The spleen is a remarkable organ with multifaceted roles in the human body. Acting as a critical filter of blood and an essential component of the immune system, the spleen not only stores and recycles blood cells but also combats infections and helps regulate blood volume. Encased in a fibrous capsule and strategically positioned in the left upper quadrant of the abdomen, this fist-sized organ plays a pivotal part in maintaining overall health and homeostasis. Whether you’re exploring its anatomical intricacies, understanding its diverse functions, or learning about conditions that affect it, this comprehensive guide offers expert insights and practical tips for optimal spleen health.
Table of Contents
- Spleen Architecture & Framework
- Immune Filtration & Blood Processing
- Hematopoiesis & Blood Reservoir
- Lymphatic & Neural Integration
- Development, Variations, & Anomalies
- Functional Dynamics & Roles
- Spleen Disorders & Conditions
- Diagnostic Approaches
- Therapeutic Interventions
- Nutritional & Supplementary Support
- Lifestyle & Wellness Practices
- Trusted Resources
- Frequently Asked Questions
- Disclaimer & Sharing
Spleen Architecture & Framework
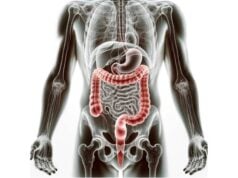
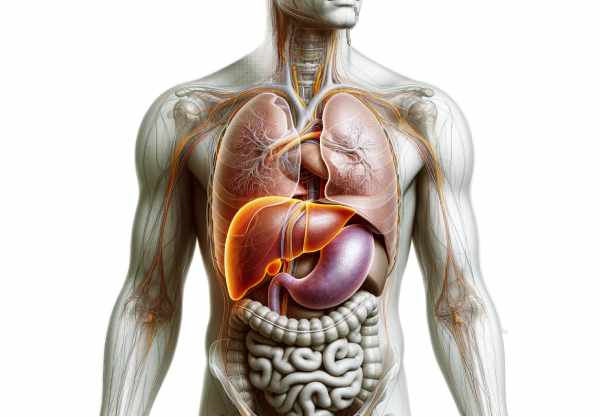
The spleen is a dark purple, fist-sized organ weighing roughly 150 grams in adults. Its structure is distinctly divided into two major components: the white pulp and the red pulp, each with its own specialized functions. Encased in a dense, fibrous capsule, the spleen’s structural integrity is maintained by trabeculae—connective tissue strands that extend inward and form a supportive network. These trabeculae not only help preserve the spleen’s shape but also compartmentalize its internal regions, ensuring that the immune cells and blood filtration mechanisms operate effectively and in harmony.
Capsule and Trabeculae
- Capsule:
The spleen is enveloped in a robust, fibrous capsule that provides mechanical support and protection. This outer layer shields the delicate internal structures from physical trauma. - Trabeculae:
Extending from the capsule into the parenchyma, the trabeculae are bands of connective tissue that subdivide the spleen into lobules. They serve as conduits for blood vessels and nerves, ensuring an organized distribution of blood flow and facilitating communication among splenic cells.
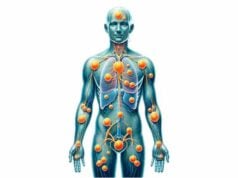
White Pulp
The white pulp constitutes the immunologically active regions of the spleen. It consists primarily of lymphoid tissue arranged around central arterioles, forming structures known as periarteriolar lymphoid sheaths (PALS). Within these sheaths, T lymphocytes are the predominant cell type. Surrounding the PALS are lymphoid follicles, densely populated by B lymphocytes. These structures are crucial for mounting immune responses, as they facilitate the activation, proliferation, and maturation of lymphocytes. Upon encountering antigens, the white pulp initiates the production of antibodies, thereby playing a central role in defending the body against infections.
Red Pulp
The red pulp is the site for blood filtration and storage within the spleen. It is characterized by a network of sinusoids—irregular, blood-filled spaces lined with specialized endothelial cells and macrophages. As blood slowly percolates through these sinusoids, old or damaged red blood cells are identified and removed through phagocytosis. The red pulp also serves as a reservoir for blood cells and platelets. During times of hemorrhage or increased physiological demand, the spleen can contract to release stored blood, thus aiding in the maintenance of blood volume and pressure.
