The trachea is a vital component of the human respiratory system, serving as the essential conduit for air between the upper respiratory passages and the lungs. This robust yet flexible tube not only plays a key role in breathing but also in protecting the lower airways from foreign particles and pathogens. In this guide, we delve into the intricate details of tracheal structure, its physiological functions, common disorders, state‐of‐the‐art diagnostic methods, available treatments, and everyday tips for maintaining tracheal health.
Table of Contents
- Tracheal Structural Insights
- Tracheal Function and Physiological Role
- Tracheal Conditions and Disorders
- Diagnostic Approaches for Tracheal Health
- Management and Treatment Options
- Supplemental Aids for Tracheal Wellness
- Tracheal Health: Best Practices
- Recommended References and Resources
- Frequently Asked Questions
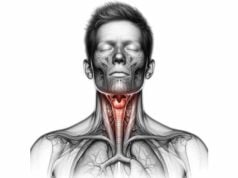
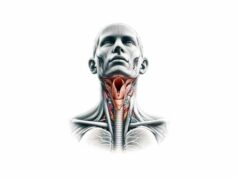
Tracheal Structural Insights
The trachea, commonly known as the windpipe, is an anatomical marvel engineered for both resilience and flexibility. Stretching from the lower larynx near the C6 vertebra to its bifurcation at the T4–T5 vertebrae, the trachea splits into the right and left bronchi—a critical junction known as the carina. This division marks the beginning of the complex network of airways leading to each lung lobe.
Layered Composition and Architecture
The trachea’s wall is composed of several distinct layers, each designed for a specific function:
- Mucosal Lining:
The innermost surface is lined with pseudostratified ciliated columnar epithelium. This cellular layer contains abundant goblet cells that secrete mucus to trap dust, bacteria, and other airborne particles. The coordinated beating of cilia propels the mucus upward toward the larynx, facilitating its eventual expulsion or swallowing. - Submucosal Layer:
Beneath the mucosa lies a supportive layer of connective tissue rich in seromucous glands. These glands contribute to the production of mucus, ensuring that the airway remains well-lubricated and effective in its protective role. - Cartilaginous Framework:
The structural integrity of the trachea is maintained by 16–20 C-shaped rings of hyaline cartilage. These rings prevent the collapse of the airway during respiration while allowing the flexibility needed for swallowing and vocalization. Their open ends, which face the esophagus, allow for a slight expansion that accommodates the passage of food. - Adventitial Covering:
The outermost layer, or adventitia, is a dense connective tissue that secures the trachea in place. This layer contains small blood vessels, nerves, and lymphatic channels, all of which are critical for the organ’s nourishment and immune surveillance.
Anatomical Relationships and Surrounding Structures
Positioned anteriorly in the neck and upper chest, the trachea is flanked by essential vascular and glandular structures. The carotid arteries and internal jugular veins are found on either side, while the thyroid gland lies just anterior to its upper segment. The intimate proximity of the recurrent laryngeal nerves—branches of the vagus nerve—plays a key role in voice modulation and airway reflexes.
Bifurcation and Beyond
At its lower end, the trachea divides into the right and left main bronchi at the carina. Notably, the right bronchus is typically shorter, wider, and more vertical, rendering it more susceptible to aspirated objects. Each bronchus further subdivides into lobar and segmental branches, ultimately leading to the alveolar sacs where gas exchange occurs.
Vascular, Neural, and Lymphatic Support
- Blood Supply:
The trachea receives oxygenated blood through branches of the inferior thyroid arteries and bronchial arteries originating from the thoracic aorta. - Nervous Innervation:
Autonomic fibers from the vagus nerve supply parasympathetic signals that regulate mucus secretion and smooth muscle tone, while sympathetic fibers help dilate the airway when needed. - Lymphatic Drainage:
Lymph nodes located along the trachea (pretracheal, paratracheal, and deep cervical nodes) filter lymph, playing a crucial role in immune defense.
