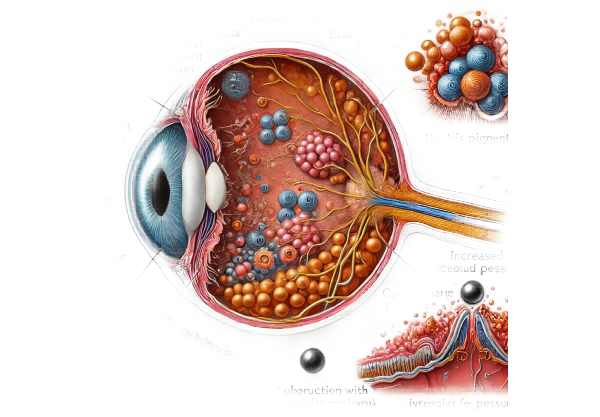
What is pigmentary glaucoma?
Pigmentary glaucoma is a type of secondary open-angle glaucoma caused by pigment granules dispersed throughout the eye. These granules, which normally reside in the iris, escape into the aqueous humor and can clog the trabecular meshwork. This blockage prevents the outflow of aqueous humor, resulting in increased intraocular pressure (IOP) and subsequent optic nerve damage. Pigmentary glaucoma is frequently associated with pigment dispersion syndrome (PDS).
Pathophysiology
The pathophysiology of pigmentary glaucoma begins with the dispersion of pigment granules from the iris pigment epithelium. The causes of this dispersion are unknown, but it is believed to be due to mechanical friction between the posterior iris surface and the zonular fibers that hold the lens in place. Activities that cause the iris to move more, such as exercise or pupil dilation, frequently exacerbate this friction.
Once dispersed, the aqueous humor transports the pigment granules to the trabecular meshwork, where they accumulate and obstruct outflow pathways. The accumulation of these granules increases the resistance to aqueous outflow, resulting in elevated IOP. Over time, high IOP damages the optic nerve, causing the characteristic glaucomatous optic neuropathy and visual field loss associated with pigmentary glaucoma.
Epidemiology
Pigmentary glaucoma primarily affects young people, between the ages of 20 and 50. It is more common in men than in women, with a ratio of roughly 2:1. This condition is more common among people of European descent. The prevalence of pigmentary glaucoma among people with pigment dispersion syndrome varies, with estimates ranging from 10% to 50%.
Risk Factors
Several factors raise the risk of developing pigmentary glaucoma, including:
Genetic Predisposition: Evidence suggests a hereditary component, as pigment dispersion syndrome and pigmentary glaucoma can run in families. Specific genetic mutations linked to this condition are being investigated.
Myopia (Nearsightedness): People with moderate to high myopia have a higher risk of developing pigmentary glaucoma. The exact mechanism is unknown, but it is thought that the anatomical configuration in myopic eyes may contribute to increased iris-zonule contact.
Sex: Males are more commonly affected than females, possibly due to differences in iris anatomy and hormonal influences.
Age: Pigmentary glaucoma usually appears in early to middle adulthood, as opposed to other types of glaucoma that are more common in older people.
Symptoms
Pigmentary glaucoma can be asymptomatic in its early stages, which is why at-risk individuals should have regular eye exams. As the disease progresses, symptoms may include:
Blurred Vision: Patients may experience episodes of blurred vision, especially after physical exertion or activities requiring significant pupil dilation.
Halos Around Lights: Halos, or rainbow-colored rings, can form around lights, particularly in low-light conditions.
Eye Pain: Some people experience intermittent eye pain or discomfort, which is frequently associated with high IOP.
Peripheral Vision Loss: Glaucoma causes gradual loss of peripheral vision. This symptom may go unnoticed until major vision loss occurs.
Frequent Changes in Eyeglass Prescriptions: Sudden changes in prescription strength may indicate fluctuating IOP and advancing glaucoma.
Impact on Vision
Pigmentary glaucoma can have a significant impact on vision if not detected and treated promptly. The condition primarily affects peripheral vision, and patients may not notice vision loss until it interferes with their central vision. Glaucoma-related visual field loss follows a distinct pattern, beginning in the peripheral field and progressing inward.
