Superior Oblique Myokymia (SOM) is a rare and usually harmless ocular condition characterized by spontaneous, involuntary, and episodic contractions or twitching of the superior oblique muscle, which is one of the extraocular muscles that control eye movement. The superior oblique muscle controls the downward and inward movement of the eye, and when it contracts involuntarily, it can cause a variety of visual disturbances that are distressing and disorienting for the affected person.
Structure and Function of the Superior Oblique Muscle
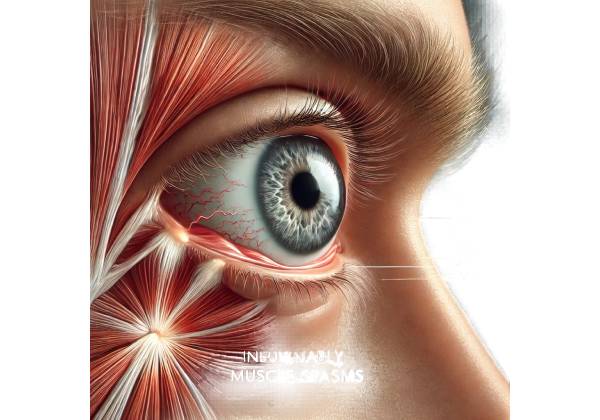
To understand Superior Oblique Myokymia, you must first understand the anatomy and function of the superior oblique muscle. The extraocular muscles are a collection of six muscles that regulate eye movement. These muscles are the medial rectus, lateral rectus, superior rectus, inferior rectus, superior obliques, and inferior obliques. The superior oblique muscle originates near the back of the orbit, moves forward, and passes through the trochlea, a small cartilaginous loop that functions as a pulley. After passing through the trochlea, the muscle attaches to the top of the eye.
The superior oblique muscle plays a unique role in regulating eye movement. It controls intorsion (rotation of the top of the eye toward the nose), depression (downward movement of the eye), and abduction. When the superior oblique muscle is working properly, these movements are smooth and coordinated, allowing the eye to track objects precisely and maintain stable vision.
Pathophysiology of Superior Oblique Myokymia
Superior Oblique Myokymia causes the affected muscle to contract spontaneously and repeatedly, often described as twitching or flickering. These contractions are usually unilateral, affecting only one eye, and last only a few seconds or minutes. The exact cause of these involuntary contractions is unknown, but they are thought to be caused by abnormal discharges in the trochlear nerve (cranial nerve IV), which supplies the superior oblique muscle. These abnormal discharges cause muscle hyperactivity, resulting in irregular contractions.
The pathophysiology of SOM may involve a number of factors, including:
- Neurovascular Compression: One theory proposes that SOM is caused by neurovascular compression, in which an artery or vein compresses the trochlear nerve. This compression may irritate the nerve, resulting in abnormal electrical discharges and subsequent muscle contractions. Neurovascular compression is a known cause of other cranial nerve hyperactivity disorders, including trigeminal neuralgia and hemifacial spasm, and it may also contribute to SOM.
- Microvascular Ischemia: Microvascular ischemia is another possible mechanism in which small blood vessels supplying the trochlear nerve become clogged, resulting in localized nerve damage and dysfunction. This ischemia can cause the nerve to fire intermittently and spontaneously, causing muscle contraction.
- Demyelinating Conditions: SOM has been linked to demyelinating conditions like multiple sclerosis (MS), in which the protective myelin sheath around nerves is damaged. This damage can cause abnormal nerve impulse conduction, which may contribute to the development of SOM.
- Idiopathic Causes: In many cases, the exact cause of SOM remains unknown, indicating that no specific underlying cause can be identified. The condition can develop spontaneously without a clear cause, and it is commonly classified as a primary muscle hyperactivity disorder.
Symptoms Of Superior Oblique Myokymia
Superior Oblique Myokymia symptoms can vary in severity and frequency, but they usually include visual disturbances that occur during muscle contractions. These symptoms can be intermittent, with periods of normal vision in between episodes, or more frequent, interfering with the patient’s daily activities. Common symptoms include:
- Monocular Oscillopsia: One of the most distinguishing symptoms of SOM is monocular oscillopsia, a sensation in which objects in the visual field appear to move or oscillate. The rapid, involuntary movements of the affected eye cause this phenomenon, which causes the perception of motion in stationary objects. Oscillopsia can be especially distressing for patients because it causes visual instability and difficulty focusing on objects.
