The sympathetic nervous system (SNS) is a critical component of the autonomic nervous system that orchestrates the body’s rapid “fight or flight” responses. It prepares the body for action by regulating heart rate, blood pressure, metabolism, and more, while also influencing functions such as digestion and temperature control. Understanding the SNS is vital for appreciating how our bodies react to stress and maintain homeostasis. In this guide, we delve into the complex anatomy, diverse functions, common disorders, state-of-the-art diagnostic techniques, and the broad spectrum of treatment and lifestyle approaches for optimal SNS health.
Table of Contents
- Anatomical Structure
- Preganglionic Neurons
- Sympathetic Ganglia
- Postganglionic Neurons & Fibers
- Sympathetic Pathways
- Adrenal Medulla Pathway
- Neurotransmitters & Receptors
- System Integration
- Functional Roles
- SNS Disorders
- Diagnostic Techniques
- Treatment Options
- Supplemental & Nutritional Support
- Lifestyle & Wellness Practices
- Trusted Resources
- Frequently Asked Questions
- Disclaimer & Sharing
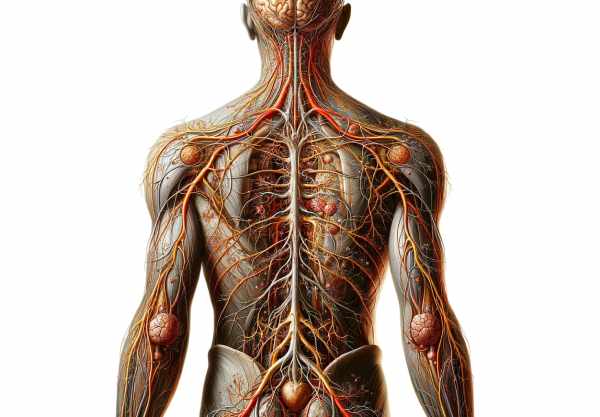
Anatomical Structure of the SNS
The sympathetic nervous system is intricately organized, originating in the thoracolumbar region of the spinal cord. Its structure comprises multiple neuronal layers that ensure rapid communication between the central nervous system and peripheral organs. The key components include:
- Preganglionic Neurons:
Located in the lateral horn of the spinal cord’s gray matter between the T1 and L2 segments, these neurons initiate the sympathetic response. They exit via the ventral roots to reach the sympathetic ganglia. - Sympathetic Ganglia:
Two primary types exist—paravertebral (sympathetic chain) and prevertebral ganglia. The sympathetic chain runs along the vertebral column, while prevertebral ganglia (such as the celiac, superior, and inferior mesenteric ganglia) are located in the abdominal region. These ganglia serve as relay stations where preganglionic neurons synapse with postganglionic neurons. - Postganglionic Neurons & Fibers:
After synapsing in the ganglia, postganglionic neurons extend toward target tissues. They predominantly release norepinephrine to stimulate adrenergic receptors, although in certain cases (e.g., sweat glands), acetylcholine is released.
This hierarchical organization enables the SNS to coordinate a swift and integrated response to various physiological challenges.
Preganglionic Neurons
Preganglionic neurons are the first tier of the sympathetic pathway. They play a crucial role in transmitting signals from the central nervous system to the peripheral ganglia.
- Origin and Location:
Their cell bodies reside in the lateral horn of the spinal cord, specifically between the T1 and L2 segments. This strategic placement in the thoracolumbar region enables them to control a wide range of bodily functions. - Pathway to Ganglia:
These neurons exit the spinal cord via the ventral roots. They then travel along short pathways to the adjacent sympathetic ganglia, where they synapse with postganglionic neurons. - Neurotransmitter Role:
Preganglionic neurons release acetylcholine at their synapses. This neurotransmitter binds to nicotinic receptors on the postganglionic neurons, thereby initiating the sympathetic response.
The efficiency of these neurons in conveying signals is fundamental for the rapid activation of the sympathetic nervous system during stress.
Sympathetic Ganglia
The sympathetic ganglia serve as relay points for the transmission of signals from the preganglionic neurons to the postganglionic neurons.
