The skin is the largest organ of the body, serving as a vital barrier between the internal environment and external hazards. It plays a multifaceted role in protection, sensation, thermoregulation, and metabolism, while also contributing to aesthetics and overall well-being. This guide provides an in-depth exploration of skin anatomy, its essential functions, common conditions that affect it, and the most effective treatment options. Whether you’re looking to understand its complex structure or seeking tips to maintain healthy skin, this comprehensive resource offers expert insights and practical advice for optimal skin health.
Table of Contents
- Anatomical Structure & Histology
- Physiological Functions & Mechanisms
- Common Skin Conditions
- Diagnostic Techniques & Assessments
- Treatment Approaches & Therapies
- Nutritional Support & Supplementation
- Preventative Care & Healthy Practices
- Trusted Resources & Further Reading
- Frequently Asked Questions
Anatomical Structure & Histology
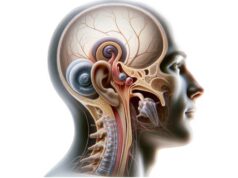
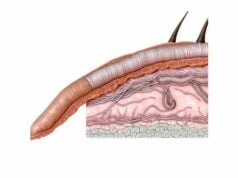
The skin is a complex, multi-layered organ that provides a dynamic interface between the body and its external environment. Its structure is divided into three primary layers—each with unique roles and compositions—that work in unison to offer protection, sensory perception, and homeostatic regulation.
Epidermis
The epidermis is the outermost layer and serves as the primary barrier against environmental aggressors.
- Stratum Corneum:
The outermost sublayer composed of dead, keratin-rich cells. These flattened cells, called corneocytes, are continuously shed and replaced, creating a resilient barrier that limits water loss and prevents microbial invasion. - Stratum Lucidum:
Present only in thick skin (palms and soles), this clear layer provides an additional protective barrier against friction. - Stratum Granulosum:
Contains keratinocytes in the process of keratinization, filled with keratohyalin granules that help form the protein keratin. - Stratum Spinosum:
Characterized by its spiny appearance due to desmosomal connections, this layer provides strength and flexibility. Langerhans cells present here serve as immune sentinels. - Stratum Basale:
The deepest epidermal layer is composed of a single row of continuously dividing basal cells, which give rise to new keratinocytes. Melanocytes in this layer produce melanin, the pigment that determines skin color and protects against UV radiation.
Dermis
Beneath the epidermis lies the dermis, a thick and robust layer that supports the skin’s mechanical properties.
- Papillary Dermis:
The superficial portion containing loose connective tissue with dermal papillae that interdigitate with the epidermis, enhancing nutrient exchange. This layer is richly vascularized and houses sensory nerve endings. - Reticular Dermis:
The deeper, denser layer made of collagen and elastin fibers. It provides tensile strength and elasticity to the skin and contains hair follicles, sweat and sebaceous glands, blood vessels, and nerves. - Accessory Structures:
Embedded within the dermis are structures such as hair follicles, sweat glands, and sebaceous glands. These components are integral to functions like thermoregulation, lubrication, and protection.
Hypodermis (Subcutaneous Tissue)
The hypodermis is the innermost layer of the skin, primarily consisting of adipose tissue and loose connective tissue.
- Adipose Tissue:
Fat cells (adipocytes) in this layer store energy, provide insulation, and serve as a cushion for underlying muscles and organs. - Connective Tissue:
This layer anchors the skin to the underlying muscles and bones and contains larger blood vessels and nerves.
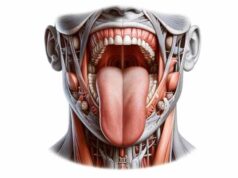
Vascular and Nervous Supply
The skin is highly vascularized and innervated:
- Blood Vessels:
A dense network of capillaries in the dermis ensures efficient delivery of oxygen and nutrients, while also playing a role in thermoregulation. - Nerve Endings:
A variety of sensory receptors detect touch, pressure, pain, and temperature. These include Meissner’s corpuscles for light touch, Pacinian corpuscles for deep pressure, and free nerve endings for pain and temperature.
