Punctate Inner Choroidopathy (PIC) is a rare inflammatory eye condition that affects mostly young, myopic (nearsighted) women. These small, yellow-white lesions in the inner choroid can cause significant visual disturbances if not treated. The choroid is a vascular layer of the eye that supplies oxygen and nutrients to the retina; inflammation in this area can cause damage to the overlying retina, resulting in vision loss.
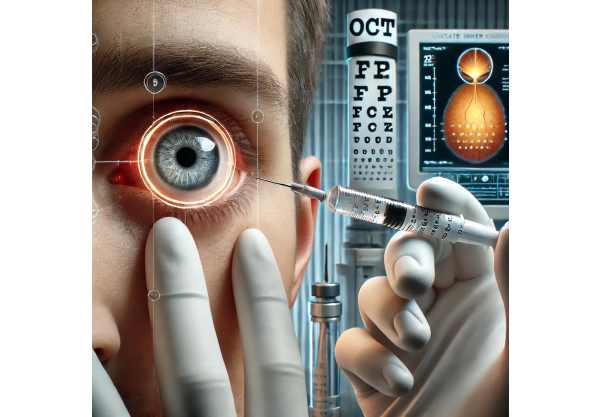
Patients with PIC frequently report blurred vision, scotomas (blind spots), and photopsia. A comprehensive eye examination is typically used to diagnose the condition, which includes imaging techniques such as optical coherence tomography (OCT) and fluorescein angiography to visualize lesions and assess their impact on retinal structures.
Although the exact cause of PIC is unknown, it is thought to be linked to an autoimmune response in which the body’s immune system incorrectly attacks its own tissues. PIC’s episodic nature, with flare-ups and remissions, lends credence to this hypothesis. Understanding PIC is critical for early detection and intervention, which can help preserve vision and improve the quality of life for those suffering from this condition.
Typical Punctate Inner Choroidopathy Management
The goals of Punctate Inner Choroidopathy (PIC) management and treatment are to reduce inflammation, avoid complications, and preserve vision. Given the chronic and recurrent nature of PIC, long-term monitoring and a combination of therapeutic approaches are frequently necessary.
Non-surgical Treatments
The primary goal of nonsurgical treatments is to reduce inflammation and regulate the immune response. Common nonsurgical treatments include:
- Corticosteroids: These are the most commonly used medications to treat PIC. Corticosteroids are available orally, intravenously, and as periocular injections. They effectively reduce inflammation and manage acute flare-ups. However, prolonged use of corticosteroids can result in side effects such as increased intraocular pressure, cataract formation, and systemic complications.
- Immunosuppressive Agents: Patients who do not respond well to corticosteroids or who require long-term treatment may be given immunosuppressive drugs such as methotrexate, azathioprine, or mycophenolate mofetil. These medications help to regulate the immune response and reduce inflammation. Regular monitoring is essential for managing potential side effects and ensuring treatment efficacy.
- Biologic Agents: Recently, biologic agents such as anti-TNF (tumor necrosis factor) drugs have been investigated for the treatment of PIC. These medications target specific immune system components and can help patients with severe or refractory conditions. Examples include adalimumab and infliximab. When conventional treatments fail or are intolerable, biologic agents are usually considered.
Surgical Treatments
In some cases, surgical intervention may be required to treat complications associated with PIC, such as choroidal neovascularization (CNV), which can cause significant vision loss if left untreated.
- Laser Photocoagulation: This procedure uses laser energy to destroy abnormal blood vessels that form in the choroid due to CNV. Laser photocoagulation can help to prevent further leakage and retinal damage. However, it is typically reserved for well-defined lesions located away from the fovea (central part of the retina) to reduce the risk of damaging central vision.
- Photodynamic Therapy (PDT): PDT uses a photosensitizer (verteporfin) and a non-thermal laser to selectively target and close abnormal blood vessels. This treatment is especially useful for CNV near the fovea, where conventional laser treatment would result in a higher risk of vision loss. PDT has a favorable safety profile and can be repeated as needed.
