: Bacterial, fungal, or viral pathogens.
- Allergic Reactions: Sensitivity to soaps, detergents, or latex.
- Irritation: Prolonged moisture or smegma accumulation can lead to irritation.
Symptoms:
- Redness, swelling, and tenderness of the glans.
- Itching or burning sensations.
- Discharge or foul odor.
- Difficulty retracting the foreskin in severe cases.
Penile Fracture
Overview:
A penile fracture is a rare but serious injury resulting from a rupture in the tunica albuginea during vigorous sexual activity or trauma.
Etiology:
- Traumatic Bending: Sudden, forceful bending of an erect penis.
- Accidental Injury: Falls or impact injuries during intercourse.
Clinical Features:
- A popping or cracking sound at the moment of injury.
- Immediate pain and loss of erection.
- Rapid onset of swelling, bruising, and hematoma formation.
- Potential long-term complications such as curvature or erectile dysfunction if not treated promptly.
Understanding these conditions and their causes is crucial for early detection, appropriate treatment, and the prevention of long-term complications. Each disorder presents unique challenges, and effective management typically involves a multidisciplinary approach.
Diagnostic Strategies for Penile Health
A precise diagnosis is the cornerstone of effective management of penile conditions. Medical practitioners employ a wide range of diagnostic tools and methods to assess the health of the penis, ranging from physical examinations to advanced imaging techniques.
Clinical Evaluation and History
The diagnostic process usually starts with a comprehensive clinical evaluation. Physicians take detailed patient histories, focusing on:
- The onset, duration, and progression of symptoms.
- Any previous injuries, surgeries, or infections.
- Lifestyle factors including smoking, alcohol use, and sexual habits.
- Family history and genetic predispositions.
A thorough physical examination follows, during which the penis is inspected for lesions, deformities, swelling, or discoloration. Palpation helps assess the presence of plaques, lumps, or tenderness that might indicate underlying conditions.
Laboratory Tests
Blood Tests:
Blood tests are essential to identify systemic issues that may affect penile health. These include:
- Complete Blood Count (CBC): To check for infections or hematologic conditions.
- Blood Glucose Levels: High levels may indicate diabetes, a common cause of erectile dysfunction.
- Hormonal Assays: Measuring testosterone, prolactin, and thyroid hormone levels to identify endocrine abnormalities.
Urine Analysis:
Urinalysis and culture tests help detect urinary tract infections or sexually transmitted infections (STIs) that could contribute to penile symptoms.
Imaging Modalities
Ultrasound Examination:
Ultrasound is a non-invasive, readily available imaging technique that is invaluable for assessing penile structure and vascular flow.
- Doppler Ultrasound: Evaluates blood flow in the penile arteries and veins, which is critical in diagnosing erectile dysfunction and priapism.
- High-Resolution Ultrasound: Can detect fibrous plaques in Peyronie’s disease or other structural anomalies.
Magnetic Resonance Imaging (MRI):
MRI provides high-resolution images of soft tissues, making it particularly useful for complex cases such as penile trauma or suspected cancer. MRI can delineate the extent of lesions and guide surgical planning when necessary.
Specialized Diagnostic Procedures
Penile Biopsy:
When suspicious lesions or cancers are detected, a small tissue sample may be obtained via biopsy for histopathological examination. This procedure confirms the presence of malignant cells and helps determine the appropriate treatment plan.
Cavernosography:
This imaging technique involves injecting a contrast dye into the corpora cavernosa followed by X-ray imaging. It is primarily used to assess venous leakage in cases of erectile dysfunction and to evaluate vascular integrity.
Nocturnal Penile Tumescence (NPT) Test:
The NPT test monitors erections during sleep to differentiate between physiological and psychological causes of erectile dysfunction. A device worn overnight records erection frequency, duration, and rigidity.
Urethroscopy:
A thin, flexible camera is inserted into the urethra to directly visualize the urethral lining and detect strictures, blockages, or lesions that might contribute to urinary or sexual dysfunction.
Genetic and Psychological Evaluations
Genetic Testing:
For congenital anomalies such as hypospadias or epispadias, genetic tests can identify mutations or markers that influence penile development.
Psychological Assessment:
In cases where psychological factors may contribute to erectile dysfunction, a structured evaluation by a mental health professional can identify stress, anxiety, or depression that may be impairing sexual function.
