Skeletal muscles are the powerhouse of the human body, responsible for movement, posture, and heat production. These highly organized tissues play an essential role in every voluntary movement—from the smallest facial expression to running a marathon. Beyond movement, skeletal muscles contribute to metabolic regulation and overall body composition. Their intricate structure, from the macroscopic organization into muscle groups down to the microscopic arrangement of sarcomeres, enables efficient contraction and energy utilization. This guide delves into the detailed anatomy, physiology, common disorders, diagnostic techniques, treatment options, and lifestyle practices that support optimal skeletal muscle health.
Table of Contents
- Anatomical Structure & Histology
- Physiological Functions & Mechanisms
- Common Muscle Disorders
- Diagnostic Methods & Techniques
- Treatment Approaches & Therapies
- Nutritional Support & Supplementation
- Preventative Care & Healthy Practices
- Trusted Resources & Further Reading
- Frequently Asked Questions
Anatomical Structure & Histology
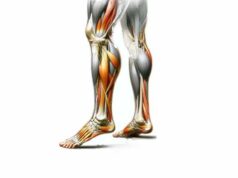
Skeletal muscles are highly organized tissues that exhibit a distinct hierarchy in their structure, allowing them to contract and produce force. At the macroscopic level, muscles are arranged in groups and separated by fascia, while at the microscopic level, the contractile units within muscle fibers orchestrate movement.
Gross Anatomy
Muscle Belly
The muscle belly is the central, fleshy part of a skeletal muscle. It contains bundles of muscle fibers called fascicles, which provide the main contractile force. The size, shape, and orientation of the muscle belly determine the muscle’s overall function and range of motion.
Fascicles
Fascicles are bundles of individual muscle fibers. They are encased in a connective tissue sheath known as the perimysium. The arrangement of fascicles—whether parallel, pennate, or convergent—affects the muscle’s strength and speed of contraction.
Tendons
Tendons are robust bands of connective tissue that attach muscle to bone. They transmit the force generated by muscle contraction to the skeletal system, enabling movement. The structure of tendons is primarily collagen, which provides tensile strength.
Fascia
Fascia is a continuous sheet of connective tissue that envelops muscles and muscle groups. It supports, separates, and provides a conduit for nerves and blood vessels while reducing friction between muscles during movement.
Microscopic Anatomy
Muscle Fibers (Myocytes)
Muscle fibers are long, cylindrical cells that contain multiple nuclei. They are the basic contractile units of skeletal muscle and exhibit a striated appearance due to the regular arrangement of myofibrils.
Myofibrils and Sarcomeres
Within each muscle fiber are myofibrils—bundles of contractile proteins arranged in repeating units called sarcomeres. The sarcomere is the fundamental unit of muscle contraction, composed of thick filaments (myosin) and thin filaments (actin). Z-lines mark the boundaries of sarcomeres and serve as anchor points for actin filaments.
Sarcolemma and Sarcoplasm
The sarcolemma is the cell membrane of a muscle fiber, responsible for transmitting electrical impulses. The sarcoplasm, the cytoplasm of the muscle fiber, contains organelles such as mitochondria, which supply the energy required for contraction.
Sarcoplasmic Reticulum (SR) and T-Tubules
The sarcoplasmic reticulum stores calcium ions, essential for initiating muscle contraction. T-tubules are invaginations of the sarcolemma that facilitate rapid transmission of electrical signals deep into the muscle fiber, ensuring coordinated contraction.
Connective Tissue Layers
- Endomysium:
A fine connective tissue layer that surrounds each individual muscle fiber, providing structural support and housing capillaries and nerve endings. - Perimysium:
Envelops each fascicle, providing a supportive framework for nerve and blood vessel distribution. - Epimysium:
A dense, fibrous sheath that encases the entire muscle, maintaining its integrity and facilitating force transmission to tendons.
Blood Supply and Innervation
Skeletal muscles are richly vascularized, ensuring efficient delivery of oxygen and nutrients while removing metabolic wastes.
- Arterial Supply:
Arteries branch into arterioles and capillaries that penetrate muscle fibers. - Venous Drainage:
Veins collect deoxygenated blood and return it to the heart. - Innervation:
Motor neurons from the central nervous system innervate skeletal muscles at the neuromuscular junction, where they transmit electrical impulses that trigger muscle contraction.