Marginal Zone
Positioned at the interface between the white and red pulp, the marginal zone is a critical region for initiating immune responses. It is rich in macrophages, dendritic cells, and lymphocytes. The marginal zone acts as a first line of defense by capturing blood-borne antigens and presenting them to the lymphocytes in the white pulp, triggering a rapid and effective immune response.
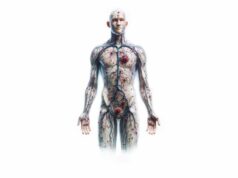
Blood Supply
The spleen receives its blood supply primarily through the splenic artery, which is a major branch of the celiac trunk. Upon entering the spleen at the hilum—a concave area on its surface—the splenic artery divides into smaller arterioles that penetrate deep into the organ. These arterioles eventually lead to the sinusoids in the red pulp, where the essential process of blood filtration occurs. Venous blood is then collected by the splenic veins, which converge to form the portal vein, integrating the spleen’s function with the liver and systemic circulation.
Immune Filtration & Blood Processing
The spleen plays an indispensable role in the body’s immune defense and blood maintenance. Through its dual functions of immune surveillance and blood filtration, the spleen ensures that the bloodstream remains free of pathogens and damaged cells.
Immune Response Activation
- Antigen Detection:
As blood circulates through the spleen, it is continuously scanned by immune cells. Macrophages and dendritic cells in the white pulp detect and capture pathogens, foreign particles, and abnormal cells. - Lymphocyte Activation:
Once antigens are captured, they are presented to T and B lymphocytes. This antigen presentation triggers the proliferation and activation of lymphocytes, leading to the production of antibodies and the generation of cytotoxic responses that eliminate the threat. - Adaptive Immunity:
The spleen is integral to the development of adaptive immunity. The lymphoid follicles within the white pulp facilitate the maturation of B cells, which then produce specific antibodies tailored to the encountered pathogens.
Blood Filtration Mechanisms
- Removal of Old Red Blood Cells:
In the red pulp, the spleen meticulously filters the blood to remove senescent or damaged red blood cells. Macrophages in the red pulp engulf and digest these cells, recycling valuable components such as iron for future red blood cell production. - Clearance of Debris and Pathogens:
The slow flow of blood through the sinusoids ensures that pathogens and cellular debris are efficiently captured by macrophages. This process is critical in preventing systemic infections and maintaining the overall health of the circulatory system. - Maintenance of Blood Quality:
By ensuring that only healthy red blood cells remain in circulation, the spleen contributes significantly to optimal oxygen delivery throughout the body. Additionally, it stores platelets and other blood components, releasing them when needed during emergencies.
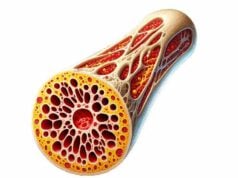
Hematopoiesis & Blood Reservoir
Although the bone marrow is the primary site of blood cell production in adults, the spleen retains the remarkable ability to produce blood cells under certain circumstances—a function known as extramedullary hematopoiesis. Additionally, the spleen serves as a vital reservoir for blood cells, playing a crucial role during times of increased demand.
Extramedullary Hematopoiesis
- Fetal Development:
During fetal development, the spleen is a major site for hematopoiesis, producing red and white blood cells. After birth, this function diminishes as the bone marrow takes over. However, under pathological conditions such as severe anemia or bone marrow failure, the spleen can reactivate its hematopoietic capabilities. - Clinical Significance:
Extramedullary hematopoiesis in the spleen may be seen in disorders like myelofibrosis or hemolytic anemias. Although this adaptive response can help compensate for insufficient bone marrow activity, it may also lead to splenomegaly and further complications.
Blood Reservoir Function
- Storage of Blood Components:
The spleen stores a substantial reserve of red blood cells and platelets. This reservoir function is critical during acute blood loss, as the spleen can contract to release stored blood, thus stabilizing blood pressure and volume. - Response to Physiological Stress:
During vigorous physical activity or injury, the spleen’s ability to release its stored blood becomes particularly important. This rapid response helps maintain oxygen delivery and supports overall cardiovascular function. - Regulation of Circulatory Homeostasis:
By acting as a buffer for blood volume fluctuations, the spleen ensures that the circulatory system operates efficiently, particularly during episodes of hemorrhage or shock.
