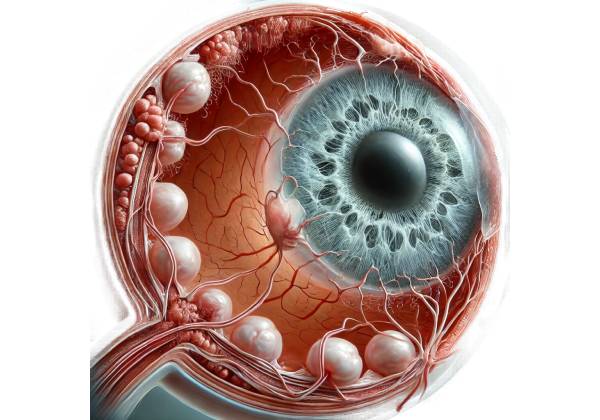
Proliferative vitreoretinopathy (PVR) is a complex and serious ocular condition that typically develops as a result of retinal detachment surgery. Membranes form on both the retina’s surfaces and within the vitreous cavity, resulting in retinal traction, distortion, and redetachment. PVR is the most common cause of failure in retinal detachment repair surgeries, with a significant impact on patient prognosis and visual outcomes.
Pathophysiology
PVR pathophysiology consists of a series of cellular and molecular events precipitated by retinal detachment and subsequent surgical intervention. The process starts with the release of RPE cells, glial cells, and macrophages into the vitreous cavity. These cells multiply, migrate, and differentiate, resulting in fibrous membranes on the retinal surface and within the vitreous body.
Several growth factors and cytokines play important roles in the development of PVR. Key among these are:
- Transforming Growth Factor-beta (TGF-β): TGF-β is a powerful fibrogenic cytokine that converts RPE cells into myofibroblasts, which aid in membrane formation and contraction.
- Platelet-Derived Growth Factor (PDGF): PDGF promotes the proliferation and migration of RPE cells and fibroblasts, which helps to form fibrous membranes.
- Vascular Endothelial Growth Factor (VEGF): VEGF promotes angiogenesis and increases vascular permeability, which contributes to the inflammatory environment in PVR.
- Fibroblast Growth Factor (FGF): FGF stimulates the proliferation of fibroblasts and other membrane-forming cells.
The formation of epiretinal membranes exerts tractional forces on the retina, resulting in distortion and possible redetachment. Furthermore, the contraction of these membranes can produce tangential forces, complicating the clinical picture.
Epidemiology
PVR is a significant concern in the management of retinal detachment, accounting for 5-10% of all cases. Some predisposing factors, such as:
- Extent and Duration of Retinal Detachment: The longer the retina is detached, the greater the risk of PVR from prolonged exposure to the vitreous cavity environment.
- Multiple Surgeries: Patients who have multiple retinal surgeries are more likely to develop PVR, as each surgical intervention can cause additional cellular responses.
- Trauma: Traumatic retinal detachments are more likely to cause PVR due to the extensive cellular disruption and inflammation that accompany ocular injuries.
- Vitreous Hemorrhage: The presence of blood in the vitreous cavity can exacerbate the inflammatory environment, increasing the risk of PVR development.
Clinical Presentation
The clinical presentation of PVR varies depending on the severity and scope of the condition. Patients may have a variety of symptoms, including:
- Decreased Visual Acuity: One of the most common symptoms of PVR is a gradual or sudden loss of visual acuity due to retinal distortion, traction, or redetachment.
- Metamorphopsia: Tractional forces on the retina can cause patients to experience distorted or wavy vision.
- Floaters: The presence of cells and membranes in the vitreous cavity can cause patients to see floaters, which are small, dark shapes or spots that move across the visual field.
- Photopsia: The tractional effects on the retina may cause patients to experience flashes of light, known as photopsia.
- Redetachment of the Retina: In severe cases, PVR can cause recurrent retinal detachment, which presents with symptoms similar to the initial detachment, such as sudden vision loss and a shadow or curtain across the visual field.
Differential Diagnosis
Diagnosing PVR requires distinguishing it from other ocular conditions that may present with similar symptoms. Differential diagnosis includes:
- Macular Pucker (Epiretinal Membrane): Both conditions result in the formation of membranes on the retinal surface. However, macular pucker is characterized by milder symptoms and does not involve the extensive traction and redetachment seen in PVR.
- Vitreous Hemorrhage: The presence of blood in the vitreous cavity can result in floaters and decreased vision. However, vitreous hemorrhage alone does not explain the retinal traction and distortion associated with PVR.
- Retinal Vein Occlusion: Retinal vein occlusions can result in sudden vision loss and retinal hemorrhages. However, it lacks membrane formation and tractional forces found in PVR.