Types of Muscle Fibers
Skeletal muscles consist of different fiber types, each specialized for distinct functions:
- Type I (Slow-Twitch) Fibers:
Rich in mitochondria and myoglobin, these fibers are adapted for endurance and continuous, low-intensity activities. - Type II (Fast-Twitch) Fibers:
Designed for rapid, powerful contractions, these fibers are subdivided into Type IIa (intermediate) and Type IIb (glycolytic), which vary in their fatigue resistance and energy production mechanisms.
Muscle Attachments
- Origin and Insertion:
The origin is the fixed attachment of a muscle, while the insertion is the movable attachment that translates muscle contraction into movement. - Lever Mechanics:
Muscles act as levers on bones, with the force and range of motion determined by the relative positions of their origins, insertions, and joints.
Understanding the intricate architecture of skeletal muscles is essential to appreciate their role in generating movement, maintaining posture, and supporting overall bodily functions.
Physiological Functions & Mechanisms
Skeletal muscles are central to virtually every voluntary movement and play key roles in metabolism, thermoregulation, and overall health. Their dynamic functions arise from the coordinated interplay between cellular structures, biochemical pathways, and neural control.
Muscle Contraction Process
Muscle contraction involves a complex series of events that transform electrical signals into mechanical force:
- Excitation-Contraction Coupling:
A motor neuron releases acetylcholine at the neuromuscular junction, generating an action potential that travels along the sarcolemma and into T-tubules. - Calcium Release:
The action potential triggers the sarcoplasmic reticulum to release calcium ions into the sarcoplasm. - Cross-Bridge Formation:
Calcium binds to troponin, shifting tropomyosin and exposing binding sites on actin. Myosin heads attach to actin, forming cross-bridges. - Power Stroke:
The myosin heads pivot, pulling the actin filaments toward the center of the sarcomere, which shortens the muscle fiber. - Relaxation:
Calcium is pumped back into the sarcoplasmic reticulum, and the muscle fiber relaxes as tropomyosin covers the binding sites again.
Energy Metabolism in Muscles
Muscle contraction is powered by adenosine triphosphate (ATP), produced through:
- Aerobic Metabolism:
Efficient ATP production via oxidative phosphorylation, ideal for sustained, low-intensity activities. - Anaerobic Glycolysis:
Rapid ATP generation for high-intensity, short-duration activities, though accompanied by lactate accumulation. - Phosphocreatine System:
Provides immediate ATP during the initial seconds of intense activity.
Functions Beyond Movement
Skeletal muscles contribute to several other essential functions:
- Posture and Stability:
Continuous low-level contractions maintain posture and joint stability, allowing the body to remain upright against gravity. - Heat Production:
Muscle metabolism generates heat as a byproduct of contraction, helping to regulate body temperature. - Support for Circulation:
Muscle contractions assist in venous return by compressing blood vessels during movement.
Muscle Adaptation and Plasticity
Muscles exhibit remarkable plasticity, adapting to various stimuli such as exercise, injury, and hormonal changes:
- Hypertrophy:
The enlargement of muscle fibers due to increased protein synthesis, often induced by resistance training. - Atrophy:
A decrease in muscle mass and strength, which can occur due to disuse, aging, or illness. - Fiber Type Transformation:
Under certain conditions, muscle fibers can adapt their metabolic properties (e.g., from fast-twitch to more fatigue-resistant profiles) to meet functional demands.
These physiological mechanisms underpin the diverse roles of skeletal muscles, from generating rapid, forceful movements to sustaining prolonged activity and maintaining overall homeostasis.
Common Muscle Disorders & Conditions
Skeletal muscles are subject to various disorders that can impair their function and affect quality of life. Understanding these conditions is vital for early diagnosis, effective treatment, and long-term management.
Muscle Sprains and Tears
Muscle strains, commonly known as pulled muscles, occur when muscle fibers are overstretched or torn.
- Grades of Injury:
- Grade I: Minor stretching with minimal pain and no significant loss of function.
- Grade II: Partial tear with moderate pain, swelling, and reduced strength.
- Grade III: Complete tear, often requiring surgical intervention.
- Symptoms:
Sudden pain, swelling, bruising, and loss of function in the affected muscle. - Causes:
Overuse, sudden movements, or inadequate warm-up before exercise.
Muscle Cramps
Muscle cramps are involuntary contractions that cause sudden, intense pain and temporary loss of function.
