The tonsils are vital lymphoid tissues forming part of Waldeyer’s ring—a collection of immune structures located at the entrance to the respiratory and digestive tracts. They play an essential role in protecting the body from airborne and ingested pathogens by trapping antigens and facilitating the development of immune responses. In addition to their immune function, the tonsils are involved in the early development of immunological memory. However, due to their constant exposure to external pathogens, they are prone to various conditions ranging from simple infections to chronic inflammation and even neoplasms. This in-depth guide covers the detailed anatomy, physiology, common disorders, diagnostic methods, treatment options, and lifestyle tips for maintaining optimal tonsil health.
Table of Contents
- Anatomical Structure
- Types of Tonsils
- Histological Features
- Vascular Supply & Innervation
- Lymphatic Drainage
- Development & Variations
- Physiological Functions
- Common Disorders
- Diagnostic Methods
- Management and Treatment
- Supplements for Tonsil Health
- Lifestyle & Maintenance Tips
- Trusted Resources
- Frequently Asked Questions
- Disclaimer & Sharing
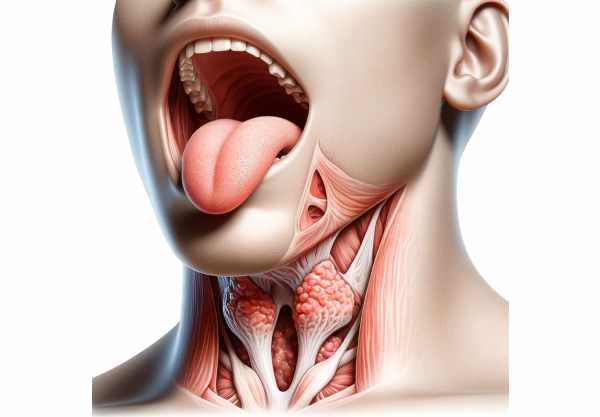
Anatomical Structure
The tonsils are collections of lymphoid tissue strategically located in the pharynx, serving as a first line of immune defense. They form part of Waldeyer’s ring—a circular arrangement of lymphoid tissue that includes the palatine tonsils, adenoids (pharyngeal tonsils), lingual tonsils, and tubal tonsils. Each type of tonsil occupies a specific anatomical location and performs unique functions in immune surveillance. Their positions at the gateway of the respiratory and digestive systems enable them to intercept pathogens entering the body, triggering immune responses that protect against infection and disease.
Types of Tonsils
Tonsils are not a single organ but a group of lymphoid tissues with varied locations and functions:
- Palatine Tonsils:
Located on either side of the oropharynx between the palatoglossal and palatopharyngeal arches, these are the most well-known tonsils and are easily visible when the mouth is open. They contain deep crypts that increase their surface area for antigen trapping. - Pharyngeal Tonsils (Adenoids):
Situated in the nasopharynx, adenoids are not visible during a standard oral examination. They play a key role in filtering air and protecting against inhaled pathogens, particularly in children. - Lingual Tonsils:
Found at the base of the tongue, these tonsils are less prominent but still contribute significantly to the immune defense of the oral cavity. - Tubal Tonsils:
Located near the openings of the Eustachian tubes in the nasopharynx, these small collections of lymphoid tissue help protect the middle ear from infections.
Each type has distinct anatomical and histological features that tailor it to its specific role in immune surveillance and response.
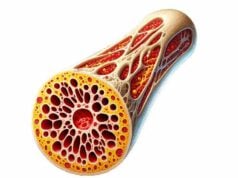
Histological Features
The microscopic structure of the tonsils reveals their complex role in immunity:
- Lymphoid Follicles:
The core of the tonsils consists of lymphoid follicles with germinal centers where B cells proliferate, differentiate, and undergo class-switch recombination to produce high-affinity antibodies. - Epithelial Covering:
The tonsils are lined by stratified squamous epithelium. In the palatine tonsils, this epithelium extends into deep crypts, increasing the area for antigen exposure and immune cell interaction. - Immune Cells:
Both T and B lymphocytes are abundant within tonsillar tissue. Macrophages and dendritic cells are also present, aiding in antigen presentation and the removal of apoptotic cells. - Interfollicular Regions:
These areas are rich in T cells, facilitating the interaction between T cells and antigen-presenting cells, which is crucial for developing a robust immune response.
