What is persistent fetal vasculature?
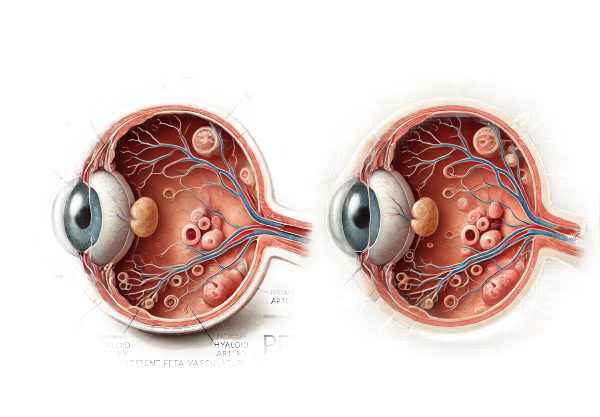
Persistent fetal vasculature (PFV), also known as persistent hyperplastic primary vitreous (PHPV), is a congenital ocular abnormality caused by the failure of the fetal hyaloid vascular system to regress. This system, which includes the hyaloid artery, primary vitreous, and tunica vasculosa lentis, usually undergoes involution in the late stages of fetal life. When this regression does not occur properly, remnants of the vasculature remain in the eye, causing a variety of structural abnormalities and potential vision problems.
Pathophysiology
During normal fetal development, the hyaloid artery delivers blood to the developing lens. Around the third trimester, this artery and its associated structures regress and disappear, allowing the secondary vitreous to develop. In PFV, this regression is either incomplete or absent, resulting in the persistence of these structures, which can disrupt normal eye development and function.
PFV can be classified as anterior, posterior, or a combination of the two, depending on the location and extent of the persistent vasculature.
Anterior PFV: This form primarily affects the front part of the eye, specifically the lens and ciliary body. It can cause cataracts, shallow anterior chambers, elongated ciliary processes, and secondary glaucoma. The presence of fibrovascular tissue may cause traction on the lens and other anterior structures.
Posterior PFV: This form affects the back of the eye, which includes the vitreous, retina, and optic disc. It can cause retinal detachment, vitreous hemorrhage, and optic nerve abnormalities. Posterior PFV is frequently associated with more severe visual impairment than the anterior form.
Combined PFV: In many cases, both the anterior and posterior segments are involved, resulting in a combination of the complications listed above.
Causes and Risk Factors
Although the exact cause of PFV is unknown, it is thought to be caused by a disruption in the fetal vasculature’s normal involution process. While PFV is usually sporadic, there are several risk factors and associations to consider.
Genetic Factors: Although most cases are sporadic, there have been reports of PFV being associated with genetic syndromes or familial occurrences, indicating a possible genetic component.
Premature Birth: Infants born prematurely are more likely to have developmental anomalies such as PFV. Incomplete development at birth may contribute to the persistence of fetal vasculature.
Other Congenital Anomalies: PFV may coexist with other congenital conditions, including trisomy 13, Walker-Warburg syndrome, and Norrie disease. These associations point to a broader developmental disturbance that affects the ocular structures.
Symptoms
The symptoms and clinical presentation of PFV can vary greatly depending on the severity and scope of the condition. Common indications and symptoms include:
Leukocoria: One of the most visible symptoms of PFV is leukocoria, a white pupillary reflex. This happens when there is a cataract or fibrovascular membrane in the visual axis.
Microphthalmia: Affected eyes are typically smaller than normal (microphthalmic), which can be a distinguishing clinical feature. The persistent fetal vasculature disrupted development, resulting in this size reduction.
Strabismus: Children with PFV frequently experience eye misalignment, also known as strabismus. This can be the result of abnormal visual development and poor visual acuity in the affected eye.
Nystagmus: Involuntary, rhythmic eye movements, or nystagmus, may be present, especially if the condition has severely impaired vision from a young age.
Vision Impairment: The degree of visual impairment varies. In mild cases, vision may be relatively preserved, whereas severe cases can result in significant vision loss or blindness. The degree of visual impairment is largely determined by the structures involved and the effectiveness of any treatments used.
Impact on Vision
The impact of PFV on vision is significant, and it varies depending on whether the condition is unilateral (affecting one eye) or bilateral. In unilateral cases, the unaffected eye usually develops normally, but the child may still have difficulty with depth perception and binocular vision. Bilateral cases are more difficult because both eyes are impaired, which can result in severe visual impairment or blindness.
Psychological and Social Implications
Living with PFV can have a significant psychological and social impact, particularly on children. Visible abnormalities such as leukocoria and strabismus can have an impact on self-esteem and social relationships. Vision impairment can have an impact on learning and development, making it difficult for children to keep up academically and socially. Early intervention and support are critical for assisting children and families in dealing with the challenges posed by PFV.
Complications
If left untreated, PFV can cause a number of serious complications, including:
Glaucoma: Increased intraocular pressure due to structural abnormalities can cause secondary glaucoma, which, if left untreated, can cause further damage to the optic nerve and result in vision loss.