Paravertebral Ganglia
- Structure:
Also known as the sympathetic chain ganglia, these structures are arranged in a chain alongside the vertebral column, extending from the base of the skull to the coccyx. - Function:
They distribute sympathetic fibers to various regions including the head, neck, thorax, and limbs. The chain facilitates communication across multiple segments, ensuring a coordinated systemic response.
Prevertebral Ganglia
- Location:
Positioned in front of the vertebral column, near major abdominal arteries, these ganglia include the celiac, superior mesenteric, and inferior mesenteric ganglia. - Function:
They primarily innervate the abdominal and pelvic organs, regulating digestive, urinary, and reproductive functions.
By serving as critical relay stations, these ganglia ensure that sympathetic signals are accurately directed to their respective targets.
Postganglionic Neurons & Fibers
Postganglionic neurons represent the final step in the sympathetic pathway, conveying signals from the ganglia to the target organs.
- Pathway:
After receiving signals from preganglionic neurons, postganglionic neurons extend long fibers from the ganglia to various peripheral tissues. Their distribution covers multiple organ systems, including the cardiovascular, respiratory, and digestive systems. - Neurotransmitter Release:
These neurons primarily secrete norepinephrine, which interacts with adrenergic receptors on target tissues, resulting in responses such as vasoconstriction, increased heart rate, and bronchodilation. In certain regions, such as sweat glands, they may release acetylcholine. - Fiber Types:
The sympathetic system contains both myelinated fibers (mostly preganglionic) that facilitate rapid signal conduction and unmyelinated fibers (postganglionic) that conduct signals more slowly.
This final relay step is essential for the execution of the physiological responses orchestrated by the SNS.
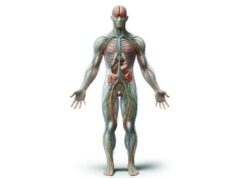
Sympathetic Pathways
Sympathetic pathways are the conduits by which sympathetic signals are delivered to target organs throughout the body. These pathways are categorized based on their destination:
Head and Neck
- Origin:
Sympathetic fibers serving the head and neck originate in the upper thoracic segments and synapse in the superior cervical ganglion. - Function:
They control functions such as pupil dilation, decreased salivary secretion, and vasoconstriction in facial blood vessels, thereby modulating responses like fight-or-flight reactions.
Thoracic Organs
- Origin:
Fibers for thoracic organs arise from the mid-thoracic segments. - Function:
These fibers increase heart rate and contractility, facilitate bronchodilation, and regulate blood flow to the lungs, ensuring that the body can respond rapidly to physical demands.
Abdominal Organs
- Origin:
Derived from the lower thoracic and upper lumbar segments, these fibers pass through the prevertebral ganglia. - Function:
They innervate the liver, stomach, intestines, and kidneys. Their actions include stimulating glycogenolysis, reducing gastrointestinal motility, and modulating renal functions, thereby prioritizing energy use during stress.
Pelvic Organs
- Origin:
These fibers arise from the lower lumbar and sacral segments. - Function:
They play a role in controlling functions such as bladder relaxation, sexual arousal (ejaculation), and vasoconstriction in the pelvic region.
Understanding these pathways is crucial to appreciating how the SNS coordinates a widespread, integrated response across various organ systems.
Adrenal Medulla Pathway
The sympathetic nervous system uniquely innervates the adrenal medulla, a part of the adrenal glands, directly via preganglionic neurons.
- Mechanism:
Preganglionic neurons release acetylcholine directly onto the adrenal medulla. In response, the adrenal medulla secretes catecholamines—primarily epinephrine (adrenaline) and norepinephrine—into the bloodstream. - Systemic Impact:
This direct pathway results in a widespread and sustained sympathetic response, which amplifies the body’s ability to cope with stress by increasing heart rate, blood pressure, and energy mobilization.
This connection between the SNS and the adrenal medulla is a cornerstone of the body’s acute stress response.
Neurotransmitters & Receptors
The communication within the sympathetic nervous system is mediated by specific neurotransmitters and their corresponding receptors.