The rate of progression can vary greatly between individuals. Some people deteriorate quickly, while others progress more slowly. Without treatment, pigmentary glaucoma can cause significant visual impairment and, eventually, blindness.
Psychological and Social Implications
Living with pigmentary glaucoma can have a significant psychological and social impact. The fear of progressive vision loss and blindness can cause anxiety and depression. The condition can also affect daily activities such as driving, work, and social interactions, resulting in a lower quality of life.
Patients with pigmentary glaucoma may need to make lifestyle changes to deal with their condition. These modifications may include avoiding activities that aggravate symptoms, such as high-impact sports or activities that require extended periods of pupil dilation.
Complications
If left untreated, pigmentary glaucoma can cause a number of serious complications:
Chronic Angle-Closure Glaucoma: As IOP rises over time, the angle between the iris and cornea narrows or closes, resulting in angle-closure glaucoma.
Optic Nerve Damage: Prolonged pressure on the optic nerve can cause permanent nerve damage and irreversible vision loss.
Blindness: Severe and untreated pigmentary glaucoma can lead to complete blindness.
Prognosis
The prognosis for people with pigmentary glaucoma varies depending on when the condition is diagnosed and how well it is managed. Early detection and consistent treatment can reduce IOP and slow the progression of optic nerve damage. With proper management, many patients can maintain useful vision for the rest of their lives.
Regular ophthalmologist visits, adherence to treatment regimens, and lifestyle changes are critical for managing this condition and preserving vision. Medical and surgical advances are improving the prognosis for people suffering from pigmentary glaucoma.
Techniques to Diagnose Pigmentary Glaucoma
An ophthalmologist conducts a thorough evaluation to diagnose pigmentary glaucoma, which includes a detailed patient history, clinical examination, and specialized diagnostic tests. Here are the main diagnostic methods used:
Patient History
Detailed History: A complete patient history is required to identify risk factors such as a family history of glaucoma, myopia, and previous episodes of elevated IOP or ocular trauma. Understanding the patient’s symptoms and any vision changes can provide valuable diagnostic information.
Symptom Evaluation: Patients may report blurred vision, halos around lights, eye pain, or changes in peripheral vision. Documenting these symptoms aids in connecting clinical findings to patient experiences.
Clinical Examination
Visual Acuity Test: Measuring visual acuity helps determine the effect of pigmentary glaucoma on central vision. This test determines how well a person sees at various distances.
Slit Lamp Examination: A slit lamp examination allows an ophthalmologist to thoroughly examine the eye’s anterior segment. Pigment granules on the corneal endothelium (Krukenberg spindle), the anterior lens capsule, and the trabecular meshwork are common findings in pigmentary glaucoma cases.
Gonioscopy: Gonioscopy is an essential diagnostic tool for determining the drainage angle of the eye. It aids in detecting pigment accumulation in the trabecular meshwork and determining the anterior chamber angle configuration. This examination is necessary to distinguish between open-angle and angle-closure glaucoma.
Intraocular Pressure Measurement: Measuring intraocular pressure is critical for diagnosing and managing glaucoma. Elevated IOP is a significant risk factor for optic nerve damage. Tonometry is one of the techniques used to measure IOP.
Specialized Tests
Optic Nerve Head Examination: A thorough examination of the optic nerve head with ophthalmoscopy or fundus photography is required. The optic nerve may exhibit glaucomatous damage, such as increased cupping, thinning of the neuroretinal rim, and notching.
Visual Field Testing: Automated perimetry is used to detect visual field defects. Patients with pigmentary glaucoma frequently exhibit distinct patterns of peripheral vision loss, which aids in the diagnosis and monitoring of disease progression.
Optical Coherence Tomography (OCT): OCT can produce high-resolution cross-sectional images of the retina and optic nerve head. It measures the thickness of the retinal nerve fiber layer (RNFL) and the ganglion cell complex (GCC), which can indicate early glaucoma damage.
