Retinal vein occlusion (RVO) is a common and potentially vision-threatening ocular condition that occurs when one of the veins that transport blood away from the retina becomes clogged. The retina is the light-sensitive layer at the back of the eye that converts light into electrical signals and sends them to the brain, allowing us to see. When the retinal vein becomes occluded, the normal outflow of blood becomes obstructed, resulting in increased capillary pressure, retinal hemorrhages, and fluid leakage. This can cause retinal swelling (edema), retinal tissue damage, and, if left untreated, severe vision loss.
Types of Retinal Vein Occlusion
There are two types of RVO: branch retinal vein occlusion (BRVO) and central retinal vein occlusion (CRVO). Each type has different characteristics, risk factors, and clinical implications.
Branch Retinal Vein Occlusion (BRVO)
When one of the central retinal vein’s smaller branches becomes clogged, it causes BRVO. The occlusion usually occurs where a retinal artery and vein intersect, which is particularly vulnerable to compression by atherosclerotic (hardened) arteries. The blockage causes blood and fluid leakage in the retina served by the affected branch, resulting in localized hemorrhages and edema.
BRVO is more common than CRVO and typically affects a single quadrant of the retina, resulting in sectoral visual field loss. The severity of vision loss in BRVO varies according to the location and size of the occlusion. If the macula—the part of the retina responsible for central vision—is involved, the visual impact can be severe. In some cases, BRVO can cause complications such as macular edema (swelling of the macula) or neovascularization (the formation of new, abnormal blood vessels), which can worsen vision.
Central retinal vein occlusion (CRVO)
CRVO happens when the central retinal vein, which drains blood from the entire retina, becomes clogged. This type of occlusion has a broader impact on the retina than BRVO, resulting in more extensive retinal hemorrhages, edema, and ischemia (lack of oxygen). There are two subtypes of CRVO: non-ischemic and ischemic.
- Non-Ischemic CRVO: This is a milder form of CRVO that causes partial blockage of the central retinal veins. While blood flow continues through the vein, outflow is reduced, resulting in retinal hemorrhages and edema. Non-ischemic CRVO causes less severe vision loss and has a better prognosis than ischemic CRVO. However, non-ischemic CRVO can progress to ischemic form over time.
- Ischemic CRVO: This is the most severe type of CRVO, characterized by a complete blockage of the central retinal vein, which causes extensive retinal ischemia. A lack of oxygen supply to the retina can result in significant vision loss, as well as an increased risk of complications such as neovascular glaucoma. Ischemic CRVO has a poorer visual prognosis and requires more aggressive treatment.
The pathophysiology of retinal vein occlusion
The pathophysiology of RVO is complex, with a number of factors contributing to retinal vein obstruction. The most common underlying cause is the formation of a thrombus (blood clot) within the vein, which restricts blood flow and raises intravascular pressure. Several factors influence thrombus formation, including:
- Atherosclerosis: Arterial hardening and narrowing caused by plaque buildup is a significant risk factor for RVO, especially in BRVO. Atherosclerosis in the adjacent retinal artery can compress the vein at arteriovenous crossing points, resulting in thrombosis.
- Hypercoagulable States: Conditions that cause blood to clot more easily, such as certain blood disorders, prolonged immobility, or the use of certain medications, can predispose people to RVO. Systemic conditions such as diabetes, hypertension, and high cholesterol levels all contribute to hypercoagulability.
- Inflammation: Inflammatory conditions affecting blood vessels, such as vasculitis, can cause endothelial damage and increase the risk of retinal vein thrombosis.
- Increased Intraocular Pressure: Elevated pressure within the eye, as seen in glaucoma, can compress the central retinal vein near the lamina cribrosa (a sieve-like structure in the optic nerve), contributing to the development of CRVO.
When a retinal vein becomes occluded, the capillaries experience increased pressure, which can cause them to rupture. This causes retinal hemorrhages, where blood leaks into the retinal tissue. Impaired blood flow also causes hypoxia (oxygen deprivation) in the affected retinal areas, which can stimulate the release of vascular endothelial growth factor (VEGF). VEGF stimulates the formation of new blood vessels in an attempt to restore oxygen supply, but these new vessels are frequently abnormal and fragile, resulting in additional complications such as macular edema, vitreous hemorrhage, and neovascular glaucoma.
