Purtscher’s retinopathy is a rare but serious condition affecting the retina, the light-sensitive layer in the back of the eye. It is defined by sudden vision loss following trauma, particularly head or chest injuries, but it can also be associated with non-traumatic conditions such as acute pancreatitis, childbirth, and renal failure. Otmar Purtscher, an Austrian ophthalmologist, first described the condition in 1910 after seeing retinal findings in patients who had suffered head trauma.
Cotton wool spots, retinal hemorrhages, and Purtscher flecken—distinctive areas of retinal whitening that are often located around the optic nerve—are the hallmark signs of Purtscher’s retinopathy. These signs indicate microvascular occlusions and ischemia in the retinal arterioles. Patients frequently report symptoms such as sudden blurred vision, partial or complete vision loss, and visual field defects.
A thorough clinical examination, often supplemented by imaging techniques such as fundus photography, fluorescein angiography, and optical coherence tomography (OCT), is required to diagnose Purtscher’s retinopathy. These tools aid in determining the extent of retinal damage and distinguish Purtscher’s retinopathy from other retinal vascular diseases. Early diagnosis and treatment are critical for preventing permanent vision loss and addressing any underlying systemic conditions that contribute to the disease.
Standard Treatments for Purtscher’s Retinopathy
To preserve vision, Purtscher’s retinopathy management and treatment primarily focus on addressing the underlying cause and mitigating retinal damage. Given its relationship to systemic conditions and trauma, a multidisciplinary approach involving ophthalmologists, trauma surgeons, internists, and other specialists is frequently required.
Initial Management
The initial management of Purtscher’s retinopathy entails stabilizing the patient, particularly in cases of trauma or acute medical conditions. Key steps include:
- Systemic Stabilization: For patients with trauma-induced Purtscher’s retinopathy, the top priority is to treat life-threatening injuries and stabilize vital signs. Similarly, in non-traumatic cases, treating the underlying condition, such as acute pancreatitis or renal failure, is critical.
- Ophthalmic Evaluation: As soon as the patient is stable, he or she should have a thorough eye examination. Visual acuity tests, slit lamp examinations, and dilated fundus examinations are used to determine the extent of retinal damage.
Medical Treatment
There is no specific treatment for Purtscher’s retinopathy, so management focuses on providing supportive care and addressing the underlying cause. Nonetheless, several therapeutic strategies have been investigated to improve outcomes:
- Corticosteroids: The anti-inflammatory properties of systemic corticosteroids make them useful. Although the evidence is limited, some studies indicate that high-dose corticosteroids may reduce retinal inflammation and improve visual outcomes. Corticosteroids are usually given intravenously or orally, depending on the severity of the condition.
- Antiplatelet and anticoagulant therapy: These treatments aim to prevent further microvascular occlusions in the retina. Some cases have used aspirin and other antiplatelet agents, but their efficacy is unknown. Anticoagulants are more controversial and are typically reserved for specific indications based on the patient’s overall health and risk factors.
Monitoring and Supportive Care
Regular follow-up is required for patients with Purtscher’s retinopathy in order to monitor their visual function and detect any changes early. Supportive care can include:
- Visual Rehabilitation: Patients with severe vision loss can benefit from visual aids such as magnifiers, specialized lighting, and adaptive technologies to improve their remaining vision and quality of life.
- Patient Education: Teaching patients about their condition, the importance of follow-up visits, and lifestyle changes can help them manage their disease more effectively. For example, patients should be advised to avoid activities that could worsen their condition or cause additional trauma.
Latest Innovations in Purtscher’s Retinopathy Treatment
Recent advances in medical research and technology have created new opportunities for the treatment of Purtscher’s retinopathy. These innovations aim to improve diagnostic accuracy, therapeutic outcomes, and patient support for this difficult condition.
Advanced Imaging Techniques
Modern imaging technologies have greatly improved the detection and monitoring of Purtscher’s retinopathy. These tools provide detailed visualizations of retinal structures and aid in the detection of subtle changes that traditional examination methods may miss.
- Optical Coherence Tomography (OCT): OCT is a non-invasive imaging technique for obtaining high-resolution cross-sectional images of the retina. It allows for a thorough examination of the retinal layers, detecting abnormalities like microvascular occlusions and retinal edema. Enhanced-depth imaging OCT (EDI-OCT) can also see deeper structures such as the choroid, providing a more complete picture of retinal health.