Lymphatic System
The skin also has an extensive lymphatic network that helps maintain fluid balance and plays an essential role in immune defense.
Cellular Turnover and Regeneration
The skin undergoes continuous renewal:
- Keratinocyte Lifecycle:
New cells are generated in the stratum basale, migrate upward through the epidermis, become keratinized, and are eventually shed from the stratum corneum—a process that takes approximately 28 days. - Wound Healing:
The skin exhibits a robust healing process involving inflammation, tissue formation, and remodeling, with fibroblasts synthesizing collagen and extracellular matrix proteins.
Physiological Functions & Mechanisms
The skin performs a myriad of vital functions that are crucial for survival and overall well-being. Beyond serving as a physical barrier, it is an active organ involved in sensory perception, thermoregulation, metabolic processes, and immune defense.
Protective Barrier
- Physical Protection:
The skin’s multilayered structure, particularly the keratinized stratum corneum, serves as a formidable barrier against mechanical injuries, pathogens, chemicals, and ultraviolet (UV) radiation. - Immune Defense:
Langerhans cells and other immune components in the epidermis detect and respond to pathogens, while the lymphatic system aids in the removal of foreign particles and cellular debris. - UV Protection:
Melanin produced by melanocytes absorbs and dissipates UV radiation, protecting deeper tissues from damage and reducing the risk of skin cancer.
Sensory Functions
The skin is the primary organ of sensation:
- Touch and Pressure:
Mechanoreceptors such as Merkel cells and Meissner’s corpuscles enable the detection of light touch and pressure. - Pain and Temperature:
Nociceptors and thermoreceptors allow the skin to sense pain, heat, and cold, triggering protective reflexes. - Proprioception:
Though less pronounced in the skin compared to joints and muscles, sensory receptors help in the perception of the body’s position and movement.
Thermoregulation
The skin plays a critical role in regulating body temperature:
- Sweat Production:
Eccrine sweat glands secrete sweat, which evaporates and cools the body. - Vasodilation and Vasoconstriction:
Blood vessels in the dermis can expand or constrict to regulate heat loss. Vasodilation increases blood flow to the skin to release heat, while vasoconstriction reduces flow to conserve heat.
Metabolic Functions
- Vitamin D Synthesis:
The skin is essential for the synthesis of vitamin D. When exposed to UVB radiation, 7-dehydrocholesterol in the skin converts to vitamin D3, which is further processed in the liver and kidneys to its active form. - Excretion:
Through perspiration, the skin helps in the excretion of waste products, such as urea, salts, and toxins, thus contributing to detoxification.
Storage and Communication
- Energy Storage:
The hypodermis stores fat, which serves as an energy reserve and provides insulation. - Endocrine Functions:
The skin secretes various bioactive substances, including cytokines and hormones, which participate in local and systemic signaling.
Common Skin Conditions
The skin is prone to numerous disorders that can affect its appearance, function, and overall health. Below are some of the most common skin conditions, their causes, symptoms, and treatments.
Acne
Acne is a prevalent condition that primarily affects adolescents but can persist into adulthood.
- Causes:
Hormonal fluctuations lead to increased sebum production, combined with abnormal keratinization and bacterial overgrowth (Propionibacterium acnes). - Symptoms:
Clogged pores manifest as comedones (blackheads and whiteheads), along with inflammatory papules, pustules, nodules, and cysts. - Treatment:
Topical retinoids, benzoyl peroxide, and salicylic acid; oral antibiotics and hormonal treatments in severe cases; isotretinoin for recalcitrant acne.
Eczema (Atopic Dermatitis)
Eczema is a chronic inflammatory condition marked by itchy, red, and dry patches.