The combination of these features creates an environment where pathogens can be efficiently detected, processed, and responded to.
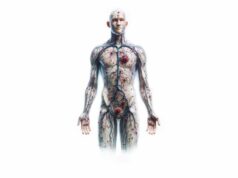
Vascular Supply & Innervation
The tonsils receive a rich blood supply and are well innervated, which supports their immune functions and contributes to their role in the body’s defense mechanisms.
Blood Supply
- Arterial Supply:
The tonsils are supplied by several branches of the external carotid artery, including the ascending palatine artery, the tonsillar branch of the facial artery, and the ascending pharyngeal artery. This extensive vascular network ensures a robust delivery of oxygen and immune cells. - Venous Drainage:
Venous blood from the tonsils drains into the peritonsillar plexus and then into the internal jugular vein, facilitating efficient removal of metabolic waste and inflammatory mediators.
Innervation
- Sensory Innervation:
The glossopharyngeal nerve (cranial nerve IX) and branches of the vagus nerve (cranial nerve X) provide sensory input, allowing the tonsils to detect pain, temperature, and touch. - Autonomic Innervation:
The sympathetic nervous system modulates blood flow and may influence immune function within the tonsils. This neural input plays a role in the overall regulation of tonsillar activity.
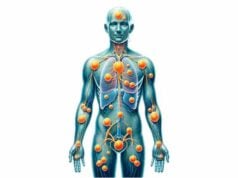
Lymphatic Drainage
The tonsils have an extensive lymphatic network that facilitates the transport of immune cells and the clearance of pathogens:
- Lymphatic Channels:
Lymph from the tonsils is drained by numerous small lymphatic vessels that converge into larger channels. - Regional Lymph Nodes:
The primary lymph nodes involved in tonsillar drainage are the jugulodigastric lymph nodes, located along the internal jugular vein. These nodes filter lymph and trap antigens, playing a crucial role in initiating immune responses.
This efficient lymphatic drainage is essential for maintaining a robust immune defense in the head and neck region.
Development & Variations
Tonsils develop from the embryonic pharyngeal pouches and undergo significant changes during childhood:
- Embryological Origin:
The palatine tonsils arise from the second pharyngeal pouch, while the adenoids and lingual tonsils originate from the third and fourth pouches, respectively. - Growth and Maturation:
Tonsils are most active in early childhood, contributing significantly to the development of the immune system. They typically reach their maximum size during childhood and gradually involute during adolescence and adulthood. - Variations:
Anatomical variations, such as differences in size or the presence of accessory tonsillar tissue, are common. Congenital anomalies like ectopic tonsillar tissue or persistent thyroglossal duct remnants can also occur.
Understanding these developmental patterns is important for diagnosing congenital conditions and planning appropriate interventions.
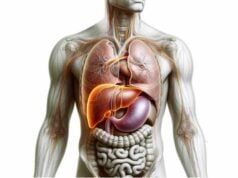
Physiological Functions
The tonsils are integral components of the immune system, performing several critical functions that protect the body against infection:
Immune Surveillance
The tonsils are strategically positioned at the gateway to the respiratory and digestive tracts, where they continuously sample and filter antigens from inhaled or ingested substances. This constant exposure to pathogens primes the immune system for rapid response.
Antigen Presentation and Lymphocyte Activation
- Antigen Capture:
Specialized cells, including dendritic cells and macrophages within the tonsils, capture antigens and present them to T cells. - Lymphocyte Activation:
The tonsillar follicles serve as sites for the activation and proliferation of B lymphocytes, leading to the production of high-affinity antibodies. - Establishing Immune Memory:
By fostering the development of memory B and T cells, the tonsils contribute to long-lasting immunity against recurrent infections.
Secretory IgA Production
Tonsillar tissue produces secretory immunoglobulin A (IgA), a critical antibody that protects mucosal surfaces by neutralizing pathogens and preventing their adherence to the mucous membranes.
Oral Tolerance
The tonsils also play a role in developing oral tolerance, a mechanism that prevents overreaction to harmless substances like food proteins and commensal bacteria, thereby maintaining immune homeostasis.