Monitoring and Supportive Care
Patients with PIC require regular monitoring to detect changes in their condition and adjust treatment plans as needed. This typically includes regular eye exams, imaging studies, and visual function tests. Supportive care, such as the use of low-vision aids and counseling, can also assist patients in coping with the visual impairment associated with PIC.
Innovative Treatments for Punctate Inner Choroidopathy
Recent advances in understanding and treating Punctate Inner Choroidopathy (PIC) have resulted in the development of novel therapies and techniques to improve patient outcomes. These cutting-edge innovations include pharmacological advances, novel imaging technologies, and regenerative medicine approaches that are revolutionizing PIC treatment.
Advanced Pharmacological Therapies
The development of targeted pharmacological therapies has transformed the treatment landscape for PIC, providing new hope for patients suffering from this difficult condition.
- Intravitreal Injections: Anti-VEGF (vascular endothelial growth factor) agents like ranibizumab (Lucentis) and aflibercept (Eylea) have shown promise in treating CNV associated with PIC. These medications prevent the formation of abnormal blood vessels and reduce fluid leakage, thereby stabilizing or improving vision. Intravitreal injections are administered as an outpatient procedure and may be repeated on a regular basis depending on the patient’s response.
- New Immunomodulatory Drugs: Research into new immunomodulatory drugs is ongoing, with the goal of developing treatments that are more effective and have fewer side effects than traditional immunosuppressive medications. For example, JAK inhibitors, which block specific immune response pathways, are being studied for their potential to treat autoimmune ocular conditions such as PIC. Early research suggests that these drugs may provide a more targeted approach to inflammation control without causing widespread immunosuppression like older medications.
Innovative Imaging Techniques
Imaging technology advancements have greatly improved PIC diagnosis and monitoring, allowing for more precise and personalized treatment approaches.
- Enhanced Depth Imaging Optical Coherence Tomography (EDI-OCT): EDI-OCT generates high-resolution cross-sectional images of the choroid, allowing for detailed visualization of lesions and measurement of choroidal thickness. This imaging technique is especially useful for tracking disease progression and response to treatment over time.
- Optical Coherence Tomography Angiography (OCTA): OCTA is a non-invasive imaging technique that provides detailed images of blood flow in the retina and choroid. Unlike traditional fluorescein angiography, OCTA is dye-free, making it safer and more comfortable for patients. OCTA can detect early signs of CNV and monitor changes in vascular structures, allowing for timely treatment initiation.
Regenerative Medicine & Gene Therapy
Regenerative medicine and gene therapy hold great promise for the future treatment of PIC, with potential solutions for restoring vision and repairing damaged tissue.
- Stem Cell Therapy: Stem cell therapy aims to regenerate damaged retinal and choroidal tissues, with the potential to reverse the effects of PIC. Researchers are investigating the use of induced pluripotent stem cells (iPSCs) and mesenchymal stem cells (MSCs) to create treatments that can restore normal function in the affected areas. While still in the experimental stages, early results are encouraging and indicate that stem cell therapy may become a viable option in the future.
- Gene Therapy: Gene therapy is the process of introducing genetic material into cells to correct or compensate for defective genes. In the case of PIC, gene therapy could target specific genetic factors that contribute to inflammatory response and choroidal damage. Advances in CRISPR-Cas9 technology and viral vector delivery systems have made gene therapy a more viable and precise treatment option for ocular diseases.
Personalized Medical Approaches
The personalized medicine trend is also making its way into PIC treatment, with therapies tailored to individual patient profiles using genetic, molecular, and clinical data.
- Genetic Profiling: Genetic profiling can help identify patients who are more likely to develop PIC and tailor treatment strategies accordingly. Understanding the genetic factors that contribute to the disease allows clinicians to develop more targeted and effective treatment plans, lowering the risk of flare-ups and complications.
- Biomarker Analysis: Biomarkers are quantitative indicators of disease activity or response to treatment. Advances in biomarker research are allowing for the identification of specific molecules associated with PIC, which can be used to track disease progression and guide treatment decisions. For example, elevated levels of certain inflammatory cytokines in the blood or ocular fluids may indicate active disease and the need for more aggressive treatment.