Neurotransmitters
- Acetylcholine:
Released by preganglionic neurons, acetylcholine binds to nicotinic receptors on postganglionic neurons. In certain target tissues, such as sweat glands, acetylcholine is also released by postganglionic neurons. - Norepinephrine:
The predominant neurotransmitter of postganglionic neurons, norepinephrine binds to adrenergic receptors on target tissues, eliciting responses such as increased heart rate, vasoconstriction, and bronchodilation. - Epinephrine:
Secreted by the adrenal medulla, epinephrine acts systemically to reinforce sympathetic responses, particularly during the fight-or-flight response.
Receptors
- Nicotinic Receptors:
Found on postganglionic neurons, these receptors bind acetylcholine, initiating synaptic transmission in the sympathetic pathway. - Adrenergic Receptors:
These receptors are located on various target tissues and are divided into: - Alpha Receptors:
Alpha-1 receptors mediate vasoconstriction and increased peripheral resistance, while alpha-2 receptors modulate neurotransmitter release. - Beta Receptors:
Beta-1 receptors primarily affect the heart, increasing heart rate and contractility; beta-2 receptors mediate bronchodilation and vasodilation in specific tissues; beta-3 receptors are involved in lipolysis and thermogenesis.
The specificity and distribution of these neurotransmitters and receptors ensure that the SNS can elicit precise and coordinated physiological responses.
Integration with Other Systems
The sympathetic nervous system does not work in isolation; it is intricately integrated with other components of the autonomic nervous system to maintain balance and homeostasis.
Parasympathetic Collaboration
- Opposing Roles:
The parasympathetic nervous system (PNS) generally promotes rest, digestion, and conservation of energy. While the SNS triggers fight-or-flight responses, the PNS helps the body relax and recover. - Balanced Function:
The interplay between the SNS and PNS ensures that the body can quickly switch between states of alertness and rest, optimizing overall function.
Central Control by the Hypothalamus
- Regulatory Center:
The hypothalamus acts as the central coordinator of the autonomic nervous system. It processes sensory input and orchestrates the appropriate balance between sympathetic and parasympathetic activity. - Stress Response:
Under stress, the hypothalamus signals the SNS to ramp up activity, while simultaneously modulating the PNS to ensure that the response is proportionate and controlled.
This integration is critical for maintaining physiological balance and enabling the body to adapt to changing environmental demands.
Functional Roles of the SNS
The sympathetic nervous system is essential for orchestrating the body’s rapid response to stress and maintaining homeostasis. Its key functions include:
Cardiovascular Regulation
- Heart Rate and Contractility:
By stimulating beta-1 adrenergic receptors in the heart, the SNS increases heart rate and the force of cardiac contraction. This ensures enhanced blood flow during stressful situations. - Vascular Tone:
Through alpha-adrenergic receptors, the SNS induces vasoconstriction, raising blood pressure and directing blood flow to critical organs and muscles.
Respiratory Enhancement
- Bronchodilation:
Activation of beta-2 adrenergic receptors in the bronchioles causes relaxation of smooth muscle, leading to bronchodilation. This improves airflow and oxygen delivery during increased physical activity or stress.
Metabolic Regulation
- Energy Mobilization:
The SNS promotes glycogenolysis in the liver and lipolysis in adipose tissue, increasing the availability of glucose and fatty acids for immediate energy. - Thermogenesis:
By stimulating brown adipose tissue via beta-3 receptors, the SNS generates heat through non-shivering thermogenesis, which is important for maintaining body temperature in cold environments.
Digestive System Inhibition
- Reduced Gastrointestinal Activity:
During acute stress, the SNS suppresses gastrointestinal motility and secretion, conserving energy for vital functions and redirecting blood flow to the muscles and heart.
Overall Stress Response
- Catecholamine Release:
The SNS, along with the adrenal medulla, releases catecholamines (epinephrine and norepinephrine) into the bloodstream, facilitating a widespread physiological response that prepares the body for immediate action.
These functional roles collectively ensure that the body can rapidly adapt to stress, sustain vital functions, and maintain internal balance.
