Seasonal Affective Disorder (SAD) is a form of depression characterized by its predictable pattern linked to changing seasons. Typically emerging in late autumn and easing by spring, SAD affects mood, energy, appetite, and social engagement. While mild “winter blues” occur in many individuals, SAD can significantly impair daily functioning, making work, relationships, and personal interests challenging. Factors like reduced sunlight, disrupted biological rhythms, and genetic predisposition all play a role. However, understanding the underlying mechanisms and available treatments—from light therapy to lifestyle adjustments—enables people to recognize symptoms early and take control of their mental health through evidence-based strategies.
Table of Contents
- Deep Dive into SAD
- Identifying Key Indicators
- Contributing Factors and Proactive Measures
- Diagnostic Process
- Relief and Recovery Approaches
- Common Questions about SAD
Deep Dive into SAD
Seasonal Affective Disorder (SAD) is categorized as a specifier of major depressive disorder or bipolar disorder, defined by recurrent depressive episodes that follow a seasonal pattern. On average, about 1 in 20 adults living in higher-latitude regions experience SAD, and up to one-fifth report milder, subclinical “winter blues.” The hallmark of SAD is its timing: symptoms reliably appear in late autumn or early winter and resolve during spring or early summer for at least two consecutive years.
At the biological level, there are three primary mechanisms implicated:
- Circadian misalignment: Shorter daylight hours can delay or disrupt the body’s internal clock (the suprachiasmatic nucleus in the hypothalamus), leading to an overproduction of melatonin at inappropriate times. This hormone regulates sleep–wake cycles, so excess can cause daytime drowsiness and lethargy.
- Neurochemical changes: Sunlight exposure influences serotonin levels, a neurotransmitter closely linked to mood. Reduced light can impair serotonin synthesis, transport, and receptor activity, contributing to depressive symptoms.
- Hormonal fluctuations: Alongside melatonin, other hormones such as cortisol and endorphins may fluctuate with changing seasons, affecting stress response and emotional regulation.
Genetic predisposition also plays a role—having a close family member with a mood disorder significantly increases one’s risk. Environmental factors compound the issue: living farther from the equator, experiencing extended overcast weather, or enduring long commute times indoors during winter all reduce natural light exposure. Social rhythms can shift too, as holiday stress, financial strain, and reduced outdoor activities place additional emotional burdens on individuals.
Understanding this multifaceted picture—where neurobiology, genetics, and environment intersect—helps clarify why some people breeze through darker months while others struggle with profound mood disturbances. Recognizing SAD as a distinct entity, rather than a passing mood change, underscores the importance of early awareness and intervention. In the sections that follow, we’ll explore how to spot the signs, identify risk factors, confirm a diagnosis, and build a comprehensive care plan that blends medical, psychological, and lifestyle strategies to help you navigate seasonal challenges with confidence.
Identifying Key Indicators
Distinguishing SAD from general low mood hinges on recognizing consistent, seasonal patterns in symptoms. While occasional sad days are normal, SAD manifests through clusters of emotional, cognitive, and physical changes that recur annually:
Emotional and social signs
- Persistent low mood, feelings of hopelessness, or tearfulness
- Heightened irritability, anxiety, or social withdrawal
- Loss of interest in hobbies and reduced enjoyment of once-pleasurable activities
Sleep disturbances
- Hypersomnia: sleeping longer yet still feeling fatigued
- Difficulty waking up in the morning, even with sufficient hours in bed
- Daytime drowsiness interfering with work or daily tasks
Appetite and weight shifts
- Strong cravings for carbohydrates and sweets
- Noticeable weight gain during colder months
- Digestive issues linked to dietary changes and reduced physical activity
Cognitive and motivational changes
- Trouble concentrating, forgetfulness, or slowed decision-making
- Low motivation, feeling “heavy” in arms and legs, difficulty initiating tasks
Functional impairment
- Declines in work or academic performance
- Strained relationships due to irritability or reduced participation in social events
To pinpoint these indicators:
- Keep a Seasonal Diary: Track mood, sleep duration, energy levels, diet, and outdoor exposure daily. Over weeks or months, patterns often emerge.
- Use Screening Questionnaires: Tools such as the Seasonal Pattern Assessment Questionnaire (SPAQ) or the Beck Depression Inventory (BDI) can help quantify symptom severity and seasonality.
- Monitor Impact on Life Domains: Note whether changes significantly impair professional responsibilities, personal relationships, or self-care routines.
If you observe a clear link between symptom onset in autumn or winter and improvement in spring or summer over multiple years, discuss these findings with a healthcare professional. Early recognition and documentation of key indicators increase the likelihood of timely, targeted interventions, reducing the duration and severity of each episode.