- Diabetic Retinopathy: Advanced diabetic retinopathy can cause proliferative changes and tractional retinal detachment. However, the underlying cause and associated systemic signs distinguish it from PVR.
Complications
PVR can cause a number of serious complications that impact the visual prognosis and overall ocular health:
- Recurrent Retinal Detachment: The most serious complication of PVR is recurrent retinal detachment, which can occur even after multiple surgical procedures.
- Retinal Atrophy: Chronic traction and redetachment can cause retinal atrophy, which leads to permanent vision loss.
- Macular Involvement: PVR can spread to the macula, the central part of the retina responsible for sharp vision, affecting both visual acuity and quality of life.
- Anterior PVR: In some cases, PVR can affect the anterior segment of the eye, resulting in secondary complications like glaucoma and corneal decompensation.
Prognosis
The prognosis for patients with PVR varies according to the severity of the condition, the success of surgical interventions, and the degree of retinal involvement. Despite advances in surgical techniques, the recurrence rate of retinal detachment in PVR is still high, and visual outcomes are frequently poor. Early detection and intervention are critical for a better prognosis and preserving as much vision as possible.
Understanding PVR is critical for developing effective management strategies and improving patient outcomes in this challenging condition. Ongoing research into molecular mechanisms and potential therapeutic targets shows promise for future advances in PVR treatment.
Diagnostic methods
Proliferative vitreoretinopathy (PVR) is diagnosed through a combination of clinical examination, imaging studies, and specialized tests that determine the extent of membrane formation, retinal traction, and potential retinal detachment. Early and accurate diagnosis is critical for developing appropriate treatment strategies and improving visual outcomes.
Clinical Examination
The first step in diagnosing PVR is a comprehensive clinical examination by an ophthalmologist. The key components of the clinical assessment are:
- Visual Acuity Testing: Measuring visual acuity determines the extent of vision loss and serves as a baseline for monitoring disease progression and treatment response.
- Slit-Lamp Biomicroscopy: This examination provides detailed visualization of the anterior segment of the eye, the vitreous cavity, and the retinal surface. It aids in the diagnosis of inflammation, vitreous opacities, and membrane formation.
- Indirect Ophthalmoscopy: Indirect ophthalmoscopy provides a broad view of the retina, allowing for the detection of retinal tears, detachment, and the extent of membrane formation.
Imaging Studies
Imaging studies are critical for assessing the structural changes in the retina and vitreous cavity associated with PVR.
- Optical Coherence Tomography (OCT): OCT generates high-resolution cross-sectional images of the retina, allowing for detailed assessment of retinal layers, epiretinal membranes, and macular involvement. It is especially effective at detecting subtle changes and tracking disease progression.
- B-Scan Ultrasonography: B-scan ultrasonography is used to image the posterior segment of the eye, particularly in cases where media opacities prevent direct visualization. It aids in the evaluation of vitreous membranes, retinal detachment, and associated complications.
- Fundus Photography: Fundus photography takes detailed images of the retina and optic disc, allowing for documentation and comparison over time. It aids in monitoring the progression of PVR and the efficacy of treatment.
Specialized Tests
Additional tests to further evaluate and support the diagnosis of PVR:
- Fluorescein Angiography: This imaging technique involves injecting a fluorescent dye into the bloodstream and taking a series of photographs of the retina. It aids in determining retinal blood flow, identifying areas of leakage, and detecting retinal tears or breaks.
- Electroretinography (ERG): ERG assesses retinal cells’ electrical responses to light stimuli. It provides information on retinal function and aids in distinguishing PVR from other retinal conditions that exhibit similar symptoms.
Additional Diagnostic Techniques
In some cases, additional diagnostic techniques may be used to get a more comprehensive understanding of the extent and nature of PVR.
- Optical Coherence Tomography Angiography (OCTA): OCTA is a non-invasive imaging technique for obtaining detailed images of the retinal and choroidal vasculature. It aids in determining the extent of retinal ischemia and neovascularization that may be associated with PVR.
- Intraoperative Optical Coherence Tomography (iOCT): During retinal surgery, iOCT can generate real-time cross-sectional images of the retina. This enables the surgeon to dynamically visualize the status of the membranes and retina, allowing for more precise surgical decisions.
- Magnetic Resonance Imaging (MRI): While not commonly used for primary diagnosis, MRI can be useful in cases where there is a suspicion of an underlying systemic condition or extensive ocular trauma associated with PVR.
Proliferative Vitreoretinopathy Treatment
Proliferative vitreoretinopathy (PVR) is a complex condition that frequently necessitates a combination of medical, surgical, and supportive treatments. The main goals of treatment are to remove epiretinal membranes, reattach the retina, and prevent recurrence. Here, we look at the available methods for effectively managing PVR.