- Causes:
Dehydration, electrolyte imbalances (low potassium or magnesium), overexertion, or nerve compression. - Management:
Stretching, hydration, and electrolyte replacement, along with massage and heat application.
Myopathies
Myopathies are disorders characterized by muscle weakness and dysfunction.
- Inflammatory Myopathies:
Conditions like polymyositis and dermatomyositis involve immune-mediated muscle inflammation, leading to progressive weakness and pain. - Genetic Myopathies:
Duchenne and Becker muscular dystrophies are inherited disorders that cause muscle degeneration and weakness over time. - Metabolic Myopathies:
Disorders such as McArdle disease impair energy metabolism in muscles, causing exercise intolerance and pain.
Rhabdomyolysis
Rhabdomyolysis is a severe condition in which muscle fibers break down rapidly, releasing myoglobin into the bloodstream.
- Symptoms:
Intense muscle pain, swelling, dark (tea-colored) urine, and potential kidney failure. - Causes:
Severe trauma, prolonged muscle overexertion, drug or alcohol abuse, and infections. - Treatment:
Immediate fluid resuscitation, electrolyte management, and close monitoring of kidney function.
Fibromyalgia
Fibromyalgia is a chronic condition characterized by widespread musculoskeletal pain, fatigue, and tender points.
- Symptoms:
Persistent muscle pain, sleep disturbances, cognitive difficulties (fibro fog), and mood changes. - Causes:
The exact cause is unclear, but it is thought to involve abnormal pain processing in the central nervous system. - Management:
Combination of medication, physical therapy, stress reduction, and lifestyle modifications.
Tendonitis and Bursitis
Tendonitis is the inflammation of tendons, while bursitis is the inflammation of the fluid-filled sacs (bursae) that cushion joints.
- Common Causes:
Overuse, repetitive motions, and acute injury. - Symptoms:
Pain, swelling, and limited movement in the affected area. - Treatment:
Rest, NSAIDs, corticosteroid injections, physical therapy, and, in severe cases, surgery.
Compartment Syndrome
Compartment syndrome occurs when increased pressure within a muscle compartment restricts blood flow and causes tissue damage.
- Symptoms:
Severe pain, swelling, numbness, and muscle weakness. - Causes:
Trauma, crush injuries, or intense physical activity. - Treatment:
Emergency fasciotomy to relieve pressure and prevent permanent damage.
Other Conditions
- Chronic Muscle Fatigue and Weakness:
Conditions like myositis and metabolic myopathies can lead to persistent muscle fatigue and reduced strength. - Exercise-Induced Muscle Damage:
Overexertion during exercise may lead to muscle soreness and damage, which typically resolves with rest and proper recovery techniques.
Understanding the spectrum of skeletal muscle disorders is essential for prompt diagnosis and effective treatment, helping to maintain mobility, strength, and overall quality of life.
Diagnostic Methods & Techniques
Evaluating skeletal muscle disorders requires a comprehensive, multidisciplinary approach that incorporates clinical assessments, imaging studies, laboratory tests, and specialized diagnostic procedures.
Clinical Evaluation
- Medical History:
A detailed history covers the onset, duration, and progression of symptoms, including pain, weakness, and any triggering events. The history may also reveal previous injuries, exercise habits, and family history of neuromuscular disorders. - Physical Examination:
Clinicians assess muscle strength, tone, and range of motion through various tests. Palpation of affected muscles helps identify tenderness, swelling, or abnormal masses. Reflex testing and gait analysis also provide valuable insights.
Imaging Techniques
- Magnetic Resonance Imaging (MRI):
MRI is the gold standard for visualizing muscle tissue. It offers high-resolution images that can detect muscle tears, inflammation, tumors, and other abnormalities. - Ultrasound:
Ultrasound imaging is a dynamic, non-invasive method used to evaluate muscle structure and function in real time. It can detect fluid collections, fiber disruptions, and other changes. - Computed Tomography (CT) Scan:
CT imaging provides detailed cross-sectional views of muscle and bone, useful in trauma or when MRI is contraindicated. - X-rays:
Although primarily used for bone imaging, X-rays can sometimes reveal soft tissue swelling and calcifications associated with chronic muscle conditions.