Disorders of the Sympathetic Nervous System
Disruptions in the sympathetic nervous system can lead to a range of disorders, resulting from either overactivity, underactivity, or structural abnormalities. These conditions can significantly impact overall health.
Hyperactivity Disorders
Hypertension
- Mechanism:
Excessive sympathetic stimulation leads to persistent vasoconstriction and increased heart rate, contributing to elevated blood pressure. - Symptoms:
Often asymptomatic until severe; may cause headaches, dizziness, and, in extreme cases, cardiovascular complications. - Treatment:
Lifestyle modifications, beta blockers, ACE inhibitors, and stress management techniques are commonly used.
Hyperhidrosis
- Mechanism:
Overactive sympathetic stimulation of sweat glands results in excessive sweating. - Symptoms:
Localized or generalized excessive sweating that interferes with daily activities. - Treatment:
Options include topical antiperspirants, oral anticholinergics, Botox injections, iontophoresis, and surgical sympathectomy for severe cases.
Panic Disorder
- Mechanism:
Dysregulated sympathetic activity triggers sudden, intense episodes of fear and physiological arousal. - Symptoms:
Rapid heartbeat, sweating, trembling, and a sense of impending doom. - Treatment:
Cognitive-behavioral therapy (CBT), SSRIs, and benzodiazepines help manage symptoms.
Hypoactivity Disorders
Orthostatic Hypotension
- Mechanism:
Inadequate sympathetic response during postural changes results in a sudden drop in blood pressure. - Symptoms:
Dizziness, lightheadedness, and even fainting upon standing. - Treatment:
Increasing fluid and salt intake, wearing compression stockings, and medications to elevate blood pressure can be effective.
Horner’s Syndrome
- Mechanism:
Damage to the sympathetic pathway affecting the face leads to a characteristic triad of symptoms. - Symptoms:
Ptosis (drooping eyelid), miosis (constricted pupil), and anhidrosis (lack of sweating) on the affected side. - Treatment:
Managing the underlying cause, though some deficits may persist.
Structural Abnormalities
Pheochromocytoma
- Mechanism:
A rare tumor of the adrenal medulla secretes excessive catecholamines, leading to severe sympathetic overactivity. - Symptoms:
Episodes of high blood pressure, headaches, excessive sweating, and palpitations. - Treatment:
Surgical removal of the tumor along with preoperative medical management is crucial.
Complex Regional Pain Syndrome (CRPS)
- Mechanism:
Abnormal sympathetic nerve activity following an injury causes chronic, debilitating pain. - Symptoms:
Severe pain, swelling, and changes in skin color and temperature in the affected limb. - Treatment:
Physical therapy, nerve blocks, and medications are part of a multimodal approach.
Dysautonomia
Postural Orthostatic Tachycardia Syndrome (POTS)
- Mechanism:
An abnormal autonomic response causes a significant increase in heart rate upon standing. - Symptoms:
Dizziness, rapid heartbeat, fatigue, and difficulty concentrating. - Treatment:
Increased fluid and salt intake, medications, and physical therapy to improve vascular tone and autonomic balance.
Autonomic Neuropathy
- Mechanism:
Damage to autonomic nerves, often due to chronic conditions like diabetes, affects the SNS. - Symptoms:
Variable, including gastrointestinal, cardiovascular, and urinary disturbances. - Treatment:
Managing the underlying condition, along with symptom-specific treatments and lifestyle modifications.
Stress-Related and Metabolic Disorders
Chronic Fatigue Syndrome (CFS)
- Mechanism:
Chronic overactivation of the sympathetic nervous system may contribute to the debilitating fatigue seen in CFS. - Symptoms:
Extreme, persistent fatigue that is not alleviated by rest, accompanied by cognitive difficulties and muscle pain. - Treatment:
Graded exercise therapy, cognitive-behavioral therapy, and medications to manage symptoms.
Metabolic Syndrome
- Mechanism:
Prolonged sympathetic hyperactivity can contribute to insulin resistance, hypertension, and dyslipidemia. - Symptoms:
Abdominal obesity, high blood pressure, elevated blood sugar, and abnormal cholesterol levels. - Treatment:
Lifestyle modifications, including diet and exercise, alongside medications to address individual metabolic components.