- Fluorescein Angiography: This imaging technique involves injecting a fluorescent dye into the bloodstream and capturing images of the dye as it circulates through the retinal vessels. Fluorescein angiography can detect areas of retinal ischemia, microaneurysms, and vascular leakage that are typical of Purtscher’s retinopathy.
- Optical Coherence Tomography Angiography (OCTA): OCTA is an advanced type of OCT that visualizes blood flow within the retinal and choroidal vessels without the use of dye injection. It generates detailed maps of retinal perfusion, making it easier to detect microvascular abnormalities and track disease progression.
Novel Pharmacological Therapies
Emerging pharmacological treatments are being investigated to address the underlying causes of Purtscher’s retinopathy and improve visual outcomes.
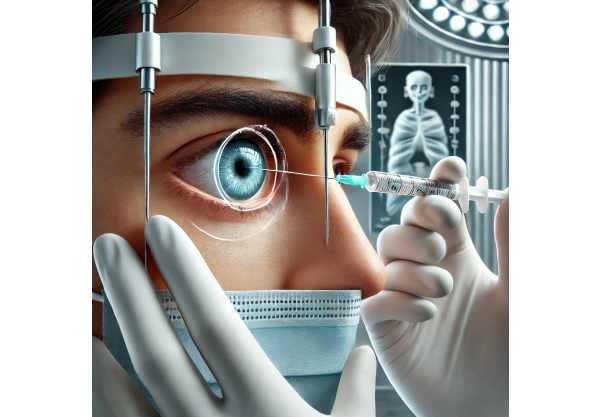
- Anti-VEGF Therapy: Anti-vascular endothelial growth factor (anti-VEGF) agents, which are commonly used to treat age-related macular degeneration and diabetic retinopathy, are being studied for their efficacy in treating Purtscher’s retinopathy. These drugs prevent abnormal blood vessel growth and decrease vascular permeability, potentially stabilizing retinal conditions and improving vision.
- Neuroprotective Agents: Neuroprotective drugs work to protect retinal ganglion cells and other neural structures from ischemia and inflammation. Citicoline and brimonidine are two compounds being studied for their ability to preserve visual function in retinal diseases such as Purtscher’s retinopathy.
Gene Therapy & Regenerative Medicine
Gene therapy and regenerative medicine innovations show promise for treating retinal diseases by addressing the underlying causes and promoting tissue repair.
- Gene Editing Technologies: Gene editing techniques such as CRISPR-Cas9 have the potential to correct genetic mutations and restore normal function in retinal cells. Although still in the experimental stage, these technologies may one day provide a cure for hereditary retinal diseases that predispose people to conditions such as Purtscher’s retinopathy.
- Stem Cell Therapy: Stem cell therapy attempts to regenerate damaged retinal tissues by introducing healthy, functional cells into the eye. Stem cell-based treatments for retinal diseases are currently being developed, and preliminary results show that they have the potential to restore vision in conditions characterized by retinal cell loss and damage.
Personalized Medical Approaches
Personalized medicine entails tailoring treatments to the unique characteristics of each patient, such as their genetic profile, disease characteristics, and overall health.
- Genetic Profiling: Genetic testing can identify people who are at risk for developing retinal diseases and help guide personalized treatment plans. Understanding the genetic causes of Purtscher’s retinopathy can aid in developing targeted therapies and preventive measures.
- Biomarker Analysis: Biomarkers are quantitative indicators of disease activity and treatment efficacy. Advances in biomarker research are allowing the identification of specific molecules linked to retinal inflammation and ischemia, which can be used to track disease progression and guide treatment.
Innovative Surgical Techniques
Surgical advancements are improving the outcomes of procedures used to treat complications caused by Purtscher’s retinopathy.
- Minimally Invasive Vitreoretinal Surgery: As surgical instruments and techniques have advanced, vitreoretinal surgery has become less invasive and more precise. Small-gauge vitrectomy, for example, enables the removal of vitreous hemorrhage and traction with minimal eye trauma, resulting in faster recovery and better visual outcomes.
- Retinal Prosthetics: Retinal prosthetics, such as the Argus II Retinal Prosthesis System, provide hope to patients suffering from severe vision loss due to retinal diseases. These devices stimulate the remaining retinal cells to produce visual input, potentially restoring partial vision in patients with severe vision loss.