Electromyography (EMG) and Nerve Conduction Studies (NCS)
- Electromyography (EMG):
EMG measures the electrical activity of muscles, providing data on muscle function at rest and during contraction. Abnormal electrical patterns can indicate muscle damage, inflammation, or neuromuscular disorders. - Nerve Conduction Studies (NCS):
These studies assess the speed and amplitude of electrical signals along peripheral nerves, helping differentiate muscle disorders from nerve injuries.
Laboratory Tests
- Blood Tests:
Measurement of muscle enzymes such as creatine kinase (CK) helps assess muscle damage. Inflammatory markers like C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) indicate systemic inflammation. - Autoantibody Panels:
Tests for antibodies (e.g., ANA, anti-Jo-1) are used to diagnose autoimmune myopathies. - Genetic Testing:
Genetic assays identify mutations associated with inherited muscle disorders, such as muscular dystrophies, aiding in diagnosis and family counseling.
Muscle Biopsy
- Procedure:
A muscle biopsy involves removing a small sample of muscle tissue for histopathological examination. This is often performed via needle biopsy or small surgical incision. - Histological Analysis:
Examination under the microscope reveals muscle fiber size, shape, and integrity, as well as the presence of inflammation, fibrosis, or abnormal protein deposits. Special stains and immunohistochemistry can help diagnose specific myopathies.
Advanced Diagnostic Techniques
- Magnetic Resonance Spectroscopy (MRS):
MRS evaluates the chemical composition of muscle tissue, detecting metabolic abnormalities that may not be visible on standard MRI. - Positron Emission Tomography (PET) Scan:
PET scans assess metabolic activity and can detect areas of increased muscle metabolism or inflammation, particularly useful in evaluating tumors. - Optical Coherence Tomography (OCT):
A non-invasive imaging technique that provides high-resolution, cross-sectional images of muscle tissue, useful for early detection of structural changes.
Functional Assessments
- Isokinetic Dynamometry:
This test measures muscle strength and endurance under controlled conditions, providing objective data on muscle performance. - Gait Analysis:
Analyzing walking patterns helps assess muscle function, coordination, and balance, offering insights into the functional impact of muscle disorders.
Through a combination of these diagnostic tools, clinicians can accurately evaluate skeletal muscle health, identify underlying disorders, and guide effective treatment plans tailored to each patient’s needs.
Treatment Approaches & Therapies
The management of skeletal muscle disorders depends on the type and severity of the condition. Treatment strategies range from conservative therapies to advanced surgical interventions, with the goal of restoring muscle function, reducing pain, and preventing further damage.
Conservative and Medical Management
Rest and Recovery
- RICE Protocol:
Rest, Ice, Compression, and Elevation are fundamental in the immediate management of muscle sprains and tears to reduce swelling and prevent further injury. - Medications:
Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naproxen alleviate pain and reduce inflammation. Acetaminophen is used for pain relief when anti-inflammatory effects are not required.
Physical Therapy and Rehabilitation
- Stretching and Strengthening Exercises:
A customized exercise program helps restore muscle strength, flexibility, and endurance after injury. - Functional Training:
Physical therapy includes techniques to improve range of motion, balance, and coordination, crucial for regaining everyday function. - Modalities:
Techniques such as ultrasound therapy, electrical stimulation, and massage can promote healing and reduce muscle tightness.
Pharmacological Interventions for Specific Myopathies
- Immunosuppressants:
In inflammatory myopathies such as polymyositis and dermatomyositis, corticosteroids and other immunosuppressive agents (e.g., methotrexate, azathioprine) reduce muscle inflammation. - Metabolic Modulators:
For metabolic myopathies, dietary modifications and specific enzyme supplements may enhance muscle energy production. - Gene Therapy (Experimental):
Emerging treatments for genetic myopathies, such as Duchenne muscular dystrophy, focus on gene editing and exon skipping to restore functional protein expression.
Treatment of Acute Muscle Injuries
Muscle Sprains and Tears
- RICE Protocol:
Immediate application of rest, ice, compression, and elevation minimizes tissue damage. - Pain Management:
NSAIDs and acetaminophen reduce pain and inflammation. - Surgical Repair:
Severe Grade III tears may require surgical intervention to repair damaged muscle fibers.
Rhabdomyolysis Management
- Aggressive Fluid Resuscitation:
Intravenous fluids help flush myoglobin and prevent kidney damage. - Electrolyte Management:
Monitoring and correcting electrolyte imbalances are critical to avoid complications. - Supportive Therapies:
Diuretics and bicarbonate may be administered to enhance renal clearance and prevent myoglobin-induced injury.
