The tongue is one of the most versatile and dynamic organs in the human body. Beyond its vital role in taste, it plays a key part in speech, mastication, swallowing, and even in protecting the oral cavity from pathogens. With its intricate muscular structure, rich nerve supply, and specialized sensory receptors, the tongue helps us savor flavors and articulate language. This guide explores the detailed anatomy, diverse functions, common conditions, diagnostic techniques, and various treatment and lifestyle strategies to ensure optimal tongue health and overall oral well-being.
Table of Contents
- Anatomical Structure
- Microanatomy & Papillae
- Muscular Architecture
- Nerve and Blood Supply
- Lymph Drainage
- Physiological Functions
- Taste, Speech & Swallowing
- Additional Roles
- Common Tongue Disorders
- Diagnostic Methods
- Treatment Approaches
- Supplements for Tongue Health
- Lifestyle & Maintenance Tips
- Trusted Resources
- Frequently Asked Questions
- Disclaimer & Sharing
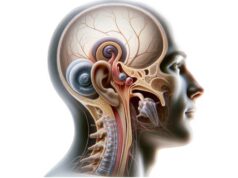
Anatomical Structure
The tongue is a muscular organ located in the oral cavity, playing essential roles in tasting, speaking, and manipulating food. It is divided into three main parts: the apex (tip), the body, and the base (root). The surface of the tongue is covered with a variety of papillae that contain taste buds and sensory receptors. These structures not only aid in the detection of flavors but also contribute to the texture that facilitates food manipulation during mastication. The tongue’s flexible and highly vascular structure is critical for its multifaceted functions, making it a key organ in both digestion and communication.
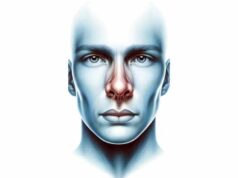
Microanatomy & Papillae
At the microscopic level, the tongue exhibits a complex structure that underpins its sensory and motor functions.
Papillae Types
- Filiform Papillae:
These are the most numerous and provide the tongue with its rough texture. Although they lack taste buds, they are crucial for gripping and manipulating food. - Fungiform Papillae:
Scattered across the tip and upper surface, these papillae house taste buds that detect sweet, sour, and salty flavors. - Circumvallate Papillae:
Larger and arranged in a V-shaped row at the back of the tongue, they are surrounded by trenches that contain numerous taste buds and are key to sensing bitter flavors. - Foliate Papillae:
Located on the sides of the tongue near the back, these papillae also contain taste buds and play a role in the perception of taste.
Epithelial Layers
The dorsal surface of the tongue is covered by a keratinized stratified squamous epithelium, particularly in areas subject to mechanical stress. In contrast, the ventral surface has a non-keratinized epithelium, which is thinner and more flexible. This specialized arrangement supports the tongue’s diverse functions, from withstanding the abrasion of food to enabling sensitive taste perception.
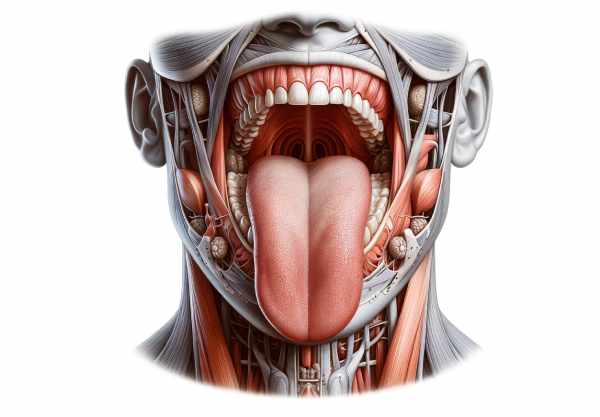
Muscular Architecture
The tongue is composed of a complex network of muscles that grant it extraordinary flexibility and control. Its muscular structure can be divided into two main groups:
Intrinsic Muscles
These muscles are completely contained within the tongue and are responsible for altering its shape. They include:
- Superior Longitudinal Muscle:
Elevates the tongue tip and helps in curling the tongue upward. - Inferior Longitudinal Muscle:
Pulls the tongue tip downward. - Transverse Muscle:
Narrows and elongates the tongue. - Vertical Muscle:
Flattens and broadens the tongue.
These intrinsic muscles work in concert to enable intricate movements necessary for speech articulation and food manipulation.