Risk Factors for Retinal Vein Occlusion
Several risk factors, many of which are associated with systemic vascular conditions, increase the likelihood of developing RVO. Key risk factors are:
- Age: RVO occurs more frequently in older adults, particularly those over the age of 50. The risk rises with age due to the higher prevalence of atherosclerosis, hypertension, and other systemic conditions in this population.
- Hypertension: High blood pressure is a major risk factor for RVO, especially BRVO. Hypertension contributes to the progression of atherosclerosis, which can compress the retinal veins and cause thrombus formation.
- Diabetes Mellitus: Diabetes is another significant risk factor for RVO because it increases the likelihood of developing microvascular complications, such as retinal vessel damage. Diabetic retinopathy, a common complication of diabetes, can coexist with RVO and exacerbate retinal damage.
- Glaucoma: Elevated intraocular pressure, which occurs in glaucoma, is a well-known risk factor for CRVO. Increased pressure can compress the central retinal vein, contributing to the formation of an occlusion.
- Hyperlipidemia: High levels of cholesterol and triglycerides in the blood can cause atherosclerosis, which increases the risk of RVO.
- Smoking: Smoking significantly increases the risk of cardiovascular disease and atherosclerosis, both of which contribute to the development of RVO. Smoking also promotes hypercoagulability, which increases the risk of thrombus formation.
- Obesity: Obesity is associated with a number of cardiovascular risk factors, including hypertension, diabetes, and hyperlipidemia, all of which increase the risk of RVO.
- Systemic Inflammatory Conditions: Vasculitis and autoimmune disorders can cause inflammation in the blood vessels, increasing the risk of RVO.
- Blood Disorders: Certain blood disorders, such as polycythemia vera or antiphospholipid syndrome, increase the likelihood of blood clot formation, which increases the risk of RVO.
Symptoms of Retinal Vein Occlusion
The symptoms of RVO differ depending on the type and severity of the occlusion, as well as the degree of retinal involvement. Common symptoms include:
- Sudden Vision Loss: The most common and concerning symptom of RVO is a brief, painless loss of vision in one eye. The degree of vision loss can range from mild blurring to complete blindness, depending on the location and severity of the occlusion.
- Blurred Vision: Patients with BRVO may have blurred or distorted vision, especially in the affected quadrant of the visual field. CRVO can affect the entire visual field, resulting in a significant reduction in visual acuity.
- Visual Field Defects: BRVO typically causes sectoral visual field defects, which correspond to the area of the retina served by the occluded vein. CRVO, on the other hand, can result in a more widespread visual field loss.
- Photopsia: Some patients may experience photopsia, or the perception of light flashes in their peripheral vision. This symptom is commonly associated with retinal traction or ischemia.
- Floaters: When an occlusion causes vitreous hemorrhage, patients may notice small, dark spots moving across their field of vision.
- Distortion of Vision (Metamorphopsia): Macular edema, a common complication of RVO, can cause metamorphopsia, which is characterized by wavy or bent straight lines. This visual distortion can have a significant impact on daily activities like reading and facial recognition.
Complications of Retinal Vein Occlusion
If untreated, RVO can cause a number of serious complications, including permanent vision loss. The complications include:
- Macular Edema: The most common complication of RVO is macular edema, which occurs when fluid enters the macula and causes it to swell. Macular edema is a leading cause of vision loss in RVO patients and must be treated promptly to avoid permanent damage to the central vision.
- Neovascularization: RVO-induced retinal ischemia can cause VEGF release, resulting in the formation of new, abnormal blood vessels. These vessels are fragile and prone to bleeding, which can lead to vitreous hemorrhage and further vision loss. Neovascularization can also lead to neovascular glaucoma, a severe and painful condition in which new blood vessels form on the iris and in the eye’s drainage angle, resulting in a significant increase in intraocular pressure. This condition requires immediate treatment to avoid permanent optic nerve damage and vision loss.
- Vitreous Hemorrhage: The fragile new blood vessels that form as a result of retinal ischemia may rupture, resulting in bleeding into the vitreous cavity. Vitreous hemorrhage can cause a sudden loss of vision, floaters, and even complete vision loss if the bleeding is severe. In some cases, the blood can clear on its own, but severe hemorrhage may necessitate surgical intervention.