Ultrasound Biomicroscopy (UBM): UBM is an advanced imaging technique that allows for high-resolution visualization of anterior segment structures. It aids in determining the configuration of the iris, ciliary body, and angle structures, providing important information for diagnosing and treating pigmentary glaucoma.
Differential Diagnosis
Primary Open-Angle Glaucoma: Differentiating pigmentary glaucoma from primary open-angle glaucoma (POAG) is critical because both conditions have open angles and high IOP. The presence of pigment dispersion and specific clinical signs, such as the Krukenberg spindle, aid in the diagnosis of pigmentary glaucoma.
Pseudoexfoliation Syndrome: This condition causes an accumulation of abnormal fibrillary material in the anterior segment, which leads to secondary glaucoma. Gonioscopy and slit lamp examination can distinguish pseudoexfoliation syndrome from pigmentary glaucoma.
Angle-Closure Glaucoma: Gonioscopy can distinguish between angle-closure glaucoma, which has a narrow or closed anterior chamber angle, and pigmentary glaucoma, which has an open angle and pigment dispersion.
Pigmentary Glaucoma Treatment
The treatment for pigmentary glaucoma focuses on lowering intraocular pressure (IOP) to prevent further optic nerve damage and preserve vision. The management strategy is usually a combination of medications, laser treatments, and surgical interventions tailored to the specific needs of the patient.
Medications
Topical medications:
- Prostaglandin Analogs: These are the first-line treatment for lowering intraocular pressure (IOP). They promote the outflow of aqueous humor via the uveoscleral pathway. Common agents include latanoprost, bimatoprost, and travoprost.
- Beta Blockers: These medications reduce aqueous humor production, lowering IOP. Timolol and betaxolol are common medications.
- Alpha Agonists: These decrease aqueous humor production while increasing uveoscleral outflow. Examples include brimonidine and apraclonidine.
- Carbonic Anhydrase Inhibitors: These reduce aqueous humor production. They come in two forms: topical (dorzolamide, brinzolamide) and oral (acetazolamide, methazolamide).
- Rho Kinase Inhibitors: A newer type of medication that lowers IOP by increasing aqueous outflow via the trabecular meshwork. Netarsudil is an example.
Oral medications:
- When topical medications fail, oral carbonic anhydrase inhibitors such as acetazolamide can be used to reduce IOP in the short term.
Laser Treatments
Laser Trabeculoplasty:*
- Argon Laser Trabeculoplasty (ALT): This procedure employs laser energy to improve aqueous outflow via the trabecular meshwork.
- Selective Laser Trabeculoplasty (SLT): SLT uses a lower energy laser to target specific cells within the trabecular meshwork, lowering IOP while causing fewer side effects than ALT. It is repeatable if necessary.
Laser Iridotomy:*
- Laser iridotomy, while uncommon in pigmentary glaucoma, may be considered if there is evidence of pupillary block or if the patient has narrow-angle glaucoma.
Surgical Interventions
Trabeculectomy:
- This is a surgical procedure that involves creating a small flap in the sclera to allow aqueous humor to drain out of the eye without passing through the trabecular meshwork. It is usually reserved for situations in which medical and laser treatments have failed to control IOP.
Glaucoma Drainage Devices :
- Implants like the Ahmed, Baerveldt, and Molteno valves can help with aqueous humor drainage. These devices are frequently considered when trabeculectomy fails or is not feasible.
** Minimally Invasive Glaucoma Surgery (MIGS):**
- MIGS procedures, such as the iStent and Hydrus microstent, offer a safer alternative to traditional surgeries. They are less invasive and can coexist with cataract surgery.
Cataract surgery:
- In patients with significant cataracts and pigmentary glaucoma, cataract surgery alone can help lower IOP by deepening the anterior chamber and reducing pigment dispersion.
Lifestyle & Monitoring
Regular monitoring:
- Patients with pigmentary glaucoma require regular check-ups to monitor their IOP, optic nerve health, and visual fields. These visits allow us to adjust treatment plans as needed to maintain optimal IOP control.