Extrinsic Muscles
These muscles originate outside the tongue and insert into it, enabling gross movements such as protrusion, retraction, and lateral movements. Key extrinsic muscles include:
- Genioglossus:
Protrudes and depresses the tongue, playing a crucial role in speech and swallowing. - Hyoglossus:
Depresses and retracts the tongue. - Styloglossus:
Elevates and retracts the tongue, essential for proper articulation. - Palatoglossus:
Elevates the posterior portion of the tongue, aiding in swallowing and closing the oropharyngeal isthmus.
The intricate interplay between intrinsic and extrinsic muscles allows the tongue to perform a wide range of movements, making it indispensable for both culinary and communicative functions.
Nerve and Blood Supply
The tongue’s remarkable functionality is supported by a dense network of nerves and an abundant blood supply.
Nerve Supply
- Motor Innervation:
The hypoglossal nerve (cranial nerve XII) provides motor innervation to almost all intrinsic and extrinsic muscles of the tongue, except the palatoglossus, which is innervated by the vagus nerve (cranial nerve X). - Sensory Innervation:
- General Sensation:
The anterior two-thirds of the tongue receive general sensory input from the lingual nerve, a branch of the mandibular division of the trigeminal nerve (cranial nerve V3), while the posterior one-third is supplied by the glossopharyngeal nerve (cranial nerve IX). - Taste Sensation:
Taste from the anterior two-thirds is transmitted by the chorda tympani, a branch of the facial nerve (cranial nerve VII), and the posterior one-third by the glossopharyngeal nerve. The base of the tongue also receives taste sensation from the internal laryngeal branch of the vagus nerve.
Blood Supply
- Arterial Supply:
The tongue is primarily supplied by the lingual artery, a branch of the external carotid artery. The lingual artery divides into branches such as the dorsal lingual and deep lingual arteries, ensuring that the entire tongue receives an adequate blood supply. - Venous Drainage:
Venous return is achieved through the lingual veins, which drain into the internal jugular vein, maintaining efficient blood flow and nutrient delivery.
Lymphatic Drainage
Lymphatic drainage of the tongue is essential for immune surveillance and the clearance of waste products.
- Anterior Tip:
Lymph from the tip of the tongue drains into the submental lymph nodes. - Lateral Margins:
The sides of the tongue drain primarily to the submandibular lymph nodes. - Central and Base:
The central and posterior parts of the tongue drain into the deep cervical lymph nodes.
This network not only supports immune function but also plays a significant role in the metastasis of oral cancers.
Physiological Functions
The tongue is integral to several vital functions that affect our daily lives, from tasting food to forming speech.
Taste Perception
Taste is one of the primary sensory functions of the tongue. Taste buds housed in various papillae on the tongue detect the five basic taste modalities: sweet, sour, salty, bitter, and umami. When food molecules interact with these taste receptors, they generate signals that are transmitted to the brain, allowing us to discern flavors. This sensory function not only enhances the pleasure of eating but also helps in identifying nutritious foods and avoiding harmful substances.
Speech Articulation
The tongue plays a crucial role in the production of speech. Its intricate and precise movements, controlled by both intrinsic and extrinsic muscles, allow for the formation of distinct sounds and words. By shaping the oral cavity and modulating airflow, the tongue contributes to the clarity, tone, and modulation of speech, making effective communication possible.
Mastication and Swallowing
During mastication (chewing), the tongue positions food between the teeth and mixes it with saliva, which contains enzymes crucial for digestion. Once the food is adequately chewed, the tongue propels it into the oropharynx, initiating the swallowing process. This coordinated action is vital for efficient digestion and preventing choking by ensuring that food enters the esophagus rather than the airway.
Sensory Feedback and Proprioception
The tongue provides essential sensory feedback regarding the texture, temperature, and consistency of food. This feedback is critical for fine motor control during eating and speech. Proprioceptive receptors in the tongue help the brain gauge its position and movement, enabling smooth coordination with other oral structures.
Immune Defense
The tongue, especially at its base, houses the lingual tonsils, which are part of the body’s immune system. These structures play a role in the initial immune defense by capturing and processing pathogens that enter the oral cavity, contributing to overall systemic immunity.
Common Tongue Disorders
Various conditions can affect the tongue, impacting its appearance, function, and overall oral health. Early diagnosis and proper treatment are essential to prevent complications.