- Diplopia (Double Vision): During episodes of SOM, irregular contractions of the superior oblique muscle can cause eye misalignment, resulting in double vision or diplopia. Diplopia occurs when the brain receives conflicting images from each eye, resulting in the perception of two overlapping images rather than one. The double vision associated with SOM is usually transient and disappears when the episode ends.
- Torsional Movements: Patients with SOM may experience torsional eye movements, which occur when the top of the affected eye rotates inward or outwards. This can cause visual distortion and discomfort because the visual field appears tilted or skewed.
- Eye Pain or Discomfort: Some people with SOM have reported mild eye pain or discomfort during muscle contractions. This pain is rarely severe, but it can be bothersome, especially if it occurs frequently.
- Head Tilt: To compensate for the visual disturbances caused by SOM, some patients may use a compensatory head tilt, which positions their head in a way that reduces the impact of abnormal eye movements. This head tilt is usually directed away from the affected eye, which helps to alleviate symptoms such as diplopia and oscillopsia.
- Visual Fatigue: The constant adjustment required to cope with SOM’s visual disturbances can cause visual fatigue, especially when performing tasks that require sustained focus, such as reading or driving. Patients may notice that their symptoms worsen when they perform long-term visual tasks or are required to concentrate visually.
Effects on Quality of Life
Superior Oblique Myokymia is rarely associated with serious long-term complications, but it can have a significant impact on a patient’s quality of life. The episodic nature of the symptoms can be unpredictable and disruptive, making it difficult for patients to carry out daily tasks or maintain normal visual function. SOM-induced visual disturbances, such as oscillopsia and diplopia, can make it difficult to perform tasks requiring precise vision, such as reading, writing, driving, or working with detailed objects.
In addition to physical symptoms, the condition may have psychological consequences. Some patients may experience anxiety or frustration as a result of the episodes’ unpredictable nature, as well as the discomfort and visual instability they cause. Social interactions may also be impacted, as the symptoms may be visible to others, causing self-consciousness or embarrassment.
Differential Diagnosis
When diagnosing Superior Oblique Myokymia, it is critical to consider other conditions that may exhibit similar symptoms. The differential diagnosis for SOM includes the following:
- Benign Essential Blepharospasm: This condition causes involuntary contractions of the eyelid muscles, resulting in twitching or blinking. Unlike SOM, which affects the superior oblique muscle, benign essential blepharospasm affects the muscles around the eye and does not result in the same visual disturbances.
- Fourth Nerve Palsy: Trochlear nerve palsy is characterized by dysfunction of the trochlear nerve, which causes weakness or paralysis of the superior oblique muscle. While SOM involves episodic contractions, fourth nerve palsy is characterized by a constant misalignment of the eyes, which results in persistent double vision.
- Hemifacial Spasm: A hemifacial spasm is a condition in which the muscles on one side of the face, including the eyelid muscles, contract involuntarily. While it may cause some ocular symptoms, it does not directly involve the superior oblique muscle and does not result in the same torsional eye movements as SOM.
- Myasthenia Gravis: Myasthenia gravis is an autoimmune condition that impairs neuromuscular transmission, resulting in muscle weakness and fatigue. Ocular myasthenia gravis can cause fluctuating double vision and ptosis (eyelid drooping), but it is not commonly associated with the episodic, twitching movements seen in SOM.
Prognosis
Patients with Superior Oblique Myokymia have a good prognosis because the condition is usually benign and does not cause progressive vision loss or serious complications. However, the frequency and severity of symptoms can differ from patient to patient, and some people may have persistent or worsening symptoms over time. With proper management, patients can usually achieve good symptom control and maintain a high quality of life.
Effective Diagnosis of Superior Oblique Myokymia
Superior Oblique Myokymia requires a thorough evaluation by an eye care professional, usually an ophthalmologist or neuro-ophthalmologist who specializes in eye and nervous system disorders. The diagnostic process consists of a thorough clinical examination, a detailed patient history, and specialized tests to confirm the diagnosis and rule out other possible causes of symptoms.
Clinical Examination
The clinical examination is an essential part of diagnosing SOM. The ophthalmologist will examine the patient’s eye movements to look for signs of abnormal contraction or twitching of the superior oblique muscle. The exam may include the following:
- Observation of Eye Movements: The doctor will closely monitor the patient’s eye movements while instructing them to follow a moving target or shift their gaze in different directions. The goal is to detect any involuntary, rapid, or irregular movements that are associated with SOM. These movements are often most visible when the patient looks downward and inward, as these directions engage the superior oblique muscle.