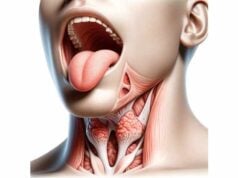
Lymphatic & Neural Integration
Beyond its roles in immune surveillance and blood processing, the spleen is intricately connected to both the lymphatic and nervous systems. These connections allow the spleen to coordinate immune responses and maintain optimal internal communication.
Lymphatic Connections
- Lymphatic Vessels:
The spleen is a central hub in the lymphatic system, interconnected with a network of lymphatic vessels that transport lymph—a clear fluid rich in immune cells—throughout the body. - Immune Cell Trafficking:
These vessels facilitate the movement of lymphocytes and other immune cells to and from the spleen. This trafficking is essential for mounting an effective immune response and for the circulation of immune surveillance cells.
Neural Innervation
- Autonomic Nervous System:
The spleen receives both sympathetic and parasympathetic innervation. The celiac plexus, a key component of the sympathetic nervous system, provides innervation that regulates splenic contraction, influencing blood release and immune modulation. - Functional Implications:
Although parasympathetic fibers are less prominent, they contribute to the overall regulation of splenic immune responses. This dual innervation ensures that the spleen can rapidly adjust its functions in response to physiological changes and stress.
Development, Variations, & Anomalies
The spleen’s development and anatomical variations provide important insights into its function and potential clinical implications. Understanding these aspects is essential for diagnosing congenital anomalies and variations that may affect spleen performance.
Embryological Development
- Origin:
The spleen develops from mesenchymal cells in the dorsal mesogastrium during the fifth week of embryonic life. Its early formation is critical to the establishment of the body’s immune framework. - Hematopoietic Role:
By the third month of fetal development, the spleen actively participates in hematopoiesis, producing red and white blood cells. This function diminishes postnatally, but the spleen retains the latent ability to resume blood cell production under stress.
Anatomical Variations
- Accessory Spleens:
Small, additional splenic tissues known as accessory spleens can be found near the main spleen or elsewhere in the abdominal cavity. Although generally benign and asymptomatic, they may become clinically significant in certain conditions, such as when the main spleen is removed. - Congenital Asplenia:
This rare condition is characterized by the complete absence of the spleen from birth, leading to significant immunological vulnerabilities. Patients with congenital asplenia require careful management to prevent life-threatening infections. - Hyposplenism:
A reduction in splenic function, often resulting from conditions like sickle cell disease, can lead to hyposplenism. This diminished function compromises the spleen’s ability to filter blood and mount effective immune responses.
Functional Dynamics & Roles of the Spleen
The spleen’s diverse functions are central to maintaining immune competence and circulatory stability. This section explores how the spleen’s activities contribute to the body’s overall health.
Immune Surveillance and Response
- Pathogen Detection:
As blood courses through the spleen, immune cells continuously scan for pathogens. Macrophages, dendritic cells, and lymphocytes work in concert to detect and neutralize invading organisms. - Activation of Lymphocytes:
Once antigens are identified, lymphocytes within the white pulp are activated. B lymphocytes produce antibodies, while T lymphocytes orchestrate cell-mediated responses that are vital for eliminating infections. - Rapid Immune Reaction:
The marginal zone serves as an immediate response zone, ensuring that blood-borne pathogens are swiftly captured and presented to immune cells. This rapid reaction is essential for preventing the systemic spread of infections.
Blood Filtration and Quality Control
- Red Blood Cell Recycling:
The red pulp functions as a filter that removes old or deformed red blood cells. Macrophages break down these cells, salvaging valuable components like iron for future use. - Clearance of Cellular Debris:
In addition to aging blood cells, the spleen efficiently eliminates cellular debris and pathogens, thereby ensuring that only healthy components circulate in the bloodstream. - Platelet Storage:
The spleen also acts as a reservoir for platelets, releasing them during acute blood loss or increased physiological demand, which aids in clot formation and hemostasis.