- Retinal Detachment: In rare cases, neovascularization and vitreous traction can cause retinal detachment, in which the retina pulls away from the underlying supportive tissue. Retinal detachment is a medical emergency that can result in permanent blindness if not treated right away. Patients with RVO who develop retinal detachment may notice an increase in floaters, flashes of light, and a shadow or curtain effect across their field of vision.
- Neovascular Glaucoma: As previously stated, neovascular glaucoma is a serious complication of RVO, especially in ischemic CRVO. The formation of new blood vessels in the drainage angle of the eye can obstruct the outflow of aqueous humor, resulting in a rapid rise in intraocular pressure. This pressure can damage the optic nerve, causing irreversible vision loss. Neovascular glaucoma is often difficult to treat and may necessitate a combination of medical, laser, and surgical procedures.
The prognosis of retinal vein occlusion
The prognosis of RVO varies according to the type of occlusion, the degree of retinal involvement, and the presence of complications. Overall, BRVO has a better prognosis than CRVO, particularly if the macula is not involved. Many patients with BRVO may experience spontaneous vision improvement over time, especially if macular edema is mild and there is no significant ischemia.
In contrast, CRVO, particularly the ischemic type, has a worse visual prognosis due to widespread retinal damage and a higher risk of complications like neovascularization and neovascular glaucoma. Non-ischemic CRVO may have a better prognosis, but close monitoring is required because it can progress to the ischemic form.
The presence of macular edema is a significant predictor of visual outcome in both BRVO and CRVO. Early detection and treatment of macular edema are critical for maintaining central vision and improving long-term visual outcomes.
Diagnostic Tools for Retinal Vein Occlusion
Retinal vein occlusion (RVO) is diagnosed using a combination of clinical examination, imaging studies, and laboratory tests to determine the extent of retinal damage, identify the underlying cause, and guide treatment. Early and accurate diagnosis is critical for avoiding complications and maintaining vision.
Clinical Examination
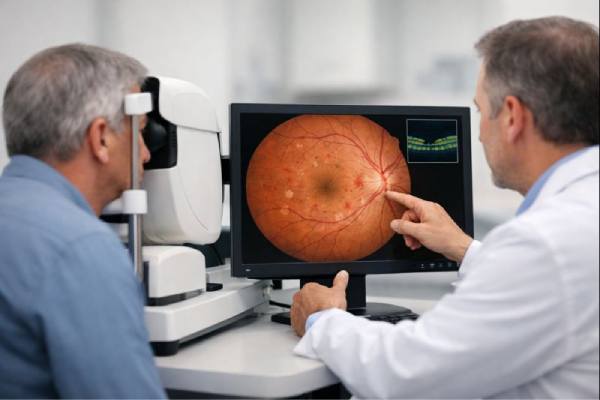
The first step in diagnosing RVO is a comprehensive clinical examination by an ophthalmologist or retina specialist. The examination starts with a thorough patient history, which includes the onset, duration, and nature of symptoms like vision loss, floaters, or photopsia. The clinician will also ask about the patient’s overall health, including any history of hypertension, diabetes, hyperlipidemia, or other vascular risk factors.
During the eye exam, the clinician will perform a visual acuity test to evaluate the patient’s central vision and a slit-lamp examination to examine the anterior segment of the eye. A dilated fundus examination is required to visualize the retina and identify characteristic signs of RVO, including retinal hemorrhages, dilated and tortuous veins, cotton-wool spots (areas of retinal ischemia), and macular edema.
CRVO can affect the entire retina, resulting in widespread hemorrhages and edema. In BRVO, retinal changes are typically limited to the area served by the occluded branch vein, resulting in sectoral hemorrhages and edema.
Optical Coherence Tomography(OCT)
Optical coherence tomography (OCT) is a non-invasive imaging technique that produces high-resolution cross-sections of the retina. OCT is an invaluable tool for diagnosing and monitoring RVO because it allows for detailed visualization of retinal layers as well as detection of macular edema.
In RVO patients, OCT can reveal the extent of macular edema, intraretinal cysts, and subretinal fluid, all of which are important indicators of disease severity and guide treatment decisions. OCT can also help monitor the response to treatment, such as anti-VEGF therapy or corticosteroid injections, by detecting changes in retinal thickness and fluid levels over time.