Diagnostic Techniques for SNS Disorders
A precise diagnosis of sympathetic nervous system disorders requires a multifaceted approach that includes detailed patient history, physical examinations, laboratory investigations, imaging studies, and specialized autonomic tests.
Patient History and Physical Examination
- Comprehensive History:
Clinicians gather detailed information about symptom onset, duration, triggers, and associated conditions. Family history, lifestyle factors, and previous medical issues are also important. - Physical Exam:
A thorough examination assesses vital signs, skin changes (such as sweating patterns), pupil responses, and cardiovascular parameters.
Laboratory Investigations
- Blood Tests:
Blood panels, including complete blood counts, metabolic panels, and thyroid function tests, help identify systemic conditions affecting the SNS. Measurement of catecholamines and their metabolites (metanephrines) is crucial for diagnosing pheochromocytoma. - Urine Tests:
A 24-hour urine collection can detect elevated catecholamine metabolites, assisting in the diagnosis of catecholamine-secreting tumors.
Imaging Studies
- MRI and CT Scans:
These imaging modalities provide detailed views of the brain, spinal cord, and adrenal glands, helping to detect structural lesions, tumors, or other abnormalities affecting the SNS. - PET Scans:
Combined with CT or MRI, PET scans evaluate metabolic activity and can be instrumental in diagnosing malignancies.
Autonomic Function Tests
- Tilt Table Test:
This test evaluates the body’s cardiovascular response to positional changes, helping diagnose conditions like orthostatic hypotension and POTS. - Heart Rate Variability (HRV):
HRV analysis measures the variation in time between heartbeats, reflecting autonomic nervous system balance. - Deep Breathing and Valsalva Maneuver:
These tests assess the parasympathetic and sympathetic responses by monitoring changes in heart rate and blood pressure during controlled breathing and forced exhalation.
Electrophysiological Studies
- Electromyography (EMG) and Nerve Conduction Studies (NCS):
Although primarily used for peripheral nerve evaluation, these tests can help detect neuropathies that impact the autonomic fibers. - Sympathetic Skin Response (SSR):
SSR measures changes in skin electrical potential in response to stimuli, providing insight into the integrity of sympathetic nerve fibers.
Genetic Testing and Biopsy
- Genetic Analysis:
In cases of suspected hereditary dysautonomia, genetic tests can identify mutations that affect autonomic nerve function. - Nerve Biopsy:
Rarely, a nerve biopsy may be necessary to confirm a diagnosis when other tests are inconclusive.
Functional MRI (fMRI)
- Central Autonomic Network Evaluation:
fMRI can assess the activity of brain regions involved in autonomic regulation, offering insights into central contributions to dysautonomia.
Treatment Options for SNS Disorders
Effective management of sympathetic nervous system disorders requires a tailored, multidisciplinary approach that may involve pharmacologic, surgical, and non-pharmacologic interventions.
Pharmacologic Treatments
Beta Blockers
- Function:
Beta blockers such as propranolol, metoprolol, and atenolol reduce heart rate and blood pressure by blocking beta-adrenergic receptors, thereby mitigating the effects of excessive sympathetic stimulation. - Indications:
Commonly used for hypertension, anxiety disorders, and certain tachyarrhythmias.
Alpha Blockers
- Function:
Alpha blockers, including prazosin, doxazosin, and terazosin, lower vascular resistance by blocking alpha-adrenergic receptors, which helps reduce blood pressure. - Indications:
Often used in conditions like pheochromocytoma and refractory hypertension.
Anticholinergic Agents
- Function:
These medications, such as glycopyrrolate and oxybutynin, reduce sweating by inhibiting the action of acetylcholine on sweat glands. - Indications:
Primarily used for hyperhidrosis and other conditions characterized by excessive sweat production.
Anti-Anxiety Medications
- Function:
SSRIs (e.g., sertraline, fluoxetine) and benzodiazepines (e.g., diazepam) help manage anxiety and panic disorders by modulating neurotransmitter levels. - Indications:
Effective in reducing the sympathetic overdrive associated with anxiety and panic attacks.