By integrating these diagnostic strategies, clinicians can formulate a comprehensive view of penile health, ensuring that both physical and psychological factors are addressed. Early and accurate diagnosis is crucial for implementing effective treatment regimens and preventing further complications.
Therapeutic and Treatment Modalities for Penis Issues
Managing penile conditions requires a multifaceted treatment approach tailored to the specific disorder, its severity, and the patient’s overall health. Treatment strategies may include lifestyle modifications, medications, devices, minimally invasive procedures, and surgical interventions.
Treatment of Erectile Dysfunction
Lifestyle Modifications:
- Exercise: Regular aerobic and resistance training improves cardiovascular health and enhances blood flow.
- Diet: A balanced diet rich in fruits, vegetables, lean proteins, and whole grains supports vascular health.
- Smoking Cessation and Alcohol Moderation: Avoiding smoking and excessive alcohol consumption improves circulation and erectile function.
Medications:
- Phosphodiesterase Type 5 Inhibitors (PDE5 Inhibitors): Drugs such as sildenafil, tadalafil, and vardenafil work by relaxing smooth muscle tissue and increasing blood flow to the penis.
- Hormone Therapy: For men with low testosterone, hormone replacement can restore normal sexual function.
- Alprostadil: Available as an injection or urethral suppository, this medication promotes vasodilation and aids in achieving an erection.
Mechanical Devices:
- Vacuum Erection Devices (VEDs): These devices create a vacuum around the penis, drawing blood into the erectile tissues and facilitating an erection.
- Penile Implants: In severe cases, surgically implanted devices provide a long-term solution by allowing men to control the timing and rigidity of an erection.
Psychotherapy:
For cases where psychological factors contribute to erectile dysfunction, counseling and therapy can be invaluable. Techniques such as cognitive behavioral therapy (CBT) may alleviate performance anxiety and stress.
Management of Peyronie’s Disease
Pharmacological Approaches:
- Collagenase Injections (Xiaflex): This FDA-approved treatment helps break down the collagen plaques that cause curvature.
- Verapamil and Interferon Injections: These may reduce plaque size and penile curvature over time.
Non-Surgical Treatments:
- Shockwave Therapy: Low-intensity extracorporeal shockwave therapy (Li-ESWT) can promote blood flow and help remodel fibrous tissue.
- Traction Devices: Penile traction therapy may gradually reduce curvature by stretching the fibrous plaque.
Surgical Interventions:
- Plication Surgery: This procedure involves placing sutures on the longer side of the penis to counteract curvature.
- Plaque Incision and Grafting: In severe cases, the plaque is surgically incised and a graft is used to restore normal shape.
- Penile Prosthesis: For men with coexisting erectile dysfunction and severe curvature, implant surgery can provide both structural correction and functional restoration.
Approaches for Priapism
Acute Management:
- Medications: Alpha-adrenergic agonists like phenylephrine are injected to constrict blood vessels and reduce blood flow.
- Aspiration and Irrigation: Blood may be drawn from the corpora cavernosa and the area irrigated with saline to restore normal circulation.
- Surgical Shunting: In refractory cases, creating a shunt to redirect blood flow may be necessary to prevent permanent tissue damage.
Treatment for Phimosis and Paraphimosis
Non-Surgical Treatments:
- Topical Steroids: Application of corticosteroid creams can reduce inflammation and facilitate foreskin retraction in phimosis.
- Manual Reduction: In cases of paraphimosis, gentle manual manipulation may relieve the constriction.
Surgical Options:
- Circumcision: Complete removal of the foreskin is often the definitive treatment for recurrent phimosis or paraphimosis.
- Preputioplasty: A less invasive surgery that widens the foreskin without full removal.
Management of Penile Cancer
Surgical Treatments:
- Wide Local Excision: Removal of the tumor with a margin of healthy tissue.
- Partial or Total Penectomy: Depending on the extent of the cancer, removal of part or all of the penis may be necessary.
- Lymph Node Dissection: If metastasis is suspected, surrounding lymph nodes are also removed.
Adjunct Therapies:
- Radiation Therapy: Used to treat localized tumors or as an adjunct to surgery.
- Chemotherapy: Indicated in advanced or metastatic penile cancer, aimed at controlling disease progression.
Addressing Balanitis and Penile Fracture
Balanitis Treatment:
- Topical Antifungals or Antibiotics: Based on the underlying cause, these medications help alleviate infection.