Retinal Detachment: The traction exerted by the persistent fibrovascular tissue can cause the retina to detach, resulting in severe vision impairment or blindness if not treated promptly.
Cataracts: The presence of persistent vasculature frequently results in cataract formation, which obscures the visual axis and contributes to leukocoria and vision loss.
Vitreous Hemorrhage: Bleeding into the vitreous can occur due to abnormal blood vessels, resulting in sudden vision loss and requiring immediate medical attention.
Amblyopia: Also known as lazy eye, amblyopia can occur in the affected eye as a result of inadequate visual input during the critical period of visual development. If not treated promptly, this can cause permanent vision impairment.
Diagnostic Approaches for Persistent Fetal Vasculature
PFV is diagnosed using a combination of clinical examination, imaging techniques, and, in some cases, genetic testing to confirm the presence and extent of the condition and distinguish it from other ocular pathologies. Here are the main diagnostic methods used:
Clinical Examination
Ophthalmic Examination: The initial step in diagnosing PFV is to conduct a thorough ophthalmic examination. This includes evaluating visual acuity, examining the anterior segment with a slit lamp, and performing a dilated fundus examination to see the posterior segment structures.
Indirect Ophthalmoscopy: This technique provides a thorough examination of the retina and optic disc. It aids in determining the presence of persistent hyaloid arteries, fibrovascular membranes, and other posterior segment abnormalities.
Imaging Techniques
Ultrasound Biomicroscopy (UBM): UBM is an excellent imaging tool for examining anterior segment structures. It aids in detecting abnormalities such as persistent tunica vasculosa lentis, elongated ciliary processes, and cataracts.
B-Scan Ultrasound: B-scan ultrasonography generates cross-sectional images of the eye, allowing for the detection of vitreous and retinal abnormalities. It is especially useful when the media is opaque, such as in dense cataracts or vitreous hemorrhage.
Magnetic Resonance Imaging (MRI): MRI can generate detailed images of the intraocular and orbital structures. It is useful for determining the extent of persistent vasculature and any associated anomalies in the brain and orbit.
Fluorescein Angiography: This imaging technique involves injecting a fluorescent dye into the bloodstream and taking a series of photographs to reveal the retinal blood vessels. It aids in assessing abnormal blood vessels and detecting areas of leakage or neovascularization.
Genetic Testing
Molecular Genetic Testing: If PFV is suspected to be part of a genetic syndrome or there is a family history of similar conditions, genetic testing can be performed. This aids in identifying specific genetic mutations associated with PFV and can provide useful information for genetic counseling.
Differential Diagnosis
Retinoblastoma: One of the most important conditions to distinguish from PFV is retinoblastoma, a malignant tumor of the retina that can also cause leukocoria. Imaging and clinical characteristics aid in distinguishing the two conditions.
Coats Disease: This condition causes abnormal blood vessel development in the retina and can present with symptoms similar to PFV. Fluorescein angiography and clinical examination aid in the differentiation process.
Retinal Detachment: Tractional retinal detachments caused by PFV must be distinguished from other types of retinal detachment. Imaging tests such as B-scan ultrasound and MRI are useful in making this distinction.
Persistent Fetal Vasculature Treatment
The goal of treating Persistent Fetal Vasculature (PFV) is to address structural abnormalities and avoid complications that could impair vision. The treatment approach varies depending on the severity of the condition, the specific ocular structures involved, and the patient’s overall health. Here are the primary treatments for PFV:
Surgical Intervention
Lensectomy: In cases where the lens has been significantly affected by cataract or there is significant fibrovascular tissue causing traction, surgical removal of the lens (lensectomy) may be required. This procedure helps to clear the visual axis, lowering the risk of amblyopia.
Vitrectomy: A vitrectomy is a surgical procedure that removes persistent vitreous and fibrovascular tissue, particularly in the posterior PFV. This surgery can relieve retinal traction, treat vitreous hemorrhage, and prevent or repair retinal detachment. The vitreous gel and any abnormal tissue are removed, followed by the introduction of a saline solution or gas bubble to keep the eye in shape.
Membranectomy: In cases of severe fibrovascular proliferation, a membranectomy may be required to remove the abnormal tissue. This reduces traction on the retina and other structures, which preserves or improves vision.
Glaucoma Surgery: If secondary glaucoma develops as a result of increased intraocular pressure, surgical intervention to treat it may be required. Trabeculectomy and the placement of glaucoma drainage devices can help control intraocular pressure and protect the optic nerve.
Non-surgical Management
Observation: In mild cases of PFV, where structural anomalies do not cause significant visual impairment or complications, careful observation may be the preferred method. Regular monitoring ensures that any progression of the condition is addressed promptly.
Correction of Refractive Errors: Children with PFV frequently develop refractive errors due to structural abnormalities in the eye. Prescription glasses or contact lenses can help correct these errors by increasing visual acuity and lowering the risk of amblyopia.