Common Tonsil Disorders
Due to their constant exposure to environmental pathogens, the tonsils are prone to various disorders that can impact both local and systemic health.
Tonsillitis
Tonsillitis is an inflammation of the tonsils, commonly caused by viral or bacterial infections.
- Acute Tonsillitis:
Characterized by sudden onset of sore throat, fever, red and swollen tonsils, and sometimes white or yellow exudate. - Chronic Tonsillitis:
Recurrent or persistent tonsillar inflammation, leading to chronic sore throat, bad breath, and enlarged cervical lymph nodes. - Recurrent Tonsillitis:
Multiple episodes per year may indicate the need for surgical intervention such as tonsillectomy.
Peritonsillar Abscess
A peritonsillar abscess, or quinsy, is a complication of tonsillitis where a pus-filled cavity forms near the tonsils.
- Symptoms:
Severe throat pain (often unilateral), difficulty swallowing, muffled voice, and trismus. - Treatment:
Requires drainage (via needle aspiration or incision and drainage) and antibiotic therapy.
Tonsil Stones (Tonsilloliths)
Tonsil stones are calcified debris that accumulate in the crypts of the tonsils.
- Symptoms:
Bad breath, a sensation of something stuck in the throat, and occasional discomfort. - Treatment:
Improved oral hygiene, tongue scraping, and in persistent cases, laser cryptolysis or tonsillectomy may be recommended.
Hypertrophic Tonsils
Enlarged tonsils, often seen in children, can lead to obstructive symptoms such as sleep apnea, difficulty swallowing, and recurrent infections.
- Symptoms:
Snoring, mouth breathing, and in severe cases, obstructive sleep apnea. - Treatment:
Observation, medical management, or tonsillectomy in cases causing significant airway obstruction.
Tonsillary Hyperplasia
A condition characterized by abnormal growth of tonsillar tissue, often in response to repeated infections.
- Symptoms:
Chronic sore throat, enlarged tonsils, and associated lymphadenopathy. - Treatment:
Conservative management for mild cases; tonsillectomy may be considered if symptoms are severe or recurrent.
Tonsil Cancer
Though less common, tonsil cancer is a serious condition typically associated with risk factors such as smoking, alcohol use, and HPV infection.
- Symptoms:
Persistent sore throat, a mass in the neck, difficulty swallowing, and changes in voice. - Treatment:
Surgical excision, radiation therapy, chemotherapy, or a combination of these, depending on the stage and type of cancer.
Adenoiditis
Inflammation of the adenoids, often associated with tonsillitis, especially in children.
- Symptoms:
Nasal obstruction, mouth breathing, snoring, and recurrent ear infections. - Treatment:
Antibiotics, nasal steroids, and, in chronic cases, adenoidectomy.
Diagnostic Methods
Diagnosing tonsil disorders requires a multifaceted approach combining clinical evaluation, laboratory tests, imaging, and sometimes biopsy procedures.
Clinical Examination
- Visual Inspection:
A thorough examination of the oral cavity and oropharynx using a light and tongue depressor to identify tonsillar enlargement, discoloration, exudates, and lesions. - Palpation:
Assessment of cervical lymph nodes to detect tenderness or enlargement, which may indicate infection or inflammation. - Medical History:
Detailed history including frequency of infections, duration of symptoms, and any associated systemic issues helps guide diagnosis.
Laboratory Tests
- Throat Swab Culture and RADT:
Used to identify bacterial infections, particularly Group A Streptococcus, which is a common cause of tonsillitis. - Complete Blood Count (CBC):
Helps detect signs of infection or inflammation. - Monospot and Viral Panels:
These tests are used to diagnose viral causes of tonsillitis, such as infectious mononucleosis.
Imaging Studies
- Ultrasound:
A non-invasive method to evaluate tonsillar size and detect abscess formation. - X-rays:
Lateral neck X-rays can help assess adenoidal hypertrophy, especially in children. - CT and MRI:
Advanced imaging modalities used to evaluate deep tissue involvement, assess the extent of masses, and plan surgical interventions.
Biopsy and Cytological Examination
- Fine-Needle Aspiration (FNA) Biopsy:
A minimally invasive procedure to extract cells from suspicious tonsillar lesions for cytological analysis. - Incisional/Excisional Biopsy:
Provides a larger tissue sample for histopathological examination, essential for diagnosing malignancies.