- Causes:
Genetic predisposition, immune dysregulation, and environmental triggers such as allergens and irritants. - Symptoms:
Itchy, inflamed, and scaly skin that may ooze or crust over, particularly on flexural areas. - Treatment:
Moisturizers, topical corticosteroids, antihistamines, and lifestyle adjustments to avoid triggers.
Psoriasis
Psoriasis is an autoimmune condition characterized by rapid skin cell turnover leading to thick, scaly plaques.
- Causes:
Genetic factors and immune system dysregulation. - Symptoms:
Red, inflamed patches with silvery scales, commonly on elbows, knees, scalp, and lower back; may be associated with joint pain in psoriatic arthritis. - Treatment:
Topical corticosteroids, vitamin D analogs, phototherapy, and systemic medications including biologics.
Rosacea
Rosacea is a chronic inflammatory disorder affecting the central face.
- Causes:
Genetic predisposition and environmental triggers such as heat, spicy foods, and alcohol. - Symptoms:
Persistent facial redness, visible blood vessels, papules, and pustules; ocular symptoms in some cases. - Treatment:
Topical metronidazole, azelaic acid, oral antibiotics, and laser therapy; avoidance of known triggers.
Skin Cancer
Skin cancer arises from abnormal growth of skin cells and includes basal cell carcinoma, squamous cell carcinoma, and melanoma.
- Causes:
Excessive UV exposure, genetic predisposition, and fair skin. - Symptoms:
New growths, changes in existing moles (irregular borders, color changes), non-healing sores, and lesions. - Treatment:
Surgical excision, radiation therapy, chemotherapy, and immunotherapy depending on the type and stage.
Vitiligo
Vitiligo is characterized by the loss of melanocytes, leading to white patches on the skin.
- Causes:
Autoimmune destruction of pigment cells, with possible genetic and environmental contributions. - Symptoms:
Depigmented patches, often on the face, hands, and other body parts. - Treatment:
Topical corticosteroids, calcineurin inhibitors, phototherapy, and, in some cases, surgical treatments.
Dermatitis
Dermatitis encompasses a group of inflammatory skin conditions.
- Contact Dermatitis:
Caused by exposure to allergens or irritants, resulting in a red, itchy rash. - Seborrheic Dermatitis:
A chronic form affecting areas with high sebaceous gland density, characterized by flaky, oily skin. - Treatment:
Topical corticosteroids, moisturizers, and avoidance of triggers.
Diagnostic Techniques & Assessments
Effective diagnosis of skin disorders requires a multifaceted approach combining clinical evaluation, imaging, laboratory tests, and sometimes invasive procedures. These methods help determine the underlying cause and guide appropriate treatment.
Clinical Evaluation
- Medical History:
A comprehensive history that details symptom onset, duration, triggers, family history, and prior treatments. - Physical Examination:
A thorough skin examination assessing lesion morphology, distribution, color, texture, and any associated symptoms such as itching or pain.
Dermatoscopy
- Technique:
Dermatoscopy uses a dermatoscope to magnify and illuminate skin lesions, allowing for enhanced visualization of patterns, colors, and structures that are not visible to the naked eye. - Applications:
Particularly useful in diagnosing pigmented lesions and differentiating benign moles from malignant melanoma.
Skin Biopsy
- Procedure:
A skin biopsy involves removing a small sample of skin tissue, which is then processed and examined under a microscope. - Types:
Punch, shave, or excisional biopsy techniques may be used depending on the lesion’s characteristics. - Histopathological Analysis:
This analysis provides definitive diagnosis by revealing cellular details, inflammatory patterns, and any malignant changes.
Patch Testing
- Procedure:
Small amounts of potential allergens are applied to the skin under adhesive patches for 48–72 hours. - Purpose:
Helps identify substances causing allergic contact dermatitis.