Lifestyle modifications:
- Patients should avoid activities that exacerbate pigment dispersion, such as strenuous exercise or frequent pupil dilation. Protective eyewear can help reduce trauma to the eye, which can result in pigment release.
Psychological Support
Living with pigmentary glaucoma can be difficult because of the risk of vision loss and the need for continuous treatment. Psychological support, such as counseling and support groups, can help patients deal with the emotional and social consequences of their condition.
Frequently Asked Questions About Pigmentary Glaucoma
What is Pigmentary Glaucoma?
Pigmentary glaucoma is a form of secondary open-angle glaucoma in which pigment granules from the iris clog the trabecular meshwork, raising intraocular pressure and causing optic nerve damage.
How Is Pigmentary Glaucoma Diagnosed?
A comprehensive eye examination is required for diagnosis, which includes visual acuity tests, slit lamp examination, gonioscopy, intraocular pressure measurement, optic nerve head examination, visual field testing, and optical coherence tomography (OCT).
What are the signs of pigmentary glaucoma?
Symptoms may include blurred vision, halos around lights, eye pain, peripheral vision loss, and frequent changes in eyeglass prescriptions. Early stages may be asymptomatic.
Is it possible to cure pigmentary glaucoma?
There is no cure for pigmentary glaucoma, but it can be effectively managed with medications, laser treatments, and surgeries to reduce intraocular pressure and prevent vision loss.
Is pigmentary glaucoma hereditary?
The fact that pigment dispersion syndrome and pigmentary glaucoma can run in families suggests a genetic predisposition. Specific genetic mutations are under investigation.
How can lifestyle changes help manage pigmentary glaucoma?
Avoiding activities that cause significant pupil dilation, wearing protective eyewear, and following prescribed treatments and eye exams are critical for managing the condition.
Is there any new treatment for pigmentary glaucoma?
Research is ongoing, and new treatments, such as advanced medications and minimally invasive glaucoma surgeries (MIGS), are emerging, providing more ways to manage the condition.
How frequently should I visit my eye doctor if I have pigmentary glaucoma?
Regular follow-up visits, usually every 3-6 months, are essential for monitoring intraocular pressure, optic nerve health, and visual fields, allowing for timely adjustments to the treatment plan.
Can pigmentary glaucoma cause blindness?
If left untreated, pigmentary glaucoma can cause significant vision loss and even blindness. Early detection and consistent treatment are critical for preserving vision.
Are there any support groups for people with pigmentary glaucoma?
Yes, support groups and organizations offer resources, information, and emotional support to people with pigmentary glaucoma and their families. Connecting with others who are facing similar challenges can be beneficial.
Trusted Resources and Support
Books and Organizations
Books:
- “Glaucoma: A Patient’s Guide to the Disease”* by Graham E. Trope.
- “The Glaucoma Book: A Practical, Evidence-Based Approach to Diagnosis and Treatment”* by Paul N. Schacknow and John R. Samples.
Organizations:
- American Academy of Ophthalmology (AAO): Provides extensive resources on ocular conditions, including pigmentary glaucoma, for patients and healthcare professionals.
- The Glaucoma Research Foundation (GRF) provides information, support, and funding for glaucoma research.
- National Eye Institute (NEI): An extensive source of information on eye health and related conditions, including pigmentary glaucoma.
Financial Aid Options
Insurance Coverage: Most health insurance policies cover the diagnosis and treatment of glaucoma and related conditions. Patients should consult with their insurance companies to understand the specifics of their coverage, such as co-pays and deductibles.
Patient Assistance Programs: Pharmaceutical companies and non-profit organizations frequently provide patient assistance programs to help with the cost of medications and treatments. Programs such as RxAssist provide information about available resources.
Non-Profit Organizations: Organizations like the HealthWell Foundation and the Patient Advocate Foundation help patients pay for medical expenses, including treatments for pigmentary glaucoma.
Government Programs: Medicaid, Medicare, and the Children’s Health Insurance Program (CHIP) provide coverage to eligible individuals. These programs can help cover the costs of treating and caring for pigmentary glaucoma, ensuring that patients receive the medical care they require regardless of their financial situation.