Functional Tests
- Polysomnography:
A sleep study used to diagnose obstructive sleep apnea associated with hypertrophic tonsils. - Swallowing and Speech Evaluations:
Assess the impact of tonsillar disorders on functions like swallowing and speech, guiding therapy decisions.
Management and Treatment
Effective management of tonsillar disorders involves tailored treatment strategies based on the underlying condition and symptom severity. Treatments range from conservative management and medications to surgical interventions and advanced therapies.
Medical Management
- Antibiotic Therapy:
Used for bacterial tonsillitis (e.g., streptococcal infections) to reduce symptoms and prevent complications. Typical antibiotics include penicillin, amoxicillin, or azithromycin. - Pain and Inflammation Relief:
Over-the-counter pain relievers such as acetaminophen or ibuprofen help manage fever and pain. Throat lozenges and topical anesthetic sprays provide additional symptomatic relief. - Anti-inflammatory Medications:
Corticosteroids may be prescribed in cases of severe inflammation or chronic tonsillitis to reduce swelling and pain.
Surgical Interventions
Tonsillectomy
- Indications:
Recurrent or chronic tonsillitis, obstructive sleep apnea, hypertrophy causing breathing difficulties, and tonsil cancer. - Techniques:
Various methods include cold knife dissection, electrocautery, harmonic scalpel, and coblation, each with specific advantages in reducing bleeding, pain, and recovery time. - Postoperative Care:
Includes pain management, dietary modifications (soft, cool foods), hydration, and rest. Follow-up appointments are essential to monitor healing.
Adenoidectomy
Often performed in conjunction with tonsillectomy in children with chronic adenoiditis or obstructive symptoms. It alleviates nasal obstruction and reduces the frequency of ear infections.
Abscess Drainage
For peritonsillar abscesses, drainage is critical:
- Needle Aspiration or Incision and Drainage:
These procedures remove pus and reduce infection, followed by antibiotic therapy.
Laser Tonsil Cryptolysis
A minimally invasive procedure used to treat tonsil stones by reducing the depth of tonsillar crypts, thus preventing the accumulation of debris.
Emerging Techniques
- Radiofrequency Ablation (RFA) and Cryotherapy:
These minimally invasive techniques reduce tonsil size and inflammation with less postoperative pain and faster recovery, especially beneficial for obstructive sleep apnea or chronic tonsillitis. - Photodynamic Therapy (PDT):
An emerging treatment for tonsil cancer that utilizes light-sensitive drugs activated by specific wavelengths to destroy malignant cells.
Supplemental & Nutritional Support for Tonsil Health
Optimal tonsil function and overall immune health can be enhanced through targeted nutritional support and supplementation.
Vitamins and Minerals
- Vitamin C:
An essential antioxidant that boosts immune function and supports tissue repair. It helps reduce the duration and severity of infections. - Zinc:
Critical for immune cell function, zinc aids in the healing of tonsillar tissue and can help reduce the incidence of infections. - Vitamin D:
Vital for immune modulation, adequate levels of vitamin D support the immune system and may reduce chronic inflammation. - Selenium:
Plays a role in antioxidant defense, protecting tonsillar tissue from oxidative stress.
Herbal Supplements
- Echinacea:
Known for its immune-enhancing properties, echinacea may reduce the severity and duration of infections affecting the tonsils. - Licorice Root:
With its anti-inflammatory and antimicrobial effects, licorice root can soothe inflamed tonsillar tissue and help combat infections. - Turmeric (Curcumin):
Offers strong anti-inflammatory and antioxidant benefits, which may alleviate chronic tonsillitis symptoms.
Probiotics
Maintaining a healthy gut microbiome supports overall immune function, indirectly benefiting the tonsils. Probiotic supplements and fermented foods like yogurt and kefir help maintain immune balance.
Antioxidants and Enzymes
- Alpha-Lipoic Acid:
A potent antioxidant that protects cells from oxidative stress, supporting tissue repair and immune function. - Bromelain and Papain:
Enzymes with anti-inflammatory properties that may reduce swelling and promote healing in tonsillar tissue.