Laboratory Tests
- Blood Tests:
Evaluate markers of inflammation (ESR, CRP), complete blood count (CBC), and autoantibody profiles (ANA, anti-dsDNA) for systemic or autoimmune conditions. - Microbial Cultures:
Used to identify pathogens from skin swabs, particularly in suspected infections like impetigo or cellulitis.
Imaging Studies
- X-Rays and CT Scans:
Though not routine for primary skin conditions, these are useful for assessing deeper tissue involvement or metastasis in skin cancer. - MRI:
Offers detailed images of soft tissues and is employed in complex cases of invasive skin cancers. - Ultrasound:
High-frequency ultrasound is beneficial for evaluating cysts, abscesses, and the extent of lesions.
Advanced Techniques
- Reflectance Confocal Microscopy (RCM):
A non-invasive imaging method that provides high-resolution, real-time images of skin at the cellular level. - Optical Coherence Tomography (OCT):
Produces cross-sectional images of the skin, assisting in the evaluation of superficial and deeper layers for early signs of disease.
Functional and Sensory Testing
- Skin Prick Tests:
Used to diagnose immediate allergic reactions by introducing small quantities of allergens into the skin. - Phototesting:
Evaluates the skin’s reaction to UV exposure, particularly useful in diagnosing photosensitivity disorders.
Treatment Approaches & Therapies
Skin disorders are managed through a range of treatment modalities, from topical and systemic therapies to advanced procedural interventions. The choice of treatment is tailored to the specific condition, its severity, and the patient’s overall health.
Topical Treatments
Corticosteroids
- Usage:
Applied to reduce inflammation in conditions such as eczema, psoriasis, and contact dermatitis. - Considerations:
Available in various potencies; long-term use requires caution to avoid side effects like skin thinning.
Retinoids
- Usage:
Effective in treating acne, photoaging, and psoriasis by regulating cell turnover and reducing inflammation. - Types:
Includes tretinoin, adapalene, and tazarotene; typically applied at night to minimize irritation.
Antimicrobials
- Usage:
Topical antibiotics (e.g., clindamycin, erythromycin) are used to manage acne and minor skin infections. - Combination:
Often combined with benzoyl peroxide to enhance efficacy and mitigate resistance.
Emollients and Moisturizers
- Usage:
Essential for managing dry skin conditions like eczema, psoriasis, and vitiligo by restoring the skin barrier. - Ingredients:
Products containing ceramides, urea, or hyaluronic acid are particularly effective.
Calcineurin Inhibitors
- Usage:
Non-steroidal agents such as tacrolimus and pimecrolimus help manage atopic dermatitis without the side effects associated with prolonged steroid use.
Systemic Therapies
Oral Medications
- Antibiotics:
Systemic antibiotics (e.g., doxycycline) are used for moderate to severe acne and rosacea. - Retinoids:
Oral isotretinoin is reserved for severe, recalcitrant acne but requires close monitoring due to its side effects. - Immunosuppressants:
Agents such as methotrexate, cyclosporine, and azathioprine are used for severe psoriasis, eczema, and other autoimmune skin disorders. - Biologics:
Targeted therapies (e.g., TNF inhibitors, IL-17 inhibitors) are effective for moderate to severe psoriasis and atopic dermatitis.
Phototherapy
UV-B and PUVA
- Usage:
Phototherapy uses controlled UV light exposure to reduce inflammation and slow skin cell proliferation. UV-B is commonly used for psoriasis and eczema, while PUVA (psoralen plus UVA) is used for more severe conditions. - Benefits:
Provides a non-invasive treatment option with minimal systemic side effects.
Procedural and Surgical Treatments
Laser Therapy
- Applications:
Used to treat vascular lesions, pigmented lesions, acne scars, and for hair removal. Laser resurfacing also improves skin texture and tone. - Types:
CO₂ lasers, Nd:YAG lasers, and pulsed dye lasers are commonly used, depending on the condition.