Iron Metabolism
- Recycling Process:
The breakdown of red blood cells in the red pulp releases hemoglobin, which is then degraded into its constituent parts. Iron is stored within splenic macrophages as ferritin or hemosiderin, making it available for the synthesis of new red blood cells in the bone marrow. - Metabolic Balance:
By recycling iron, the spleen contributes to the overall balance of essential nutrients, ensuring efficient erythropoiesis and optimal oxygen delivery throughout the body.
Spleen Disorders & Conditions
Despite its resilience, the spleen is susceptible to a variety of disorders that can compromise its function. Understanding these conditions is critical for prompt diagnosis and effective management.
Splenomegaly
Splenomegaly refers to an abnormally enlarged spleen, which can occur as a response to infection, liver disease, hematologic disorders, or autoimmune conditions.
- Infectious Causes:
Viral infections (e.g., mononucleosis), bacterial infections (e.g., syphilis), and parasitic diseases (e.g., malaria) can lead to splenic enlargement. - Liver and Portal Hypertension:
Chronic liver diseases like cirrhosis cause increased pressure in the portal venous system, resulting in blood pooling within the spleen. - Hematologic & Autoimmune Disorders:
Conditions such as leukemia, lymphoma, rheumatoid arthritis, and lupus often provoke splenomegaly due to increased immune activity and abnormal blood cell proliferation.
Hypersplenism
Hypersplenism is characterized by an overactive spleen that excessively destroys blood cells, leading to cytopenias such as anemia, leukopenia, and thrombocytopenia.
- Primary vs. Secondary:
Primary hypersplenism occurs without a clear underlying cause, whereas secondary hypersplenism is often linked to conditions like chronic liver disease or hematologic malignancies.
Asplenia and Hyposplenism
- Asplenia:
The absence of a spleen, whether congenital or acquired (post-splenectomy), significantly impairs immune function and increases susceptibility to severe infections. - Hyposplenism:
Partial loss of splenic function, as seen in conditions like sickle cell disease, compromises the organ’s ability to filter blood and mount an adequate immune response.
Splenic Rupture
A splenic rupture is a life-threatening condition that results from trauma or pathological weakening of the splenic capsule. It causes internal bleeding and requires immediate medical intervention.
- Causes & Symptoms:
Trauma from accidents or sports injuries, as well as conditions like infectious mononucleosis, can precipitate rupture. Symptoms include sudden left upper quadrant pain, dizziness, and signs of shock.
Splenic Cysts and Tumors
- Splenic Cysts:
Fluid-filled sacs that may be congenital or acquired through infection or trauma. While often asymptomatic, large cysts can cause discomfort and may require surgical intervention. - Splenic Tumors:
Tumors may be benign (such as hemangiomas) or malignant (such as lymphoma or metastatic cancer). Their presence can disrupt normal splenic function and lead to systemic symptoms.
Splenic Infarction
Splenic infarction occurs when the blood supply to a region of the spleen is interrupted, leading to tissue necrosis.
- Etiology:
Common causes include blood clots, embolism, and conditions like sickle cell disease. - Clinical Presentation:
Patients may experience acute left upper quadrant pain, fever, and signs of systemic inflammation.
Autoimmune and Inflammatory Disorders
Conditions like sarcoidosis and systemic lupus erythematosus (SLE) can involve the spleen, leading to enlargement, dysfunction, or both, as the immune system mistakenly attacks healthy splenic tissue.
Hemolytic Anemia
In hemolytic anemias, the spleen plays a major role in destroying abnormal red blood cells. Conditions such as hereditary spherocytosis or autoimmune hemolytic anemia may cause the spleen to enlarge and become overactive, contributing to anemia and other complications.
Diagnostic Approaches for Spleen Health
Accurate diagnosis of spleen-related conditions requires a comprehensive evaluation that integrates clinical examination with advanced imaging and laboratory tests. This multidisciplinary approach ensures that underlying issues are correctly identified and managed.