Geographic Tongue
Geographic tongue, or benign migratory glossitis, is characterized by red, smooth patches on the tongue that resemble maps. These patches often have irregular, white borders and may change in shape and location over time. Although the condition is benign, it can cause discomfort or sensitivity to certain foods.
Symptoms:
- Red, smooth areas on the tongue with white borders
- Occasional discomfort or sensitivity, especially to spicy or acidic foods
Treatment:
- No treatment is usually necessary, though avoiding irritants can reduce discomfort.
- Topical corticosteroids or antihistamines may be used for symptomatic relief.
Glossitis
Glossitis refers to inflammation of the tongue, which can be caused by infections, nutritional deficiencies, allergies, or irritants. The condition may result in a swollen, red, and smooth tongue.
Symptoms:
- Swelling and redness of the tongue
- Pain or tenderness, sometimes accompanied by difficulty swallowing
- Changes in taste perception
Treatment:
- Treat the underlying cause (e.g., nutritional supplements for deficiencies, antibiotics for bacterial infections).
- Avoid irritants such as tobacco, alcohol, and spicy foods.
- Use anti-inflammatory medications to alleviate pain and swelling.
Thrush (Oral Candidiasis)
Thrush is a fungal infection caused by an overgrowth of Candida species, most commonly Candida albicans. It typically affects the tongue and inner cheeks, resulting in white, creamy lesions.
Symptoms:
- White, curd-like patches on the tongue and other areas of the mouth
- Redness, soreness, and a cottony sensation in the mouth
- Difficulty swallowing in severe cases
Treatment:
- Antifungal medications (e.g., nystatin, clotrimazole, or fluconazole)
- Maintain good oral hygiene and manage underlying conditions that may predispose to fungal overgrowth.
Tongue Tie (Ankyloglossia)
Tongue tie is a congenital condition where the lingual frenulum is unusually short or thick, restricting tongue movement. This can interfere with breastfeeding in infants and may contribute to speech difficulties later in life.
Symptoms:
- Limited tongue mobility
- Difficulty breastfeeding in infants
- Speech impediments in older children
Treatment:
- For mild cases, observation and speech therapy may suffice.
- Severe cases often require surgical intervention (frenotomy or frenuloplasty) to release the frenulum and improve tongue mobility.
Leukoplakia
Leukoplakia presents as thick, white patches on the tongue or other areas of the oral cavity that cannot be scraped off. While often benign, these patches can sometimes be precancerous.
Symptoms:
- Persistent white patches on the tongue
- Mild discomfort or sensitivity in the affected area
- Potential changes in texture or appearance
Treatment:
- Eliminate irritants such as tobacco and alcohol.
- Regular monitoring and biopsy of lesions to rule out malignancy.
- Surgical removal or laser therapy may be indicated for persistent or suspicious lesions.
Oral Cancer
Oral cancer can develop on the tongue and poses significant health risks if not diagnosed early. Risk factors include tobacco use, alcohol consumption, HPV infection, and prolonged exposure to other carcinogens.
Symptoms:
- A persistent sore or ulcer on the tongue
- White or red patches that do not heal
- Pain, numbness, or bleeding from the tongue
- Difficulty speaking or swallowing
Treatment:
- Treatment typically involves surgical excision of the tumor, often combined with radiation therapy or chemotherapy.
- Early diagnosis through self-examination and medical evaluation is critical for improving outcomes.
Burning Mouth Syndrome (BMS)
Burning mouth syndrome is a chronic condition characterized by a burning sensation in the tongue or other parts of the mouth without an obvious cause. It is more common in postmenopausal women and may be linked to dry mouth, nutritional deficiencies, or psychological factors.
Symptoms:
- Persistent burning sensation in the tongue or entire mouth
- Altered taste perception
- Dry mouth and discomfort that worsens throughout the day
Treatment:
- Address underlying conditions such as nutritional deficiencies or dry mouth.
- Medications such as antidepressants, anticonvulsants, or topical capsaicin may provide relief.
- Stress management and psychological support are also beneficial.
Black Hairy Tongue
Black hairy tongue is a benign condition characterized by an abnormal elongation and discoloration of the filiform papillae, giving the tongue a hairy appearance.
Symptoms:
- Discolored (black or brown) and hairy appearance on the dorsal surface of the tongue
- Bad breath or altered taste
- Generally painless, though aesthetic concerns may arise
Treatment:
- Improved oral hygiene, including regular tongue scraping and brushing.