Histological Considerations
Microscopically, the trachea’s lining is a dynamic structure comprised of ciliated cells, goblet cells, and basal cells. Ciliated cells propel mucus, goblet cells secrete it, and basal cells serve as progenitors for repairing and regenerating the epithelial layer—a testament to the trachea’s ability to maintain its protective barrier.
Variations, Anomalies, and Clinical Implications
While the general structure is consistent, anatomical variations can occur. For instance, some individuals may possess an accessory bronchus (tracheal bronchus), while congenital malformations such as tracheoesophageal fistula require early intervention. A comprehensive understanding of tracheal anatomy is vital in clinical settings—especially during procedures like intubation, bronchoscopy, and tracheostomy—to ensure patient safety and optimal outcomes.
Tracheal Function and Physiological Role
The trachea’s role transcends its basic function as an air conduit; it is intricately involved in maintaining optimal respiratory function and protecting the lungs. Its design ensures that inhaled air is conditioned, filtered, and delivered efficiently to the respiratory tree.
Air Conduction Mechanism
Every breath taken is routed through the trachea, which serves as the main highway for air movement. During inhalation, air enters via the nasal or oral cavities, passes through the larynx, and is channeled by the trachea into the bronchi before reaching the lungs. During exhalation, the process is reversed as air carrying carbon dioxide is expelled from the lungs through the trachea. This efficient system ensures that air exchange is continuous and vital for sustaining life.
Filtration and Defense Strategies
The trachea employs several defense mechanisms to protect the lower airways:
- Mucociliary Clearance:
The mucus secreted by goblet cells traps harmful particles and microbes. The beating of cilia on epithelial cells transports this mucus upward, where it can be swallowed or expelled—a natural cleaning process that reduces the risk of infection. - Cough Reflex:
In response to irritants or accumulated mucus, the trachea triggers a cough reflex. This rapid expulsion of air helps to clear the airway of potential obstructions and irritants, safeguarding the lungs from contaminants.
Air Conditioning: Humidification and Temperature Regulation
As air passes through the trachea, its moisture content and temperature are adjusted to closely match body conditions. This humidification and warming (or cooling) process is crucial for preventing the desiccation of the delicate alveolar tissues and optimizing gas exchange within the lungs.
Structural Support and Airway Patency
The hyaline cartilage rings provide essential rigidity, ensuring that the trachea remains open even during vigorous respiratory cycles. Meanwhile, the flexibility of the posterior membranous wall accommodates the movements required for swallowing and speaking. This harmonious balance of support and flexibility is indispensable for sustaining an unobstructed airway under varying physiological conditions.
Indirect Contributions to Vocalization
Although the trachea is not directly responsible for sound production, it supplies a consistent airflow to the larynx, where the vocal cords generate sound. This subglottic pressure is essential for phonation, illustrating how the trachea indirectly contributes to one’s ability to speak and communicate effectively.
Integrative Role in Respiratory Health
The trachea’s multifunctional design—from filtering pathogens to maintaining airway patency—ensures that every breath is both safe and efficient. Its interplay with other components of the respiratory system underscores the importance of holistic care, where the health of the trachea directly impacts overall respiratory wellness.
Tracheal Conditions and Disorders
A diverse range of disorders can compromise tracheal function, affecting individuals of all ages. Understanding these conditions is critical for early diagnosis, timely intervention, and effective management.
Inflammatory Conditions: Tracheitis
Tracheitis, an inflammation of the tracheal lining, often arises from bacterial or viral infections.
- Acute Tracheitis: Typically seen in children following viral infections, acute tracheitis can lead to a high fever, cough, and breathing difficulties.
- Chronic Tracheitis: Repeated exposure to irritants—such as cigarette smoke or environmental pollutants—can result in persistent inflammation, leading to a chronic cough and mucus production.
Treatment usually involves the use of antibiotics for bacterial infections, antivirals for viral causes, and supportive measures like humidification and hydration.