- Improved Hygiene: Regular cleaning under the foreskin can prevent recurrence.
Penile Fracture Management:
- Immediate Surgical Repair: Timely surgical intervention is crucial to repair the tunica albuginea and prevent long-term complications.
- Postoperative Rehabilitation: Physical therapy and careful monitoring aid in restoring function and reducing scarring.
Each treatment modality is tailored to the individual’s condition and health status, with the overarching goal of restoring function, reducing pain, and enhancing quality of life.
Nutritional Support and Supplements for Penis Wellness
Proper nutrition and targeted supplementation play a vital role in maintaining penile health by enhancing blood flow, reducing inflammation, and supporting hormonal balance. Dietary interventions complement medical therapies and can contribute significantly to improved sexual function.
Essential Nutrients and Vitamins
L-Arginine:
An amino acid that acts as a precursor for nitric oxide, L-arginine is crucial for vasodilation and blood flow. Supplementation can help improve erectile function in men with mild to moderate dysfunction.
Zinc:
Zinc is essential for testosterone production and overall sexual health. Deficiency in zinc can lead to diminished libido and erectile difficulties, making supplementation beneficial for maintaining optimal levels.
Vitamin D:
Vitamin D supports vascular health and hormonal balance. Low levels of vitamin D have been linked to erectile dysfunction, and supplementation may help improve both vascular and sexual health.
Herbal and Natural Supplements
Ginseng:
Long celebrated for its aphrodisiac properties, ginseng can boost energy levels, improve blood flow, and enhance sexual performance. Studies have shown that ginseng may also support overall vitality.
Maca Root:
Traditionally used to enhance libido and stamina, maca root is believed to improve sexual desire and performance. Its adaptogenic properties help reduce stress and boost energy.
Yohimbine:
Derived from the bark of an African tree, yohimbine may improve blood flow to the penis by stimulating nerve impulses. It is often used to treat mild cases of erectile dysfunction, although it must be used cautiously due to potential side effects.
Enzymatic and Antioxidant Support
Bromelain:
An enzyme found in pineapples, bromelain is known for its anti-inflammatory properties. It can help reduce inflammation in penile tissues, thereby supporting erectile function and recovery from injury.
Coenzyme Q10 (CoQ10):
CoQ10 is a powerful antioxidant that supports cellular energy production and cardiovascular health. Improved energy metabolism in penile tissues can lead to better erectile performance.
Pycnogenol:
Extracted from pine bark, pycnogenol enhances nitric oxide production and improves blood flow. This antioxidant has shown promise in clinical studies for improving erectile function.
Hormonal Support
Dehydroepiandrosterone (DHEA):
A natural hormone that serves as a precursor to testosterone, DHEA supplementation may help improve libido and erectile function, particularly in men with low levels of this hormone.
Integrating these nutrients and supplements into a daily regimen, alongside a balanced diet rich in fruits, vegetables, lean proteins, and whole grains, can have a synergistic effect on penile health. Regular monitoring of nutrient levels and consultation with healthcare providers ensures that supplementation is both safe and effective.
Lifestyle and Preventative Measures for Penis Health
Beyond medical treatments and supplements, everyday lifestyle choices are fundamental to maintaining the health and functionality of the penis. Preventative measures help reduce the risk of developing disorders and promote overall sexual well-being.
Dietary Habits and Physical Activity
- Nutritious Diet:
Eating a balanced diet that emphasizes fruits, vegetables, whole grains, and lean proteins provides essential vitamins and antioxidants that support vascular and hormonal health. - Regular Exercise:
Aerobic and resistance training improve cardiovascular health and circulation, which are vital for achieving and maintaining erections. Exercise also aids in weight management and stress reduction.
Hygiene and Safe Practices
- Proper Genital Hygiene:
Regular cleaning, especially for uncircumcised men, is critical to prevent infections such as balanitis. Maintaining good hygiene reduces the risk of inflammation and other complications. - Safe Sexual Practices:
Using protection during sexual activity minimizes the risk of sexually transmitted infections (STIs) that can adversely affect penile health.
Avoidance of Harmful Substances
- Smoking Cessation:
Smoking adversely affects blood flow and has been linked to erectile dysfunction. Quitting smoking can lead to improved vascular health. - Alcohol Moderation:
Excessive alcohol consumption can impair sexual function and disrupt hormonal balance. Moderation is key to preserving penile health.