Surgical Interventions
Sympathectomy
- Procedure:
Endoscopic thoracic sympathectomy (ETS) involves interrupting the sympathetic nerve chain to reduce excessive sweating or relieve symptoms of certain vascular disorders. - Indications:
Typically reserved for severe hyperhidrosis or refractory cases of Raynaud’s phenomenon. - Risks:
Potential side effects include compensatory sweating and nerve damage.
Tumor Resection
- Procedure:
Surgical removal of tumors such as pheochromocytoma, which secrete excessive catecholamines. - Indications:
Effective in resolving symptoms once the tumor is removed, though careful perioperative management is required.
Innovative and Experimental Therapies
Biofeedback
- Mechanism:
Biofeedback trains patients to control certain physiological functions by using real-time monitoring devices. - Benefits:
Can reduce stress, improve heart rate variability, and help regulate blood pressure.
Deep Brain Stimulation (DBS)
- Mechanism:
DBS involves implanting electrodes in targeted brain regions to modulate neural circuits controlling autonomic function. - Applications:
Currently experimental for certain dysautonomias and chronic pain conditions.
Transcutaneous Electrical Nerve Stimulation (TENS)
- Mechanism:
TENS uses low-voltage electrical currents applied to the skin to reduce pain and modulate autonomic responses. - Applications:
Useful in managing conditions like complex regional pain syndrome (CRPS) and neuropathic pain.
Supplements for SNS Health
Certain supplements can support the health and function of the sympathetic nervous system by enhancing nerve function, reducing oxidative stress, and balancing neurotransmitter activity.
Vitamins and Minerals
- Vitamin B Complex:
B vitamins (B1, B6, and B12) are vital for energy production, nerve repair, and neurotransmitter synthesis. - Vitamin D:
Essential for maintaining nerve health and modulating immune function. - Magnesium:
Promotes muscle relaxation and nerve conduction, reducing stress-induced sympathetic overactivity. - Zinc:
Supports immune function and facilitates cellular repair processes.
Herbal Supplements
- Ashwagandha:
An adaptogenic herb that helps regulate the stress response by lowering cortisol levels and promoting overall nervous system health. - Rhodiola Rosea:
Known to reduce fatigue and enhance mental performance by modulating the sympathetic nervous system. - Valerian Root:
Promotes relaxation and helps manage anxiety by enhancing GABAergic activity.
Omega-3 Fatty Acids
- Fish Oil & Flaxseed Oil:
Omega-3 fatty acids possess anti-inflammatory properties and support cognitive and nerve function by reducing systemic inflammation.
Antioxidants
- Alpha-Lipoic Acid:
Protects nerve cells from oxidative damage and supports energy production, which is essential for nerve regeneration. - Coenzyme Q10 (CoQ10):
Plays a key role in mitochondrial function and acts as a potent antioxidant to reduce oxidative stress.
Amino Acids
- L-Theanine:
Promotes relaxation without sedation and supports cognitive function, helping to mitigate the effects of chronic stress. - Acetyl-L-Carnitine:
Enhances energy production in nerve cells and has neuroprotective properties that may reduce neuropathic pain.
Lifestyle & Wellness Practices for SNS Health
Adopting a healthy lifestyle is crucial to maintaining the balance and function of the sympathetic nervous system. Here are evidence-based strategies to promote SNS health:
Stress Management
- Mindfulness Meditation:
Regular mindfulness practice helps reduce cortisol levels and enhances parasympathetic tone. - Yoga and Deep Breathing:
These practices encourage relaxation and improve heart rate variability, thereby balancing sympathetic output. - Biofeedback:
Learning to control physiological responses through biofeedback can enhance autonomic regulation.
Physical Activity
- Regular Exercise:
Engage in moderate aerobic and resistance training to improve cardiovascular health and autonomic balance. - Consistency:
Regular physical activity can lower resting heart rate and reduce sympathetic overactivity.