Clinical Examination
- Physical Assessment:
During a physical exam, healthcare providers palpate the left upper quadrant of the abdomen to detect splenomegaly. Percussion techniques help estimate spleen size and density, providing initial clues about potential abnormalities. - Medical History:
A detailed medical history, including recent infections, trauma, and chronic conditions, is essential to contextualize the patient’s symptoms and guide further diagnostic steps.
Imaging Studies
- Ultrasound:
Ultrasound is a first-line, non-invasive imaging modality used to assess spleen size, detect cysts or tumors, and evaluate blood flow. Its real-time imaging capabilities and safety profile make it an ideal tool for initial screening. - Computed Tomography (CT) Scan:
CT scans offer high-resolution, cross-sectional images that can reveal detailed anatomical structures. They are especially useful in detecting splenic injuries, tumors, and complex cystic formations. - Magnetic Resonance Imaging (MRI):
MRI provides detailed soft tissue contrast, which is particularly valuable in distinguishing between benign and malignant lesions and assessing vascular involvement.
Laboratory Tests
- Complete Blood Count (CBC):
A CBC evaluates the levels of red blood cells, white blood cells, and platelets. Abnormalities in these counts may indicate hypersplenism, hemolytic anemias, or underlying infections. - Peripheral Blood Smear:
This test allows for the microscopic examination of blood cells, which can help detect abnormal cell morphology related to hemolytic disorders. - Liver Function Tests:
Since liver diseases often affect the spleen via portal hypertension, liver function tests are useful for diagnosing conditions that may contribute to splenomegaly. - Autoimmune Panels:
Tests for specific antibodies can help diagnose autoimmune disorders like SLE that may impact splenic function.
Biopsy Procedures
- Fine Needle Aspiration (FNA):
FNA involves extracting a small sample of splenic tissue or fluid for cytological examination. It is minimally invasive and helps diagnose infections, cysts, or tumors. - Core Needle Biopsy:
When a more substantial tissue sample is needed, a core needle biopsy may be performed to obtain a representative specimen for histopathological analysis.
Nuclear Medicine and Functional Imaging
- Spleen Scans:
Nuclear medicine techniques, such as Technetium-99m sulfur colloid scans, assess the functional capacity of the spleen. These scans help evaluate splenic blood flow, detect infarctions, and identify functional asplenia. - Positron Emission Tomography (PET):
In cases of suspected malignancy, PET scans can identify areas of increased metabolic activity within the spleen, aiding in the diagnosis of cancers.
Endoscopic and Invasive Assessments
- Endoscopic Ultrasound (EUS):
EUS combines endoscopy with ultrasound imaging, providing detailed views of the spleen and adjacent structures. This technique is useful for evaluating splenic lesions and guiding biopsy procedures. - Diagnostic Laparoscopy:
In select cases, laparoscopy may be used to visually inspect the spleen and obtain tissue samples, offering direct insight into splenic pathology.
Therapeutic Interventions & Management
The treatment of spleen-related conditions is highly individualized, depending on the underlying cause, severity of symptoms, and the patient’s overall health status. Management strategies span from conservative medical therapies to advanced surgical interventions.
Medical Management
- Antibiotics and Antivirals:
Infections that lead to splenic complications, such as splenomegaly or abscess formation, are managed with appropriate antimicrobial therapies. The choice of antibiotic or antiviral agent depends on the identified pathogen. - Immunosuppressants:
Autoimmune conditions affecting the spleen, such as SLE or rheumatoid arthritis, may be treated with immunosuppressive medications to reduce inflammatory activity. - Chemotherapy and Targeted Agents:
Hematologic malignancies that involve the spleen, like lymphomas, are managed with systemic chemotherapy or targeted therapies designed to attack cancer cells while minimizing side effects.
Surgical Options
- Splenectomy:
Surgical removal of the spleen is indicated in cases of traumatic rupture, refractory hypersplenism, certain cancers, or when the spleen is significantly enlarged and symptomatic. Post-splenectomy patients require special precautions, including vaccinations and prophylactic antibiotics, to mitigate infection risk. - Partial Splenectomy:
When feasible, partial splenectomy aims to remove only the diseased portion of the spleen, preserving some splenic function while alleviating symptoms. - Minimally Invasive Techniques:
Laparoscopic splenectomy offers a less invasive alternative to open surgery, resulting in reduced postoperative pain, shorter hospital stays, and faster recovery.