Surgical Interventions
Surgery is the cornerstone of PVR treatment, particularly in cases of retinal detachment or significant membrane formation. The main surgical procedures are:
- Vitrectomy: This is the most common surgical procedure for PVR. The vitreous gel, epiretinal membranes, and subretinal fluid are all removed during this procedure. Vitrectomy allows the surgeon to directly address the traction points and reattach the retina. Advanced vitrectomy techniques, such as the use of small-gauge instruments and intraoperative OCT, improve the accuracy and safety of the procedure.
- Membrane Peeling: During vitrectomy, surgeons frequently use membrane peeling to remove the fibrous tissues that cause retinal traction. This delicate procedure necessitates skill and precision to avoid damaging the underlying retina.
- Scleral Buckling: Scleral buckling is the process of placing a silicone band around the sclera (the white part of the eye) to indent the eye wall. This method helps to relieve vitreoretinal traction and promotes retinal reattachment. It is occasionally used in conjunction with vitrectomy in more complex cases.
- Retinectomy: In severe cases where the retina is heavily contracted or scarred, a retinectomy may be required. This procedure involves surgically removing a portion of the retina to relieve traction and allow for retinal reattachment.
Adjuvant Treatments
Adjuvant therapies are commonly used to improve surgical outcomes and reduce the risk of PVR recurrence.
- Intravitreal Injections: Anti-VEGF agents, corticosteroids, and anti-proliferative drugs can be administered directly into the vitreous cavity to reduce inflammation and inhibit fibrocellular proliferation.
- Tamponade Agents: Following vitrectomy, tamponade agents such as silicone oil or gas (e.g., sulfur hexafluoride or perfluoropropane) are used to keep the retina in place against the eye wall, encouraging reattachment and healing.
Medical Management
While surgery is the primary treatment for PVR, medical management helps control inflammation and prevent recurrence:
- Corticosteroids: Systemic or periocular corticosteroids can reduce inflammation and modulate the immune response, lowering the risk of membrane formation.
- Anti-inflammatory Agents: Nonsteroidal anti-inflammatory drugs (NSAIDs) can be used to reduce inflammation and alleviate symptoms.
- Antibiotics: Prophylactic antibiotics may be used to prevent infections caused by surgical procedures or other conditions, such as endophthalmitis.
Post-operative Care and Monitoring
Postoperative care is critical for ensuring successful outcomes and detecting any signs of recurrence early on.
- Regular Follow-Up: Frequent follow-up appointments are required to monitor the healing process, assess retinal attachment, and detect any early signs of complications or recurrence.
- Visual Rehabilitation: Visual rehabilitation services, such as low vision aids and therapy, can help patients maximize their remaining vision and improve their quality of life.
- Patient Education: Educating patients on the importance of following follow-up schedules, recognizing symptoms of retinal detachment, and maintaining overall eye health is critical for long-term success.
Experimental and Emerging Therapies
Research into new treatments for PVR is ongoing, with several promising approaches under consideration:
- Gene Therapy: Experimental gene therapies seek to correct the underlying genetic factors that contribute to PVR, paving the way for more targeted and effective treatments.
- Cell-Based Therapies: Stem cell therapies and other cell-based approaches are under investigation to promote retinal repair and regeneration.
- New Drug Delivery Systems: Advances in drug delivery, such as sustained-release implants and nanoparticles, aim to enhance the efficacy and safety of intraocular medications.
Finally, treating proliferative vitreoretinopathy necessitates a multifaceted approach that includes surgical intervention, adjuvant therapies, medical management, and meticulous postoperative care. Advances in surgical techniques and emerging therapies show promise for improving outcomes and preserving vision in this difficult condition.
Trusted Resources and Support
Books
- “Retinal Detachment: Principles and Practice” by A. L. Vitale and T. L. Terry: This book provides an in-depth look at the principles and surgical techniques for managing retinal detachment and associated complications like PVR.
- “Proliferative Vitreoretinopathy: Mechanisms, Diagnosis, and Treatment” by S. Machemer and R. A. Laqua: A comprehensive resource covering the mechanisms, clinical presentation, and management strategies for PVR.
Organizations
- American Academy of Ophthalmology (AAO): The AAO provides extensive resources, guidelines, and continuing education for ophthalmologists and patients dealing with retinal conditions, including PVR. AAO Website
- Retina International: This global organization supports research and provides information on retinal diseases, including PVR, offering resources for patients and healthcare professionals. Retina International Website
- National Eye Institute (NEI): Part of the National Institutes of Health, the NEI conducts and supports research on eye diseases and provides valuable educational resources on PVR and other retinal conditions. NEI Website