Contributing Factors and Proactive Measures
Several risk factors heighten vulnerability to SAD, yet proactive strategies can mitigate their impact:
Risk Factors
- Geographic latitude: Higher latitudes with shorter winter days correlate with greater SAD prevalence.
- Climate patterns: Regions with frequent cloud cover or prolonged rainy seasons see elevated rates.
- Demographics: Women are diagnosed more often than men. Onset typically occurs between ages 18 and 30.
- Personal and family history: A prior mood disorder or a relative with depression increases risk.
- Lifestyle influences: Sedentary behavior, limited outdoor activity, and irregular sleep schedules exacerbate symptoms.
Proactive Measures
- Maximize Light Exposure
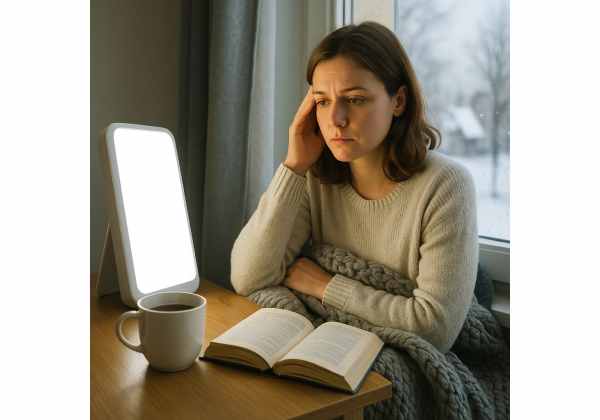
- Morning phototherapy: Use a 10,000-lux light box for 20–30 minutes each morning. Position it about 16–24 inches from your eyes while reading or working.
- Dawn simulation: Alarm clocks that gradually increase light can ease morning grogginess and synchronize circadian rhythms.
- Window optimization: Sit near south- or east-facing windows, keep blinds open, and trim outdoor foliage that blocks sunlight.
- Maintain a Consistent Routine
- Regular sleep–wake times: Go to bed and wake up at the same times daily, even on weekends, to stabilize internal clocks.
- Structured meals: Eat balanced meals at consistent intervals to regulate blood sugar and energy levels.
- Incorporate Physical Activity
- Daily movement: Aim for 30 minutes of moderate exercise—walking, jogging, cycling—ideally outdoors midday when natural light peaks.
- Group classes or accountability: Yoga, dance, or team sports can combine social interaction with exercise, boosting mood and motivation.
- Optimize Nutrition
- Omega-3 fatty acids: Foods like salmon, flaxseeds, and walnuts support brain function.
- Vitamin D supplementation: Many individuals have low vitamin D in winter; consult your provider for targeted dosing.
- Whole foods focus: Limit refined sugars and processed carbs that can trigger energy crashes and mood swings.
- Cultivate Social and Stress-Management Practices
- Regular check-ins: Schedule weekly calls, coffee dates, or virtual gatherings with friends and family to counter isolation.
- Mind–body activities: Meditation, tai chi, and deep-breathing exercises reduce stress hormones and foster emotional balance.
- Digital detox: Set boundaries on screens before bed to improve sleep quality and decrease anxiety.
By layering these strategies before symptoms intensify, you create a robust preventive framework. Even if SAD can’t be fully prevented, proactive measures often lessen episode severity and duration, empowering you to face darker months with greater resilience.
Diagnostic Process
A precise diagnosis paves the way for an effective, personalized treatment plan. The evaluation typically involves:
- Clinical Interview
A mental health professional explores your seasonal symptom history, family psychiatric background, daily functioning, and any coexisting medical conditions. Open discussion about sleep, appetite, and energy patterns is crucial. - Standardized Assessments
- Seasonal Pattern Assessment Questionnaire (SPAQ): Measures the degree of seasonality in mood and behavior.
- Beck Depression Inventory (BDI) or Patient Health Questionnaire-9 (PHQ-9): Assesses overall depressive symptom severity.
- Physical Examination and Laboratory Tests
- Thyroid function tests: Hypothyroidism can mimic depressive symptoms.
- Complete blood count and metabolic panel: Rule out anemia, infections, or nutritional deficiencies.
- Serum vitamin D levels: Low vitamin D is common in winter months and may worsen mood.
- Differential Diagnosis
- Exclude nonseasonal major depressive disorder, bipolar disorder, chronic fatigue syndrome, and other medical or psychiatric conditions that share overlapping symptoms.
- DSM-5 Criteria Confirmation
According to the Diagnostic and Statistical Manual of Mental Disorders, a SAD diagnosis requires:
- Depressive episodes with seasonal onset for at least two consecutive years
- Full remission of symptoms in other seasons
- Absence of nonseasonal depressive episodes during the defined period
- Telehealth and Ongoing Monitoring
Virtual visits can increase access to specialists, especially in remote areas. Regular follow-up—via in-person or telehealth—helps track symptom changes, treatment response, and any side effects.