- Avoid risk factors such as tobacco, excessive coffee or tea, and certain medications.
- Antibacterial or antifungal mouthwashes may be used if infection is suspected.
Macroglossia
Macroglossia refers to an abnormally large tongue, which can be congenital or acquired. It may interfere with speech, swallowing, and breathing, and is sometimes associated with conditions such as hypothyroidism, amyloidosis, or acromegaly.
Symptoms:
- Enlarged tongue that may protrude from the mouth
- Difficulty speaking, chewing, or swallowing
- Drooling and dental malocclusion
Treatment:
- Treat the underlying cause (e.g., hormone therapy for hypothyroidism).
- Speech therapy and orthodontic interventions can help manage functional problems.
- In severe cases, surgical reduction (glossectomy) may be considered.
Diagnostic Methods
Accurate diagnosis of tongue disorders involves a comprehensive approach combining clinical evaluation, laboratory tests, imaging, and sometimes biopsy procedures.
Clinical Examination
- Visual Inspection:
The clinician carefully examines the tongue for color changes, lesions, swelling, or unusual textures. This initial observation helps detect conditions such as geographic tongue, leukoplakia, or oral thrush. - Palpation:
Gently palpating the tongue can help identify masses, cysts, or areas of tenderness. - Medical History:
A detailed history including symptom onset, duration, dietary habits, tobacco or alcohol use, and systemic conditions guides the diagnosis.
Laboratory Tests
- Microbial Cultures:
Swabbing and culturing lesions can identify bacterial, fungal, or viral infections, particularly useful in diagnosing thrush or glossitis. - Blood Tests:
Evaluations such as complete blood count (CBC), vitamin B12, iron levels, and inflammatory markers (ESR, CRP) can reveal nutritional deficiencies or systemic infections that contribute to tongue disorders. - Serologic Tests:
In cases of suspected autoimmune conditions, antibody tests may be conducted.
Imaging Techniques
- Ultrasonography:
Non-invasive ultrasound imaging can assess the structure of the tongue, detect masses or cysts, and evaluate vascular flow. - Magnetic Resonance Imaging (MRI):
MRI offers high-resolution images of the tongue and surrounding tissues, helping to differentiate between benign and malignant lesions. - Computed Tomography (CT) Scan:
CT imaging provides cross-sectional views of the tongue, useful for assessing deep tissue involvement, especially in suspected cases of oral cancer.
Biopsy and Cytology
- Fine-Needle Aspiration (FNA) Biopsy:
FNA involves extracting cells from a suspicious lesion for cytological examination, particularly useful for diagnosing cancer or persistent leukoplakia. - Incisional Biopsy:
In cases where FNA is inconclusive, a small tissue sample is surgically removed for histopathological analysis. - Exfoliative Cytology:
Scraping cells from the tongue’s surface can help diagnose superficial lesions such as candidiasis or precancerous changes.
Functional Tests
- Speech Evaluation:
A speech-language pathologist may assess tongue function during articulation, especially in cases of tongue tie or macroglossia. - Swallowing Study:
Videofluoroscopic swallowing studies help evaluate the tongue’s role in bolus formation and safe swallowing. - Taste Tests:
Taste strip tests or solutions are used to assess the function of taste buds, important in diagnosing conditions that affect taste perception.
Treatment Approaches
The treatment of tongue disorders varies widely depending on the underlying cause and severity. Approaches range from conservative management to surgical intervention.
Conservative Management
Oral Hygiene and Self-Care
- Maintain Good Oral Hygiene:
Brush your teeth and tongue at least twice a day using a soft-bristled toothbrush or tongue scraper to remove debris and bacteria. - Hydration:
Drinking plenty of water ensures adequate saliva production, which protects the tongue and aids in digestion. - Dietary Modifications:
Avoid irritating foods such as spicy, acidic, or overly hot foods if you have a sensitive or inflamed tongue.
Medications
- Topical Treatments:
For conditions like glossitis or burning mouth syndrome, topical corticosteroids or anesthetic gels can provide relief. - Antifungal and Antibacterial Agents:
In cases of thrush or bacterial infections, appropriate antifungal or antibiotic treatments are prescribed. - Nutritional Supplements:
For nutritional deficiencies causing tongue inflammation, supplementation with vitamin B12, iron, and vitamin C may be recommended.