Fluorescein Angiography(FA)
Fluorescein angiography (FA) is a diagnostic test that involves injecting a fluorescent dye into the bloodstream and taking a series of photographs while the dye circulates through the retinal blood vessels. FA is especially useful for determining the extent of retinal ischemia, pinpointing areas of capillary non-perfusion, and detecting neovascularization.
In cases of BRVO, FA can help define the area of retinal involvement and assess the degree of macular ischemia. In CRVO, FA can distinguish between non-ischemic and ischemic forms by demonstrating capillary dropout and identifying areas of retinal neovascularization.
FA is also useful for planning laser photocoagulation therapy because it can identify areas of retinal ischemia that may benefit from targeted treatment to reduce the risk of neovascular complications.
Fundus Photography
Fundus photography is a standard imaging technique for documenting the appearance of the retina in RVO patients. High-resolution retinal photographs provide a visual record of retinal hemorrhages, vascular changes, and other signs of RVO, allowing for long-term disease progression monitoring.
Fundus photography is especially useful for informing patients about their condition and comparing retinal changes between follow-up visits. It can also be used to document treatment outcomes and evaluate the efficacy of interventions like laser therapy or intravitreal injections.
B-scan ultrasonography
B-scan ultrasonography is an imaging technique that uses sound waves to produce cross-sectional images of the eyeball. While not commonly used as a first-line diagnostic tool for RVO, B-scan ultrasonography can be useful when media opacities, such as cataracts or vitreous hemorrhage, obscure the view of the retina.
B-scan ultrasonography can reveal important information about the eye’s overall structure, such as the presence of vitreous hemorrhage, retinal detachment, or other complications related to RVO. It is especially useful in cases of CRVO with extensive vitreous hemorrhage, where direct vision of the retina is difficult.
Blood Tests and Systematic Evaluation
Given the strong link between RVO and systemic vascular conditions, patients with RVO frequently require a comprehensive systemic evaluation. Blood tests may include a complete blood count (CBC), lipid profile, blood glucose levels, and coagulation studies to look for underlying risk factors like hyperlipidemia, diabetes, and hypercoagulability.
In younger patients or those with no obvious systemic risk factors, additional testing for systemic inflammatory conditions, autoimmune disorders, or blood clotting abnormalities may be required. Referral to a primary care physician, endocrinologist, or hematologist may be necessary to manage these underlying conditions.
Treatment Options for Retinal Vein Occlusion
Managing retinal vein occlusion (RVO) entails identifying the underlying cause, treating symptoms, avoiding complications, and preserving vision. The type of RVO (BRVO or CRVO), the severity of the condition, and the presence of complications such as macular edema or neovascularization all influence the treatment strategy. Early and proactive management is critical for achieving optimal visual outcomes and avoiding permanent vision loss.
Observation and Monitoring
In some cases, especially in mild or non-ischemic forms of RVO, initial treatment may include observation and regular monitoring. This approach is appropriate for patients with mild symptoms, no significant macular edema, and a low risk of complications. Patients under observation are closely monitored with regular eye exams, including visual acuity tests, optical coherence tomography (OCT), and fluorescein angiography (FA), to detect any changes in the retina that may necessitate intervention.
Monitoring is also important for non-ischemic CRVO because it can sometimes progress to ischemic CRVO, which is more likely to cause complications. If the condition worsens, or if macular edema or neovascularization appear, more aggressive treatment may be required.
Anti-VEGF Therapies
Anti-vascular endothelial growth factor (anti-VEGF) therapy is the primary treatment for RVO-related macular edema and neovascularization. Anti-VEGF medications, including ranibizumab (Lucentis), bevacizumab (Avastin), and aflibercept (Eylea), work by inhibiting VEGF, a protein that promotes the formation of abnormal blood vessels and increases vascular permeability. These drugs reduce VEGF levels, which helps reduce macular edema, prevent the progression of neovascularization, and stabilize or improve vision.
Anti-VEGF therapy is typically administered via intravitreal injections, which are injections made directly into the vitreous cavity of the eye. The treatment regimen typically begins with monthly injections, followed by a maintenance phase in which the frequency of injections may be reduced based on the patient’s response.