Cryotherapy
- Usage:
Involves freezing lesions with liquid nitrogen to treat warts, actinic keratoses, and certain skin cancers. - Advantages:
A quick, outpatient procedure with minimal recovery time.
Excisional Surgery and Mohs Surgery
- Excisional Surgery:
Used to remove skin cancers and large benign lesions with a margin of normal tissue. - Mohs Surgery:
A precise, staged surgical technique that removes skin cancer layer by layer, ensuring complete excision while sparing healthy tissue.
Advanced Procedures
- Chemical Peels:
Apply acid solutions to exfoliate the skin, promoting regeneration and improving conditions like acne and hyperpigmentation. - Microneedling:
Creates micro-injuries in the skin to stimulate collagen production, aiding in the treatment of scars and wrinkles. - Platelet-Rich Plasma (PRP):
PRP injections use concentrated platelets from the patient’s blood to accelerate skin healing and rejuvenation.
Nutritional Support & Supplementation
Proper nutrition is integral to skin health, supporting cellular repair, immune function, and barrier integrity. Targeted supplementation can enhance skin appearance and aid in the treatment of various dermatological conditions.
Key Nutrients for Skin Health
- Vitamin C:
Essential for collagen synthesis, vitamin C also acts as a potent antioxidant that protects the skin from UV damage and pollution. - Vitamin E:
An antioxidant that supports the skin’s barrier function and helps reduce inflammation and oxidative stress. - Omega-3 Fatty Acids:
Found in fish oil and flaxseed oil, omega-3s reduce inflammation and support cell membrane integrity. - Zinc:
Critical for wound healing and immune function, zinc helps control inflammation and is particularly beneficial for acne. - Vitamin D:
In addition to its role in bone health, vitamin D supports immune regulation and may enhance skin repair. - B Vitamins:
Vitamins B6 and B12 are important for cellular energy production and the maintenance of healthy skin. - Biotin (Vitamin B7):
Supports healthy skin, hair, and nails, and aids in maintaining skin hydration.
Antioxidant Support
Antioxidants play a crucial role in protecting skin cells from oxidative damage:
- Selenium:
Works synergistically with vitamin E to combat free radicals. - Glutathione:
A master antioxidant that is vital for cellular detoxification and repair. - Green Tea Extract:
Rich in polyphenols, it offers powerful antioxidant and anti-inflammatory benefits that can help protect the skin from UV damage and premature aging.
Specialized Supplements
- Collagen Peptides:
Supplementing with collagen can improve skin elasticity, reduce wrinkles, and promote overall skin hydration. - Hyaluronic Acid:
Enhances moisture retention in the skin, improving skin plumpness and reducing fine lines. - Coenzyme Q-10 (CoQ10):
Supports cellular energy production and protects skin cells from oxidative damage. - Probiotics:
Maintaining a healthy gut microbiome is linked to improved skin health via the gut-skin axis, reducing inflammation and supporting barrier function.
Hydration and Electrolytes
- Water:
Adequate hydration is essential for maintaining skin moisture and facilitating the delivery of nutrients to skin cells. - Electrolytes:
Balanced electrolyte levels support cellular function and overall skin health, especially during physical activity or in hot climates.
Preventative Care & Healthy Practices
Prevention is key to maintaining healthy skin and preventing dermatological conditions. A combination of lifestyle modifications, regular skincare routines, and protective measures can significantly improve skin health over the long term.
Skincare and Personal Hygiene
- Daily Cleansing:
Use gentle cleansers suited to your skin type to remove impurities and excess oils without stripping the skin of natural moisture. - Moisturizing:
Apply moisturizers regularly to maintain skin hydration and strengthen the skin barrier. - Sun Protection:
Use broad-spectrum sunscreen with at least SPF 30 daily to protect against harmful UV radiation, which can cause premature aging and increase cancer risk. - Avoid Harsh Products:
Steer clear of products containing alcohol or other irritants that may damage the skin.