Nutrition and Hydration
- Balanced Diet:
Consume nutrient-dense foods such as fruits, vegetables, lean proteins, and whole grains. Avoid processed foods high in sugar and unhealthy fats. - Hydration:
Adequate water intake supports blood circulation and optimal nerve function. - Limit Stimulants:
Reduce caffeine and alcohol consumption, which can exacerbate sympathetic activation.
Sleep and Recovery
- Quality Sleep:
Aim for 7–9 hours of restorative sleep each night to support nerve repair and hormonal balance. - Sleep Hygiene:
Establish a consistent sleep schedule and create a calming bedtime routine to improve sleep quality.
Weight Management
- Healthy Weight:
Maintaining a healthy weight reduces strain on the cardiovascular system and lowers the risk of hypertension, which is closely linked to SNS overactivity. - Regular Monitoring:
Regular physical check-ups and dietary adjustments can help maintain weight and overall metabolic health.
Avoiding Harmful Substances
- No Smoking:
Smoking increases sympathetic activity and is a risk factor for numerous cardiovascular and neurological conditions. - Moderate Alcohol Use:
Limit alcohol intake to avoid disrupting autonomic balance and exacerbating SNS overactivity.
Regular Medical Check-Ups
- Preventive Care:
Regular consultations with healthcare providers allow early detection and management of conditions affecting the SNS. - Monitoring:
Routine cardiovascular and autonomic assessments help maintain optimal SNS function.
Trusted Resources for SNS Health
For additional information on the sympathetic nervous system and its disorders, the following reputable resources offer comprehensive insights:
Books
- “The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma” by Bessel van der Kolk, M.D.
Explores how trauma affects the nervous system and offers strategies for healing. - “Why Zebras Don’t Get Ulcers: The Acclaimed Guide to Stress, Stress-Related Diseases, and Coping” by Robert M. Sapolsky
Provides an in-depth look at how chronic stress impacts the body, including the SNS. - “The Polyvagal Theory: Neurophysiological Foundations of Emotions, Attachment, Communication, and Self-Regulation” by Stephen W. Porges
Delves into autonomic regulation and the interplay between the sympathetic and parasympathetic systems.
Academic Journals
- Journal of Neurophysiology:
Publishes cutting-edge research on nervous system function and autonomic regulation. - Autonomic Neuroscience: Basic and Clinical:
Focuses on both basic and clinical aspects of autonomic nervous system research, including the SNS.
Mobile Applications
- Calm:
Offers guided meditations and stress-relief exercises to promote autonomic balance. - Headspace:
Provides mindfulness and meditation practices that help reduce stress and support SNS health. - Heart Rate Monitor by Azumio:
Allows users to track heart rate variability and other indicators of autonomic nervous system function.
Frequently Asked Questions
What is the primary role of the sympathetic nervous system?
The sympathetic nervous system prepares the body for fight-or-flight responses by increasing heart rate, dilating bronchioles, mobilizing energy stores, and redirecting blood flow to essential organs during stress.
How does the SNS regulate cardiovascular function?
It increases heart rate and contractility via beta-1 receptors while causing vasoconstriction through alpha receptors, thereby raising blood pressure and ensuring adequate blood flow during stress.
What neurotransmitters are involved in SNS signaling?
Preganglionic neurons release acetylcholine, while postganglionic neurons primarily release norepinephrine. The adrenal medulla also secretes epinephrine to amplify the sympathetic response.
How is the SNS diagnosed in cases of dysfunction?
Diagnosis involves clinical history, physical examinations, blood and urine tests for catecholamines, imaging studies, autonomic function tests (such as the tilt table test), and sometimes electrophysiological studies.
What lifestyle changes can support SNS health?
Effective strategies include stress management through mindfulness, regular physical activity, a balanced diet, proper hydration, adequate sleep, and avoiding stimulants like caffeine and nicotine.
Disclaimer & Sharing
The information provided in this article is for educational purposes only and should not be considered a substitute for professional medical advice. Always consult with a qualified healthcare provider for diagnosis and treatment specific to your needs.
If you found this guide helpful, please share it on Facebook, X (formerly Twitter), or your preferred social platform to help spread awareness about sympathetic nervous system health and promote balanced well-being.