Interventional Radiology
- Embolization:
Splenic artery embolization is used to control bleeding in traumatic injuries or to reduce splenic size in cases of hypersplenism. This procedure involves the targeted occlusion of blood vessels feeding the affected areas, thereby decreasing blood flow and reducing symptoms. - Image-Guided Drainage:
For splenic abscesses or cysts, percutaneous drainage under imaging guidance can be an effective minimally invasive treatment.
Innovative Therapies
- Stem Cell and Regenerative Therapies:
Although still in experimental stages, stem cell therapy holds promise for regenerating damaged splenic tissue and restoring immune function. - Gene Therapy:
Research into gene therapy aims to correct genetic defects associated with congenital splenic disorders, potentially restoring normal splenic function in conditions like hereditary spherocytosis. - Biologic Agents:
The development of biologics, which target specific immune pathways, is transforming the management of autoimmune disorders that affect the spleen, offering more precise treatments with fewer systemic side effects.
Nutritional & Supplementary Support for Spleen Health
Proper nutrition and targeted supplementation play an essential role in maintaining spleen health. By providing the body with vital nutrients and antioxidants, these interventions support the spleen’s immune and filtration functions, and help mitigate inflammation.
Vitamins and Minerals
- Vitamin C:
An essential antioxidant that bolsters immune function and aids in the repair of tissues. Vitamin C supports the production of white blood cells and enhances the spleen’s ability to combat infections. - Vitamin B12:
Critical for red blood cell production and nerve health, Vitamin B12 helps prevent anemia—a condition that can overburden the spleen. - Iron:
Iron is fundamental to the production of hemoglobin. Supplementation may be necessary to prevent iron deficiency anemia, thereby reducing the spleen’s workload in filtering defective red blood cells. - Vitamin D:
Beyond its role in bone health, Vitamin D modulates immune responses and may reduce inflammation, benefiting overall splenic function.
Herbal Supplements
- Astragalus:
Known for its immune-enhancing properties, astragalus supports the spleen by stimulating white blood cell production and fortifying the body’s defense mechanisms. - Echinacea:
This herb boosts the immune system and has been shown to help reduce the incidence and duration of infections, indirectly supporting spleen health. - Milk Thistle:
Rich in silymarin, milk thistle protects the liver, which is closely linked to splenic function. By reducing the liver’s detoxification burden, it indirectly benefits the spleen.
Antioxidants
- Resveratrol:
Found in grapes and berries, resveratrol combats oxidative stress and inflammation, protecting splenic cells from damage. - Green Tea Extract:
High in catechins, green tea extract provides potent antioxidant and anti-inflammatory effects, which support overall immune function and spleen health.
Enzymes and Other Compounds
- Bromelain:
Derived from pineapple, bromelain aids digestion and reduces inflammation. Its anti-inflammatory properties can ease the spleen’s workload by promoting efficient nutrient absorption. - Acetyl-L-Carnitine:
Known for its role in energy metabolism, acetyl-L-carnitine supports cellular repair and nerve function, which may benefit overall immune competence. - L-Theanine:
This amino acid, commonly found in green tea, promotes relaxation and reduces stress—both factors that contribute to better immune regulation and splenic health.
Lifestyle & Wellness Practices for Spleen Optimization
Maintaining spleen health extends beyond medical treatments and nutritional support—it requires a holistic approach to lifestyle. Adopting healthy habits can significantly reduce the risk of spleen-related disorders and enhance overall immune function.
Dietary Habits
- Balanced Diet:
Consume a variety of fruits, vegetables, lean proteins, and whole grains to ensure you receive an abundance of essential vitamins, minerals, and antioxidants. - Hydration:
Drinking sufficient water is crucial for maintaining blood volume and facilitating efficient nutrient transport. Aim for at least eight cups of water daily. - Limit Processed Foods:
Minimizing intake of processed and high-sugar foods can reduce inflammation and support a healthier immune system.