Treatment of Chronic Conditions
Fibromyalgia
- Medications:
Antidepressants (e.g., amitriptyline, duloxetine) and anticonvulsants (e.g., pregabalin, gabapentin) help alleviate pain and improve sleep. - Lifestyle Modifications:
Regular low-impact exercise, stress management techniques, and cognitive behavioral therapy (CBT) are crucial. - Physical Therapy:
Tailored exercise programs improve muscle strength and reduce pain.
Tendonitis and Bursitis
- Conservative Management:
Rest, activity modification, and ice application reduce inflammation. - Medications:
NSAIDs and corticosteroid injections offer symptomatic relief. - Physical Therapy:
Specific stretching and strengthening exercises improve function and prevent recurrence. - Surgical Intervention:
In refractory cases, surgical repair or debridement may be necessary.
Myopathies
- Immunosuppressive Therapy:
For inflammatory myopathies, long-term treatment with corticosteroids and immunomodulators can slow disease progression. - Supportive Rehabilitation:
Physical and occupational therapy aid in maintaining muscle function and improving quality of life. - Experimental Therapies:
Gene therapies and novel pharmacologic agents are under investigation for inherited myopathies.
Advanced and Minimally Invasive Procedures
- Endoscopic Procedures:
For conditions like ejaculatory duct obstruction affecting muscle groups in the pelvic region, endoscopic techniques offer minimally invasive treatment options. - Surgical Interventions:
In cases of severe muscle damage or tumors, surgical repair and resection remain essential. Minimally invasive approaches, including arthroscopy and laparoscopic surgery, help reduce recovery time and postoperative complications. - Regenerative Medicine:
Emerging treatments such as stem cell therapy and platelet-rich plasma (PRP) injections aim to enhance muscle repair and regeneration after injury.
Nutritional Support & Supplementation
Nutrition plays a pivotal role in the maintenance and recovery of skeletal muscle function. A balanced diet, complemented by targeted supplements, provides the building blocks for muscle repair, growth, and overall performance.
Macronutrients and Protein
- Protein:
Adequate protein intake is essential for muscle repair and hypertrophy. High-quality protein sources such as lean meats, dairy, legumes, and plant-based proteins provide essential amino acids. - Amino Acids:
Supplementing with branched-chain amino acids (BCAAs) and L-glutamine can stimulate muscle protein synthesis, reduce muscle breakdown, and aid recovery.
Micronutrients and Minerals
- Vitamin D:
Crucial for muscle function and bone health, vitamin D supports muscle contraction and overall physical performance. - Magnesium:
Essential for energy production, magnesium helps prevent muscle cramps and supports relaxation. - Zinc:
Plays a vital role in protein synthesis and immune function, contributing to muscle repair and recovery. - B Vitamins:
Vitamins B6 and B12 are key for metabolic processes and help maintain muscle energy levels.
Antioxidants
Antioxidants protect muscle tissues from oxidative stress caused by intense exercise and injury.
- Vitamin C and E:
These vitamins help neutralize free radicals and reduce inflammation. - Selenium:
An important trace mineral with antioxidant properties that supports cellular repair. - Glutathione:
The master antioxidant that aids in detoxification and muscle recovery.
Specialized Supplements
- Creatine:
Proven to enhance muscle strength and performance by replenishing ATP stores during high-intensity exercise. - Omega-3 Fatty Acids:
Found in fish oil, these have anti-inflammatory effects that help reduce muscle soreness and promote recovery. - Coenzyme Q-10 (CoQ10):
Enhances mitochondrial function and energy production in muscle cells. - Curcumin:
Derived from turmeric, curcumin reduces inflammation and may expedite muscle recovery. - L-Arginine:
Supports nitric oxide production, improving blood flow to muscles, which aids in nutrient delivery and waste removal.
Integrating these nutritional strategies through a balanced diet and proper supplementation can support muscle performance, expedite recovery, and reduce the risk of injury.
Preventative Care & Healthy Practices
Maintaining optimal skeletal muscle health is crucial for overall mobility, strength, and quality of life. Preventative strategies encompass lifestyle modifications, proper training practices, and proactive healthcare.