Behavioral and Supportive Therapies
- Speech Therapy:
For conditions such as tongue tie or macroglossia that affect speech, speech therapy can help improve articulation. - Stress Management:
Techniques such as mindfulness, yoga, and meditation can help alleviate symptoms of burning mouth syndrome and other stress-related tongue conditions.
Surgical Interventions
Corrective Surgery
- Frenotomy/Frenuloplasty:
For tongue tie (ankyloglossia), surgical procedures like frenotomy (simple snipping) or frenuloplasty (more complex tissue repositioning) release the tight frenulum and improve mobility. - Lesion Excision:
Persistent or suspicious lesions, such as those seen in leukoplakia or oral cancer, may require surgical excision, often followed by adjunctive therapies. - Glossectomy:
In severe cases of oral cancer, a partial or total glossectomy (removal of part or all of the tongue) may be necessary, followed by reconstructive surgery and rehabilitation.
Minimally Invasive Procedures
- Laser Therapy:
Laser treatments can be used to remove precancerous lesions or reduce inflammation in certain tongue conditions with minimal recovery time. - Cryotherapy:
This treatment uses extreme cold to destroy abnormal tissues, particularly in the management of leukoplakia or small benign lesions.
Rehabilitation & Recovery
Physical and Occupational Therapy
- Post-Surgical Rehabilitation:
Following surgical interventions, physical therapy may be necessary to restore tongue mobility, improve speech, and aid in swallowing. - Exercises:
Specific exercises to strengthen and improve coordination of the tongue muscles can be crucial in recovery and maintaining long-term function.
Follow-Up Care
- Regular Monitoring:
Frequent check-ups with healthcare professionals are essential to monitor recovery, adjust treatments, and prevent recurrence of conditions. - Lifestyle Adjustments:
Continued adherence to good oral hygiene and dietary practices is important to maintain long-term tongue health.
Supplements for Tongue Health
Several supplements can support the health of the tongue and overall oral health by reducing inflammation, promoting tissue repair, and enhancing immune function.
Vitamins and Minerals
- Vitamin B12:
Crucial for maintaining healthy nerve cells and preventing glossitis. Supplementation is particularly important for vegetarians and older adults. - Iron:
Supports red blood cell production and helps prevent anemia-related glossitis. Iron supplementation can alleviate symptoms associated with deficiency. - Vitamin C:
An antioxidant that promotes collagen synthesis and protects mucosal tissues. Adequate vitamin C intake can support oral tissue health. - Zinc:
Essential for immune function and wound healing, zinc helps maintain the integrity of the tongue’s epithelium. - Vitamin D:
Plays a role in immune modulation and overall tissue health, indirectly supporting the oral mucosa.
Herbal Supplements
- Aloe Vera:
Known for its soothing and anti-inflammatory properties, aloe vera can alleviate symptoms of glossitis and oral irritation. - Licorice Root:
With antimicrobial and anti-inflammatory effects, licorice root can help reduce inflammation and combat infections. - Turmeric (Curcumin):
Possessing potent anti-inflammatory and antioxidant properties, curcumin can help mitigate inflammation and promote healing in tongue conditions.
Enzymes
- Papain:
An enzyme derived from papaya, papain helps reduce inflammation and supports tissue repair, beneficial for conditions like glossitis. - Bromelain:
Found in pineapple, bromelain has anti-inflammatory properties that can ease pain and swelling in tongue disorders.
Omega-3 Fatty Acids
- Fish Oil and Flaxseed Oil:
Rich in omega-3 fatty acids, these supplements reduce systemic inflammation and support cell membrane integrity, promoting oral and tongue health.
Antioxidants
- Alpha-Lipoic Acid:
A powerful antioxidant that protects tongue tissues from oxidative stress and supports cellular repair. - Resveratrol:
Found in grapes and berries, resveratrol’s antioxidant properties help reduce inflammation and enhance oral tissue health.
Lifestyle & Dietary Practices for Tongue Health
Maintaining optimal tongue health requires a comprehensive approach that combines proper oral hygiene, balanced nutrition, and healthy lifestyle habits.
Oral Hygiene
- Regular Brushing:
Brush your teeth and tongue twice daily using a soft-bristled toothbrush to remove plaque, bacteria, and debris from the tongue surface. - Tongue Scraping:
Use a tongue scraper daily to eliminate buildup and reduce bad breath. - Mouth Rinses:
Antibacterial or antifungal mouthwashes can help prevent and treat infections such as thrush.