Diet and Hydration
- Balanced Nutrition:
A diet rich in fruits, vegetables, lean proteins, and whole grains supplies essential vitamins, minerals, and antioxidants for skin repair and regeneration. - Adequate Water Intake:
Drinking sufficient water throughout the day keeps the skin hydrated and supports overall cellular function.
Lifestyle Modifications
- Regular Exercise:
Physical activity improves circulation, which enhances nutrient delivery and waste removal in the skin. - Stress Management:
Chronic stress can impair skin health by triggering inflammatory pathways. Techniques like meditation, yoga, and deep breathing can mitigate these effects. - Sufficient Sleep:
Aim for 7–9 hours of quality sleep each night to allow the skin to repair and regenerate. - Avoid Smoking and Excessive Alcohol:
Both smoking and excessive alcohol consumption negatively impact skin health, accelerating aging and impairing repair mechanisms.
Regular Health Monitoring
- Skin Self-Exams:
Perform regular self-examinations to identify new or changing lesions early. Look for asymmetry, irregular borders, color changes, and evolving size. - Dermatological Check-Ups:
Annual professional skin evaluations can help detect conditions like skin cancer, psoriasis, and eczema in their early stages. - Manage Chronic Conditions:
Conditions such as diabetes and autoimmune disorders can affect skin health. Regular monitoring and management of these conditions are essential.
Trusted Resources & Further Reading
For additional information and ongoing updates in skin health, consider these trusted resources that offer comprehensive insights and research-backed guidance:
Books
- “The Skin Type Solution” by Leslie Baumann:
Offers personalized skincare routines and insights into managing different skin types. - “The Clear Skin Diet” by Alan C. Logan and Valori Treloar:
Explores the link between nutrition and skin health, providing actionable dietary recommendations for clearer skin. - “Skin Rules: Trade Secrets from a Top New York Dermatologist” by Debra Jaliman:
A practical guide from a leading dermatologist, covering effective skincare strategies and anti-aging tips.
Academic Journals
- Journal of Investigative Dermatology:
Publishes high-quality research on skin biology, diseases, and emerging treatments. - British Journal of Dermatology:
Features comprehensive clinical and experimental research articles on dermatological conditions. - Dermatologic Clinics:
Provides review articles and clinical insights on various skin disorders and treatment approaches.
Mobile Apps
- WebMD:
A widely used app offering detailed information on skin conditions, treatments, and expert advice. - SkinVision:
An app designed to help users monitor skin lesions and detect early signs of skin cancer. - MySkin:
Provides personalized skincare recommendations based on your skin type and concerns.
Frequently Asked Questions on Skin
What are the primary functions of the skin?
The skin serves as a protective barrier, regulates body temperature, facilitates sensory perception, supports metabolic functions such as vitamin D synthesis, and plays a role in excretion and immune defense.
How does the skin protect against UV radiation?
Melanocytes in the epidermis produce melanin, which absorbs and disperses UV radiation, thereby protecting deeper skin layers from damage and reducing the risk of skin cancer.
What causes common skin conditions like acne and eczema?
Acne is primarily caused by excessive sebum production, clogged pores, and bacterial colonization, while eczema is linked to genetic predisposition, immune dysfunction, and environmental triggers.
How are skin cancers typically treated?
Treatment options for skin cancer include surgical excision, Mohs micrographic surgery, radiation therapy, and, in advanced cases, systemic therapies such as chemotherapy and immunotherapy.
What lifestyle changes can support long-term skin health?
Maintaining a balanced diet, staying hydrated, using sun protection, practicing good skincare, managing stress, and avoiding smoking and excessive alcohol are key strategies to promote healthy skin.
Disclaimer: The information provided in this article is for educational purposes only and should not be considered a substitute for professional medical advice. Always consult a healthcare provider for any concerns regarding your health.
Please share this article on Facebook, X (formerly Twitter), or your preferred social media platform to help spread awareness about skin health and the latest treatment strategies.