Diet and Hydration
- Balanced Diet:
A nutrient-rich diet consisting of lean proteins, whole grains, fruits, and vegetables provides essential nutrients for muscle repair and growth. - Adequate Hydration:
Drinking sufficient water throughout the day is essential for muscle function, preventing cramps, and facilitating recovery.
Exercise and Training
- Regular Physical Activity:
Engaging in a balanced exercise regimen that includes resistance training, aerobic exercise, and flexibility work maintains muscle mass and function. - Proper Warm-Up and Cool-Down:
Always perform a thorough warm-up before workouts and a cool-down afterward to reduce injury risk and promote recovery. - Periodization and Recovery:
Implement training cycles with adequate rest to avoid overtraining and allow muscles to rebuild and strengthen.
Posture and Ergonomics
- Maintain Good Posture:
Good posture reduces undue stress on muscles and minimizes the risk of strain and injury. - Ergonomic Practices:
Ensure that your workspace and daily activities are ergonomically optimized to prevent chronic muscle strain.
Stress and Sleep
- Stress Management:
Chronic stress can lead to muscle tension and hinder recovery. Practices like meditation, yoga, and deep breathing exercises are effective in reducing stress levels. - Quality Sleep:
Aim for 7–9 hours of restful sleep per night, as sleep is critical for muscle recovery and hormonal balance.
Regular Health Check-Ups
- Routine Medical Examinations:
Regular check-ups can detect early signs of muscle disorders, nutrient deficiencies, or other health issues. - Monitoring Physical Performance:
Track changes in strength, endurance, and overall performance to catch potential problems early and adjust your training or lifestyle accordingly.
By integrating these preventative practices into daily routines, you can safeguard muscle health, optimize performance, and enhance overall quality of life.
Trusted Resources & Further Reading
For additional insights and expert guidance on skeletal muscle health, consider these trusted resources:
Books
- “Strength Training Anatomy” by Frederic Delavier:
Provides detailed illustrations and comprehensive explanations of muscle anatomy and strength training principles. - “Science and Development of Muscle Hypertrophy” by Brad Schoenfeld:
Explores the scientific basis for muscle growth and offers evidence-based training recommendations. - “Muscle: Confessions of an Unlikely Bodybuilder” by Samuel Fussell:
A unique perspective on muscle physiology and the personal journey of understanding muscle development.
Academic Journals
- Journal of Applied Physiology:
Publishes research on muscle function, adaptation, and metabolism related to exercise and health. - Muscle & Nerve:
Focuses on clinical and basic research concerning muscle diseases and neuromuscular disorders. - European Journal of Applied Physiology:
Offers articles on the effects of exercise and physical activity on muscle physiology and overall health.
Mobile Apps
- MyFitnessPal:
A popular nutrition and fitness tracker that helps manage dietary intake and monitor exercise, supporting muscle health. - StrongLifts 5×5:
A strength training app that provides guided workouts aimed at muscle building and performance enhancement. - Fitbod:
Offers personalized workout plans that adjust to your fitness level, ensuring balanced training and muscle recovery.
Frequently Asked Questions on Skeletal Muscles
What are the primary functions of skeletal muscles?
Skeletal muscles are responsible for voluntary movement, maintaining posture, producing heat, and supporting overall bodily functions through coordinated contraction and relaxation.
How do muscles generate force?
Muscle force is generated through the process of muscle contraction, which involves electrical signals, calcium release, and the interaction between actin and myosin filaments within sarcomeres.
What causes muscle fatigue during exercise?
Muscle fatigue can result from the accumulation of metabolic byproducts like lactate, depletion of ATP, or impaired calcium handling within muscle cells during prolonged or intense exercise.
How can muscle recovery be improved after workouts?
Improved muscle recovery can be achieved through proper nutrition, adequate hydration, sufficient sleep, and the inclusion of rest days in training regimens. Supplements like protein, BCAAs, and omega-3s also help.
What lifestyle changes support long-term muscle health?
Maintaining a balanced diet, regular exercise, proper hydration, good posture, stress management, and regular medical check-ups are crucial for preserving muscle strength, preventing injuries, and promoting overall health.
Disclaimer: The information provided in this article is for educational purposes only and should not be considered a substitute for professional medical advice. Always consult a healthcare provider for any concerns regarding your health.
Please share this article on Facebook, X (formerly Twitter), or your preferred social media platform to help spread awareness about skeletal muscle health and modern treatment strategies.