Accurate identification of SAD versus other disorders ensures that you receive the most appropriate interventions, whether that’s phototherapy, psychotherapy, pharmacotherapy, or a blended approach.
Relief and Recovery Approaches
Effectively managing SAD often involves combining multiple modalities to address biological, psychological, and lifestyle dimensions:
1. Light Therapy (Phototherapy)
- Device selection: A 10,000-lux light box is the gold standard. Look for UV-filtered models with adjustable angles.
- Timing and dosage: Use for 20–30 minutes each morning, ideally within an hour of waking. Consistency every day during winter months is key.
- Side effect management: Some users experience headaches or eye strain; adjusting distance or duration can help.
2. Pharmacological Treatment
- Selective Serotonin Reuptake Inhibitors (SSRIs): Medications such as sertraline, fluoxetine, or paroxetine balance serotonin levels.
- Bupropion XL: Approved specifically for SAD prevention; often initiated in early autumn before symptoms typically begin.
- Medication monitoring: Regular check-ins with your prescriber ensure dosage effectiveness and minimize side effects like insomnia, nausea, or agitation.
3. Psychotherapeutic Interventions
- Cognitive Behavioral Therapy (CBT) for SAD: Focuses on identifying and reframing negative thoughts related to winter’s challenges, and developing structured activity scheduling.
- Interpersonal Therapy (IPT): Addresses relationship issues and life transition stresses that can exacerbate seasonal depression.
- Group therapy or support groups: Provides shared coping strategies and community support during tougher months.
4. Lifestyle and Self-Care Practices
- Regular exercise: Aim for at least 150 minutes of moderate-intensity activity weekly. Outdoor brisk walks—even on cloudy days—boost light exposure.
- Sleep hygiene: Maintain a dark, cool bedroom; limit caffeine and screens before bedtime; wake at a consistent hour.
- Nutrition: Emphasize whole foods—vegetables, lean proteins, complex carbs—and consider supplementing with vitamin D or omega-3 fatty acids under professional guidance.
- Mind–body techniques: Daily practices such as meditation, yoga, or progressive muscle relaxation support stress reduction and emotional equilibrium.
5. Complementary Therapies
- Mindfulness-Based Stress Reduction (MBSR): An eight-week structured program shown to alleviate depressive symptoms.
- Acupuncture and massage therapy: Pilot studies suggest benefits for mood enhancement and stress relief.
- Herbal and nutraceutical adjuncts: Under professional supervision, St. John’s wort or SAMe may complement conventional treatments, though they carry potential interactions.
6. Tracking and Adjustment
- Mood and symptom journal: Record daily mood ratings, therapy sessions, light therapy usage, sleep patterns, and exercise.
- Regular review with provider: Use journal insights to tweak treatment—changing light box duration, therapy focus, or medication dosage as needed.
A comprehensive, flexible plan that combines these approaches often yields the best long-term outcomes, empowering you to navigate seasonal fluctuations with greater well-being and resilience.
Common Questions about SAD
What triggers Seasonal Affective Disorder each year?
SAD is primarily triggered by reduced daylight, which disrupts circadian rhythms and lowers serotonin levels. Genetic predisposition, geographic latitude, and environmental factors like weather patterns also influence who develops seasonal mood changes.
How long does it take light therapy to work?
Most people experience noticeable improvement within one to two weeks of daily 20–30 minute sessions sitting near a 10,000-lux light box. Consistent use every morning throughout the darker months maximizes benefits and helps prevent relapse.
Can dietary changes alone prevent SAD?
While a balanced diet rich in omega-3s, lean protein, and complex carbohydrates supports mood and energy, dietary changes alone rarely prevent SAD. Combining nutrition with light therapy, exercise, and consistent routines typically yields better results.
When is professional help necessary?
Seek professional evaluation if seasonal mood shifts impair daily life—work, relationships, or self-care—for two consecutive winters. Early intervention leads to faster relief and reduces the risk of worsening depressive episodes.
Are there risks if SAD goes untreated?
Untreated SAD can lead to chronic low mood, social withdrawal, and functional impairment. Over time, it may increase vulnerability to other mental health issues such as anxiety disorders or substance misuse as a coping mechanism.
Disclaimer:
This article is for educational purposes only and should not replace professional medical advice. Always consult a qualified healthcare provider for personalized diagnosis and treatment recommendations.
If you found this guide helpful, please share it on Facebook, X (formerly Twitter), LinkedIn, or your favorite platform—and follow us on social media for more health insights. Your support helps us continue producing quality content!