Visual Rehabilitation
Amblyopia Treatment: If amblyopia occurs, early intervention is critical. Patching the unaffected eye to encourage use of the affected eye is one treatment option, as is using atropine drops in the stronger eye to temporarily blur its vision. These treatments help to strengthen the weaker eye and enhance overall visual function.
Low Vision Aids: For patients with severe visual impairment, low vision aids such as magnifying glasses, telescopic lenses, and other assistive devices can improve visual abilities and quality of life.
Supportive Care
Parental Education: Educating parents about PFV, its potential complications, and the importance of attending treatment and follow-up appointments is critical. Parents play an important role in the successful treatment of the condition.
Psychological Support: Treating the psychological impact of PFV on both the patient and their family is critical. Counseling and support groups can assist families in dealing with the emotional and social challenges presented by the condition.
Frequently Asked Questions About Persistent Fetal Vascularity
What causes persistent fetal vascularity?
Persistent Fetal Vasculature (PFV) develops when the fetal hyaloid vascular system, which normally regresses during late fetal development, does not disappear. The exact cause is unknown, but it is believed to be the result of disruptions in normal developmental processes. The majority of cases are sporadic, but some may be linked to genetics or congenital syndrome.
How Is PFV Diagnosed?
PFV is diagnosed using a combination of clinical examination, imaging techniques, and genetic testing. Ophthalmologists use techniques such as ultrasound biomicroscopy, B-scan ultrasound, and MRI to visualize the eye’s structures and identify persistent vasculature. A detailed patient history and a thorough ophthalmic examination are also required for a correct diagnosis.
Does PFV affect both eyes?
Yes, PFV can affect either or both eyes. Unilateral PFV is more common, but bilateral cases do occur and can pose more significant challenges in terms of visual development and treatment.
Is surgery always necessary for PFV?
Not all PFV cases require surgery. The severity of the condition and the presence of complications such as cataracts, retinal detachment, or significant fibrovascular tissue causing traction determine the need for surgical intervention. Mild cases can be treated with careful observation and non-surgical procedures.
What are the possible complications of PFV?
PFV complications include secondary glaucoma, retinal detachment, cataracts, vitreous hemorrhage, and amblyopia. Early detection and appropriate treatment are critical for managing these complications and maintaining vision.
How Does PFV Affect Vision?
The effect of PFV on vision varies according to its severity and the specific structures involved. In mild cases, vision may be unaffected, whereas severe cases can cause significant visual impairment or blindness. Early intervention and appropriate management are critical for improving visual outcomes.
Is PFV preventable?
PFV is a congenital condition caused by developmental anomalies, so there is currently no known way to prevent it. Early detection and treatment are critical for managing the condition and preventing complications.
What role do parents have in managing PFV?
Parents play an important role in managing PFV by ensuring that their child follows treatment plans, attends regular follow-up appointments, and uses prescribed visual aids or corrective lenses. Parental education and support are critical for the successful management of the condition.
Are there any support groups for families affected by PFV?
Yes, several organizations and support groups offer resources and assistance to families dealing with PFV and other congenital eye conditions. These groups provide useful information, emotional support, and practical advice.
Can children with PFV live normal lives?
Many children with PFV can live normal, fulfilling lives if diagnosed early, treated appropriately, and managed on an ongoing basis. Visual rehabilitation and supportive care can help them overcome obstacles and realize their full potential.
Trusted Resources and Support
Books and Organizations
Books:
- “Pediatric Ophthalmology: Current Thought and A Practical Guide”* by Edward M. Wilson and Richard Saunders.
- “Clinical Ophthalmology: A Systematic Approach” by Jack J. Kanski and Brad Bowling.
Organizations:
- The American Association for Pediatric Ophthalmology and Strabismus (AAPOS): Offers resources and support to families dealing with pediatric eye conditions, including PFV.
- The National Eye Institute (NEI) provides comprehensive information on eye health and congenital eye conditions.
- The Vision of Children Foundation: funds research and offers resources to families affected by genetic and congenital vision disorders.
Financial Aid Options
Insurance Coverage: Most health insurance policies cover the diagnosis and treatment of PFV. It is critical to consult with your insurance provider to determine the specifics of your coverage, such as co-pays and deductibles.
Patient Assistance Programs: Pharmaceutical companies and non-profit organizations may provide patient assistance programs to help with the cost of medications and treatment. Programs such as RxAssist provide information about available resources.
Non-Profit Organizations: Organizations like the HealthWell Foundation and the Patient Advocate Foundation help patients pay for medical expenses, including treatments for congenital conditions like PFV.
Government Programs: Medicaid and the Children’s Health Insurance Program (CHIP) offer coverage to low-income families. These programs can help cover the costs of PFV treatment and care, ensuring that children receive the medical attention they require regardless of their family’s financial situation.