Stress Management and Mental Well-Being
Chronic stress can impair sexual function and contribute to disorders such as erectile dysfunction. Techniques such as meditation, yoga, deep breathing exercises, and mindfulness help manage stress levels, ultimately supporting both mental and sexual health.
Regular Medical Check-Ups
- Routine Health Screenings:
Regular visits to healthcare providers facilitate early detection of conditions like diabetes, hypertension, or hormonal imbalances that could impact penile function. - Self-Examination:
Periodic self-examination helps in early detection of abnormalities such as lesions or unusual changes, ensuring prompt medical intervention.
Weight Management and Hydration
Maintaining a healthy weight reduces the risk of conditions such as diabetes and cardiovascular disease, both of which can impair penile function. Additionally, proper hydration supports overall cellular health and optimal blood flow.
By adopting these lifestyle changes and preventative strategies, individuals can significantly enhance their sexual health and reduce the likelihood of developing penile disorders.
Trusted Resources and Educational Tools
Staying informed and connected with reliable sources is essential for both patients and healthcare providers. Access to high-quality information and support resources empowers individuals to make informed decisions regarding penile health.
Recommended Books
- “The Penis Book: A Doctor’s Complete Guide to the Penis” by Aaron Spitz, M.D.:
This book provides a comprehensive overview of penile anatomy, common disorders, and treatment options, offering valuable insights for both patients and clinicians. - “Male Sexual Health: A Couple’s Guide” by Felice Dunas:
A practical resource for couples, this book explores both physical and emotional aspects of male sexual health, with strategies to enhance intimacy and address common concerns. - “The New Naked: The Ultimate Sex Education for Grown-Ups” by Harry Fisch, M.D.:
Focusing on modern sexual education, this book offers evidence-based advice on improving sexual performance and maintaining overall penile health.
Scholarly Journals
- The Journal of Sexual Medicine:
This peer-reviewed journal publishes cutting-edge research on sexual function, treatment strategies, and the latest advancements in the field of male sexual health. - Urology:
Covering all aspects of urology, this journal provides in-depth studies on penile conditions, surgical techniques, and innovative therapies.
Mobile Applications
- MyFitnessPal:
A comprehensive nutrition and fitness tracker that helps users maintain a balanced diet and exercise regimen, which is essential for vascular and overall health. - Headspace:
This mindfulness and meditation app offers stress-reduction techniques that support mental well-being and, indirectly, sexual health. - Health Mate by Withings:
An app that tracks various health metrics such as weight, activity levels, and cardiovascular health, enabling users to monitor factors that influence penile function.
These trusted resources provide valuable information, support, and tools for those looking to maintain or improve their penile health. Regularly consulting these materials and staying updated with the latest research can empower individuals to take proactive steps in managing their sexual well-being.
Frequently Asked Questions on the Penis
What are the primary functions of the penis?
The penis is essential for sexual reproduction, urination, and providing sensory pleasure. It enables the delivery of sperm during intercourse, facilitates the excretion of urine, and contains a high concentration of nerve endings, contributing to sexual sensation.
How does an erection occur?
An erection is triggered by sexual arousal, which activates parasympathetic nerves. This leads to the release of nitric oxide, causing vasodilation and increased blood flow into the erectile tissues. The trapped blood creates rigidity necessary for sexual activity.
What causes erectile dysfunction?
Erectile dysfunction can be caused by vascular problems, neurological disorders, hormonal imbalances, psychological issues, or as a side effect of certain medications. Lifestyle factors such as smoking and poor diet may also contribute.
How is Peyronie’s disease treated?
Peyronie’s disease is treated through a combination of medication, such as collagenase injections, non-surgical methods like shockwave therapy and traction, or surgical interventions to correct curvature and restore function.
Can penile conditions be prevented?
Preventative measures include maintaining a healthy diet, regular exercise, good genital hygiene, avoiding smoking and excessive alcohol, managing stress, and regular medical check-ups to monitor overall health.
Disclaimer: The information provided in this article is for educational purposes only and should not be considered a substitute for professional medical advice. Always consult a healthcare provider for any concerns regarding your health.
Please share this article on Facebook, X (formerly Twitter), or your preferred social media platform to help spread awareness about penile health and the latest treatment strategies.