Nutrition and Hydration
- Balanced Diet:
A diet rich in fruits, vegetables, lean proteins, and whole grains provides the essential vitamins and minerals needed for oral tissue health. - Hydration:
Drinking plenty of water supports saliva production, which is crucial for maintaining a healthy oral environment and preventing dry mouth. - Avoid Irritants:
Reduce intake of overly spicy, acidic, or hot foods that can irritate the tongue’s surface.
Stress and Lifestyle
- Stress Management:
Incorporate stress-reduction techniques such as meditation, yoga, and deep breathing exercises, as chronic stress can worsen conditions like burning mouth syndrome. - Avoid Tobacco and Excessive Alcohol:
Both smoking and heavy alcohol consumption can damage oral tissues and increase the risk of tongue disorders. - Regular Dental Check-Ups:
Schedule routine dental visits to monitor oral health and detect early signs of any tongue-related issues.
Additional Considerations
- Healthy Habits:
Avoid biting or chewing on the tongue, and use protective gear if you grind your teeth at night. - Sleep:
Ensure adequate sleep to support overall tissue repair and immune function. - Environmental Toxins:
Limit exposure to chemicals and pollutants that may irritate the oral mucosa.
Trusted Resources for Tongue Health
For further information on tongue health and related conditions, consider these reputable sources that offer evidence-based guidance and educational material.
Books
- “Oral Pathology: Clinical Pathologic Correlations” by Joseph A. Regezi, James J. Sciubba, and Richard C. K. Jordan
Provides comprehensive coverage of oral pathology, including disorders that affect the tongue, with clinical correlations and case studies. - “Burket’s Oral Medicine” by David L. Mills and Michael Glick
A detailed reference that covers various aspects of oral health, including diagnosis and treatment of tongue conditions. - “Oral Medicine and Pathology: A Clinical Guide” by Dimitrios G. Kastrinakis and Panagiotis Skandalakis
Offers in-depth insights into oral diseases, including tongue disorders, and provides practical diagnostic and treatment guidelines.
Academic Journals
- Journal of Oral Pathology & Medicine:
Features peer-reviewed research on oral diseases, including tongue conditions, with a focus on pathology, diagnosis, and management. - Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology:
Publishes studies and reviews on a wide range of oral health topics, including comprehensive analyses of tongue disorders and treatment methods.
Mobile Apps
- Oral-B:
An app designed to improve oral hygiene through guided brushing routines, reminders, and educational tips, including tongue care. - MyDentalCare:
Offers tools to track dental health, schedule appointments, and access information on maintaining optimal oral hygiene. - SmartMouth:
Provides personalized oral care recommendations and reminders for regular oral hygiene practices to promote overall oral health.
Frequently Asked Questions
What is the primary function of the tongue?
The tongue is essential for taste, speech, mastication, and swallowing. It helps to detect flavors, articulate words, manipulate food during chewing, and assist in forming a cohesive bolus for safe swallowing.
How does the tongue contribute to taste?
Taste buds located on various papillae of the tongue detect five basic tastes: sweet, sour, salty, bitter, and umami. These sensory signals are transmitted to the brain, where they are interpreted as distinct flavors.
What causes geographic tongue?
Geographic tongue is a benign condition characterized by irregular red patches with white borders. Its exact cause is unknown, but genetics and associations with other conditions like psoriasis may play a role. It is generally harmless and often requires no treatment.
How is tongue tie treated?
Tongue tie, or ankyloglossia, may be treated with a simple frenotomy or, in more complex cases, a frenuloplasty to release the tight frenulum and improve tongue mobility, particularly if it interferes with speech or feeding.
What lifestyle habits support tongue health?
Maintaining good oral hygiene, staying hydrated, eating a balanced diet rich in vitamins and antioxidants, managing stress, and avoiding tobacco and excessive alcohol are key habits that support the health of the tongue and overall oral well-being.
Disclaimer & Sharing
The information provided in this article is for educational purposes only and should not be considered a substitute for professional medical advice. Always consult with a qualified healthcare provider for personalized diagnosis and treatment recommendations.
If you found this guide helpful, please share it on Facebook, X (formerly Twitter), or your preferred social platform to help spread awareness and promote tongue health.