- Assessment of Visual Symptoms: The doctor will ask about the patient’s specific visual symptoms, such as oscillopsia, diplopia, or torsional movements. They may also ask the patient to describe the frequency, duration, and causes of their symptoms, as this information can aid in distinguishing SOM from other ocular conditions. The doctor may also assess the patient’s visual acuity and look for signs of misalignment or abnormalities in the eye’s position.
- Head Tilt Test: The head tilt test, also known as the Bielschowsky head tilt test, can be used to evaluate the function of the superior oblique muscle. Tilting the head to the affected side may exacerbate SOM symptoms, causing increased twitching or visual disturbances. In contrast, tilting the head away from the affected side may alleviate the symptoms.
Imaging Studies
Superior Oblique Myokymia is primarily diagnosed clinically, but imaging studies may be used to rule out underlying structural or neurological causes, such as neurovascular compression or demyelinating diseases. Common imaging techniques include the following:
- Magnetic Resonance Imaging (MRI) is a non-invasive imaging technique that uses magnetic fields and radio waves to produce detailed images of the brain, orbits, and cranial nerves. In the case of SOM, an MRI can help detect any neurovascular compression affecting the trochlear nerve or other abnormalities that may contribute to the condition. It is especially useful for detecting conditions like multiple sclerosis, which can cause demyelination and potentially lead to SOM-like symptoms.
- Magnetic Resonance Angiography (MRA): MRA is a subset of MRI that focuses on blood vessels. It can detect vascular abnormalities, such as an artery compressing the trochlear nerve. This test is especially important if neurovascular compression is suspected as the source of the patient’s symptoms.
- High-Resolution Computed Tomography (CT) Scan: A CT scan can produce detailed images of the bony structures surrounding the eye, as well as the cranial nerve pathways. It can be used if there is a possibility of bony abnormalities or trauma affecting the superior oblique muscle or its innervation.
Electromyography (EMG)
Electromyography (EMG) is a diagnostic test that detects electrical activity in muscles during contraction and at rest. EMG can detect abnormal muscle activity in the superior oblique muscle in the case of Superior Oblique Myokymia. This test involves applying small electrodes to the skin over the muscle or inserting a fine needle electrode into the muscle tissue. Electrical activity recorded during involuntary contractions can reveal important information about the underlying muscle hyperactivity and aid in the diagnosis of SOM.
Patient History
A thorough patient history is critical for diagnosing SOM. The healthcare provider will inquire about the onset, duration, and frequency of the symptoms, as well as any factors that appear to precipitate or exacerbate the condition. Information about the patient’s medical history, including any known neurological or vascular conditions, is also required. If the patient has a history of trauma, surgery, or any other relevant events, the clinician can use this information to identify possible contributing factors.
Response to Trial Therapies
In some cases, the response to trial therapies may serve as a diagnostic tool. For example, a muscle relaxant or anticonvulsant may be prescribed for a short period of time to see if it reduces the frequency or severity of myokymia. A positive response to these therapies can help confirm the diagnosis of SOM and guide future treatment plans.
Effective Oblique Myokymia Management
Managing Superior Oblique Myokymia (SOM) necessitates a personalized approach that addresses both the frequency and severity of symptoms while taking into account the patient’s unique needs and lifestyle. Although SOM is usually a minor condition, the visual disturbances it causes can be very disruptive, so effective management is critical for maintaining a good quality of life. SOM management strategies include conservative, non-invasive measures, as well as pharmacological and, in rare cases, surgical interventions.
Conservative Management
For many patients with mild or infrequent symptoms, conservative treatment may suffice. This approach focuses on reducing the severity of symptoms through lifestyle changes and coping strategies.
- Observation and Reassurance: Because SOM is a benign condition with no risk of permanent vision loss, patients may be reassured about the nature of their symptoms. In cases where episodes are uncommon or minimally disruptive, regular monitoring without active intervention may be recommended. Patients are encouraged to keep a symptom diary that includes triggers, frequency, and severity, as this can help both the patient and the clinician better understand the condition over time.
- Lifestyle Modifications: Identifying and avoiding potential SOM triggers can help you manage your symptoms effectively. Stress, fatigue, caffeine, and certain visual tasks are all potential triggers. Patients may be advised to practice stress-reduction techniques like meditation, deep breathing exercises, or yoga to help reduce the frequency of myokymia episodes. Additionally, getting enough sleep and maintaining good overall health can help to reduce symptom severity.