Physical Activity
- Regular Exercise:
Engage in moderate-intensity exercise such as walking, swimming, or yoga. Regular physical activity promotes circulation, enhances immune responses, and reduces the risk of chronic diseases that can indirectly affect the spleen. - Weight Management:
Maintaining a healthy weight is vital in preventing fatty liver disease and other metabolic conditions that can impair splenic function.
Stress Management
- Mindfulness and Meditation:
Regular practice of mindfulness, meditation, or deep breathing exercises can reduce stress and support the immune system. - Adequate Sleep:
Aim for 7–9 hours of quality sleep per night to allow your body, including the spleen, to repair and regenerate. - Avoid Smoking and Limit Alcohol:
Smoking and excessive alcohol consumption can impair blood flow and immune function. Reducing or eliminating these habits contributes to overall splenic health.
Preventative Care
- Regular Check-Ups:
Routine medical examinations help detect early signs of splenic or systemic disorders. Early intervention can prevent complications. - Vaccinations:
Staying current with vaccinations is essential, particularly for individuals with compromised splenic function, as they are more vulnerable to infections. - Injury Prevention:
Use ergonomic practices and protective gear during physical activities to prevent abdominal trauma that could injure the spleen.
Trusted Resources for Spleen Health
For further learning and reliable information on spleen health, consider these reputable resources. They provide evidence-based research, clinical insights, and practical advice for both patients and healthcare professionals.
Books
- “The Spleen and Its Diseases: Clinical and Pathological Perspectives” by Dr. William F. Frable
This comprehensive guide offers in-depth insights into spleen anatomy, pathology, and management strategies. - “Spleen: Pathophysiology and Clinical Aspects” by Dr. Anthony R. Turner
An authoritative resource that explores spleen functions, disorders, and therapeutic approaches. - “Immunology and the Spleen” by Dr. Patricia C. Fox
This book delves into the immunological roles of the spleen, emphasizing its significance in maintaining overall health.
Academic Journals
- The Journal of Clinical Investigation
Featuring cutting-edge research articles on immune function and spleen-related studies, this journal is an invaluable resource for current developments. - Blood
A premier journal in hematology, it publishes peer-reviewed studies on blood disorders and spleen function, providing insights into diagnostic and therapeutic innovations.
Mobile Applications
- MySpleen Health:
An app designed to help users track spleen-related symptoms, manage medications, and schedule medical appointments. - Spleen Check:
Offers tools for monitoring spleen size and function, along with educational resources about common splenic conditions. - Health eSpleen:
Provides comprehensive information on spleen health, preventive care tips, and a symptom tracker to assist in managing splenic disorders.
Frequently Asked Questions
What is the primary function of the spleen?
The spleen plays a crucial role in filtering blood, removing old or damaged red blood cells, and mounting immune responses by producing and activating lymphocytes. It also acts as a blood reservoir, releasing stored blood when needed.
How does the spleen contribute to immune function?
By housing white pulp rich in lymphocytes and macrophages, the spleen detects pathogens in the bloodstream, activates an immune response, and produces antibodies, making it essential for defending against infections.
What causes an enlarged spleen (splenomegaly)?
Splenomegaly can result from infections, liver diseases, hematologic disorders, or autoimmune conditions. It occurs when the spleen works harder to filter blood or due to abnormal blood cell proliferation.
How is splenic function assessed diagnostically?
Spleen function is evaluated using physical exams, imaging studies (ultrasound, CT, MRI), laboratory tests (CBC, liver function tests), and sometimes biopsies to identify structural or functional abnormalities.
What lifestyle changes support a healthy spleen?
Maintaining a balanced diet, staying hydrated, exercising regularly, managing stress, getting adequate sleep, avoiding smoking and excessive alcohol, and having routine check-ups are essential for preserving spleen health.
Disclaimer & Sharing
The information provided in this article is for educational purposes only and is not a substitute for professional medical advice. Always consult with a qualified healthcare provider for any concerns or before starting any new treatment.
If you found this guide helpful, please share it on Facebook, X (formerly Twitter), or your preferred social platform to help spread awareness and promote spleen health.