According to studies, anti-VEGF therapy improves visual acuity and reduces macular edema in patients with both BRVO and CRVO. However, because the effects of anti-VEGF therapy are only temporary, continued treatment and regular monitoring are required to maintain
the benefits.
Corticosteroid Injections
Intravitreal corticosteroid injections are another option for treating RVO-related macular edema. Corticosteroids, such as triamcinolone acetonide and dexamethasone, are anti-inflammatory drugs that can reduce vascular permeability, lowering macular edema and improving vision.
The dexamethasone intravitreal implant (Ozurdex) is an FDA-approved sustained-release corticosteroid implant for treating macular edema after RVO. The implant delivers the drug in a controlled manner over several months, reducing the need for frequent injections.
Corticosteroid injections can be effective, but they may cause increased intraocular pressure, cataract formation, and infection. As a result, corticosteroids are frequently reserved for patients who do not respond well to anti-VEGF therapy or have contraindications to anti-VEGF treatment.
Laser Photocoagulation
Laser photocoagulation is a treatment option for BRVO that aims to manage macular edema and prevent neovascularization. The procedure involves applying laser energy to the retina to cause small burns around areas of capillary leakage or ischemia. This helps to seal leaking blood vessels, reduce macular edema, and prevent the formation of new, abnormal blood vessels.
Grid laser photocoagulation is a specific technique for treating macular edema in BRVO. In this procedure, the laser is used in a grid pattern over the macular edema area to target capillary leakage. Laser photocoagulation is generally less effective in CRVO due to the diffuse nature of retinal involvement and the increased risk of complications like neovascular glaucoma.
Management of Complications
In addition to treating the underlying condition, managing complications associated with RVO is critical for maintaining vision and preventing further damage. The following are some of the key complications and how to manage them:
- Neovascularization: If neovascularization occurs, immediate treatment with anti-VEGF therapy or laser photocoagulation is required to avoid complications such as vitreous hemorrhage and neovascular glaucoma. In severe cases, surgical intervention may be necessary.
- Neovascular Glaucoma: This severe complication necessitates aggressive treatment, such as anti-VEGF therapy to reduce neovascularization, laser treatment to reduce intraocular pressure, and, in some cases, surgical interventions such as trabeculectomy or the implantation of a glaucoma drainage system.
- Vitreous Hemorrhage: If the vitreous hemorrhage is mild and likely to resolve on its own, patients with it may benefit from observation. However, in severe or persistent hemorrhage, vitrectomy surgery may be required to remove the blood and avoid retinal detachment.
- Retinal Detachment: Retinal detachment necessitates immediate surgical intervention to reconnect the retina and prevent permanent vision loss. The surgical approach may include scleral buckling, vitrectomy, or pneumatic retinopexy, depending on the severity and location of the detachment.
Systematic Management
Given the strong link between RVO and systemic vascular conditions, treating the underlying systemic risk factors is an important part of management. Patients with RVO should have a comprehensive cardiovascular evaluation to detect and treat conditions such as hypertension, diabetes, hyperlipidemia, and other risk factors. Lifestyle changes, such as quitting smoking, managing weight, and exercising regularly, are also important in lowering the risk of recurrent RVO and other cardiovascular events.
Collaboration with the patient’s primary care physician, cardiologist, or endocrinologist may be required to improve systemic management and lower the overall risk of vascular complications.
Trusted Resources and Support
Books
- “Retina” by Stephen J. Ryan – This comprehensive textbook provides detailed coverage of retinal diseases, including retinal vein occlusion, with a focus on diagnosis, management, and treatment options.
- “Medical Retina: Focus on Vascular and Inflammatory Diseases” by Frank G. Holz and Richard F. Spaide – This book offers in-depth insights into vascular retinal diseases, including RVO, with a focus on modern diagnostic techniques and therapeutic strategies.
Organizations
- American Academy of Ophthalmology (AAO) – The AAO offers extensive resources for both patients and healthcare professionals, including clinical guidelines, patient education materials, and the latest research on retinal vein occlusion and other retinal conditions.
- National Eye Institute (NEI) – The NEI provides valuable information on eye health, including detailed resources on retinal vein occlusion, treatment options, and ongoing research into new therapies for retinal vascular diseases.