- Prism Glasses: Some patients, particularly those who experience diplopia during SOM episodes, may require prism glasses. These specialized lenses help to align the images seen by each eye, reducing the effects of double vision and increasing visual comfort.
Pharmacologic Treatment
When conservative measures fail to control symptoms, pharmacological intervention may be considered. Drug therapy aims to reduce the frequency and intensity of muscle contractions that cause visual disturbances.
- Carbamazepine: Carbamazepine, an anticonvulsant medication, has been used successfully to treat SOM. It works by stabilizing hyperactive nerve impulses, which reduces abnormal muscle contractions. Carbamazepine is frequently considered a first-line treatment for SOM, particularly in patients who experience frequent or severe symptoms. The dosage is typically started low and gradually increased until the desired effect is achieved, with careful monitoring for potential side effects such as dizziness, drowsiness, or gastrointestinal upset.
- Gabapentin: Gabapentin, an anticonvulsant, has been used to treat SOM. It is thought to work by modulating neurotransmitter release in the brain, thereby reducing the abnormal nerve activity that causes myokymia. Gabapentin is frequently considered in patients who do not respond to carbamazepine or who have severe side effects from other medications.
- Baclofen: Baclofen, a muscle relaxant, may also be used to treat SOM, especially if the condition is associated with spasticity or other treatments have proven ineffective. Baclofen works by inhibiting neurotransmitter release, which helps to relax overactive muscles. However, its use in SOM is less common, and it is usually considered when other medications fail.
- Propranolol: Propranolol, a beta-blocker commonly used to treat cardiovascular conditions, has been shown to be effective in certain cases of SOM. It is thought to reduce the number of episodes by inhibiting the sympathetic nervous system response. This option should be considered especially for patients who have anxiety or other stress-related symptoms that could worsen SOM.
Surgical Treatment
Surgical intervention is rarely required for Superior Oblique Myokymia and is typically reserved for cases where pharmacological treatments have failed and the patient’s quality of life has suffered significantly. Surgical options are only considered after a thorough assessment of the potential risks and benefits.
- Microvascular Decompression: If the underlying cause of SOM is neurovascular compression of the trochlear nerve, microvascular decompression surgery may be considered. This procedure involves repositioning or removing the blood vessel that is compressing the nerve in order to relieve pressure and reduce abnormal muscle contractions. Microvascular decompression has been used successfully in other cranial nerve hyperactivity disorders, and while it is a more invasive treatment, it may provide long-term relief to some patients.
- Superior Oblique Tenotomy: In severe cases of SOM where other treatments have failed, superior oblique tenotomy, a surgical procedure that partially cuts the superior oblique muscle tendon, may be considered. This procedure aims to reduce muscle tension and thus the frequency of involuntary contractions. However, because this surgery has a risk of causing double vision or other complications, it is typically reserved for patients with severe symptoms.
Long-Term Management and Follow-up
Long-term management of Superior Oblique Myokymia entails regular follow-up with an eye care professional to assess the efficacy of the chosen treatment and make necessary adjustments. Patients may need to try various medications or treatment combinations to determine the most effective regimen with the fewest side effects. In some cases, symptoms may improve with time, allowing for a reduction in treatment intensity.
Patient education is also an essential part of long-term management. Patients should be informed about the nature of the condition, the importance of following prescribed treatments, and the potential need for lifestyle changes to effectively manage symptoms.
Trusted Resources and Support
Books
- “Neuro-Ophthalmology: Diagnosis and Management” by Grant T. Liu, Nicholas J. Volpe, and Steven L. Galetta: This comprehensive textbook provides detailed information on the diagnosis and management of neuro-ophthalmological conditions, including Superior Oblique Myokymia. It is an essential resource for healthcare professionals and patients seeking an in-depth understanding of the condition.
- “The Neuro-Ophthalmology Survival Guide” by Anthony Pane, Neil R. Miller, and Jane E. Burdon: A practical guide that covers various neuro-ophthalmological disorders, including SOM. It offers valuable insights into symptom management and treatment options for patients and clinicians alike.
Organizations
- American Academy of Ophthalmology (AAO): The AAO provides a wealth of resources for patients and healthcare providers, including information on rare ocular conditions like Superior Oblique Myokymia. Their website offers access to patient education materials, professional guidelines, and a directory of certified ophthalmologists.
- North American Neuro-Ophthalmology Society (NANOS): NANOS is a professional organization dedicated to the field of neuro-ophthalmology. They offer resources for patients with conditions like SOM, including access to expert care, educational materials, and support networks.