Lifestyle & Dietary Practices for Tonsil Health
A comprehensive approach to lifestyle and dietary habits can significantly support tonsil health and overall oral immune function.
Oral Hygiene
- Regular Brushing and Flossing:
Maintain excellent oral hygiene by brushing at least twice a day and flossing daily to reduce bacterial load. - Tongue and Mouth Rinsing:
Use an antiseptic mouthwash to lower the risk of infections that could affect the tonsils.
Nutrition and Hydration
- Balanced Diet:
Eat a nutrient-rich diet with plenty of fruits, vegetables, lean proteins, and whole grains to support immune function. - Hydration:
Drinking ample water keeps the mucous membranes moist and aids in toxin removal. - Avoid Irritants:
Limit consumption of spicy, acidic, or overly hot foods that can irritate the tonsils.
Environmental and Behavioral Factors
- Avoid Tobacco and Alcohol:
These substances can irritate the throat and compromise immune defenses. - Stress Management:
Employ stress-reduction techniques like meditation, yoga, and deep breathing to improve overall immune function. - Regular Check-ups:
Routine visits to healthcare providers ensure early detection and management of tonsillar issues. - Humidifiers:
Using a humidifier, especially during dry seasons, helps maintain moisture in the airways, reducing throat irritation. - Allergen Avoidance:
Identify and avoid allergens that trigger chronic tonsil inflammation.
Trusted Resources for Tonsil Health
For further insights and detailed research on tonsil health, consider these reputable resources:
Books
- “The Complete Guide to Understanding Tonsils and Adenoids” by Michael J. Parker
A comprehensive resource discussing tonsil and adenoid anatomy, function, and treatment options. - “Head and Neck Surgery and Oncology” by Jatin P. Shah and Snehal G. Patel
An in-depth reference for healthcare professionals covering surgical management of tonsillar disorders. - “Oral Pathology: Clinical Pathologic Correlations” by Joseph A. Regezi, James J. Sciubba, and Richard C. K. Jordan
Offers detailed coverage of oral pathology, including various tonsil conditions with clinical case studies.
Academic Journals
- The Laryngoscope:
A leading journal in otolaryngology publishing research on tonsil disorders, surgical techniques, and treatment outcomes. - Journal of Clinical Otolaryngology and Allied Sciences:
Provides evidence-based research, reviews, and clinical guidelines on the diagnosis and treatment of tonsil-related conditions.
Mobile Apps
- MyENT:
An app for managing ear, nose, and throat conditions, offering information on tonsil health and treatment options. - ENT Surgery Handbook:
A resource for healthcare professionals detailing surgical procedures, including tonsillectomy techniques and postoperative care. - Oral-B:
Promotes good oral hygiene through guided routines and educational tips that help maintain tonsil and overall oral health.
Frequently Asked Questions
What is the primary function of the tonsils?
The tonsils serve as a first line of immune defense by trapping and filtering pathogens from the respiratory and digestive tracts, helping to initiate immune responses and develop immunological memory.
How do the tonsils contribute to immune surveillance?
Tonsils capture antigens via their crypts and present them to immune cells within lymphoid follicles. This process activates B and T lymphocytes, leading to antibody production and the formation of immune memory.
What causes recurrent tonsillitis?
Recurrent tonsillitis is often caused by chronic infections, frequently due to bacteria such as Group A Streptococcus, and may be exacerbated by poor oral hygiene or underlying immune dysfunction.
When is tonsillectomy recommended?
Tonsillectomy is typically recommended for patients with recurrent, chronic tonsillitis, obstructive sleep apnea due to hypertrophic tonsils, or in cases of suspected tonsillar malignancy.
Can lifestyle changes improve tonsil health?
Yes, maintaining good oral hygiene, staying hydrated, following a balanced diet, managing stress, and avoiding irritants like tobacco and excessive alcohol can significantly improve tonsil health and reduce infection risk.
Disclaimer & Sharing
The information provided in this article is for educational purposes only and should not be considered a substitute for professional medical advice. Always consult with a qualified healthcare provider for personalized diagnosis and treatment.
If you found this guide helpful, please share it on Facebook, X (formerly Twitter), or your preferred social platform to help spread awareness and promote tonsil health.