Narrowing of the Airway: Tracheal Stenosis
Tracheal stenosis refers to the abnormal narrowing of the airway, which can be either congenital or acquired.
- Congenital Stenosis: Present at birth, this condition may be linked to other developmental anomalies.
- Acquired Stenosis: Prolonged intubation, trauma, or infections can lead to scar tissue formation, reducing the airway diameter.
Symptoms include stridor, shortness of breath, and recurrent respiratory infections. Diagnostic imaging and bronchoscopy are pivotal for confirming the diagnosis, while treatment may involve endoscopic dilation, stenting, or surgical resection.
Structural Weakness: Tracheomalacia
Tracheomalacia is characterized by the softening and collapse of the tracheal walls, which compromises airway stability.
- Congenital Tracheomalacia: Occurs due to immature cartilage, often resolving as the child grows.
- Acquired Tracheomalacia: Results from prolonged mechanical ventilation or inflammatory conditions.
Patients often present with noisy breathing, recurrent infections, and episodes of airway obstruction. Treatment strategies range from conservative management using CPAP to surgical stabilization in severe cases.
Abnormal Connections: Tracheoesophageal Fistula
A tracheoesophageal fistula (TEF) is an aberrant connection between the trachea and esophagus, most commonly identified as a congenital anomaly.
- Clinical Presentation: Infants with TEF often exhibit feeding difficulties, choking, and recurrent respiratory infections due to the misdirection of food and fluids.
- Management: Definitive treatment involves surgical repair to restore the separation between the respiratory and digestive tracts, thereby preventing aspiration and further complications.
Tumorous Growths: Tracheal Neoplasms
Although rare, neoplasms of the trachea can be benign or malignant.
- Benign Tumors: Examples include papillomas and hamartomas, which may cause localized airway obstruction.
- Malignant Tumors: More commonly, squamous cell carcinoma and adenoid cystic carcinoma are diagnosed, presenting with progressive dyspnea, chronic cough, and hemoptysis.
Accurate diagnosis relies on imaging, bronchoscopy, and histological examination, with treatment options ranging from surgical resection to radiation and chemotherapy.
Rare Conditions: Tracheobronchopathia Osteochondroplastica
Tracheobronchopathia osteochondroplastica (TBO) is a benign condition marked by the formation of bony and cartilaginous nodules within the tracheal submucosa.
- Symptoms: Many patients remain asymptomatic, with the condition discovered incidentally during imaging or endoscopy.
- Management: Symptomatic cases are managed conservatively, focusing on relieving airway obstruction and monitoring for complications.
Airway Blockage: Foreign Body Aspiration
Foreign body aspiration is an emergency situation, particularly prevalent in children.
- Presentation: Sudden coughing, choking, and respiratory distress signal that an object may have entered the trachea.
- Diagnosis and Treatment: Radiographic imaging and bronchoscopy are essential for confirming the presence and location of the foreign object. Immediate removal is critical to restore airway patency and prevent secondary complications like pneumonia.
Positional Changes: Tracheal Deviation
Tracheal deviation occurs when the trachea is displaced from its midline position, often indicating underlying thoracic pathology such as a pneumothorax, large pleural effusion, or mediastinal mass.
- Clinical Clues: Abnormal breath sounds, chest asymmetry, and respiratory distress may accompany this displacement.
- Diagnostic Workup: Imaging modalities, including chest X-rays and CT scans, aid in pinpointing the cause, with treatment focusing on correcting the underlying condition.
Diagnostic Approaches for Tracheal Health
Timely and accurate diagnosis of tracheal disorders is crucial for effective management. A multi-faceted diagnostic approach is typically employed, integrating clinical evaluation with advanced imaging and functional tests.
Comprehensive Clinical Evaluation
The diagnostic journey begins with a thorough clinical examination.
- Patient History: Detailed inquiry into symptoms such as persistent cough, stridor, and dyspnea provides critical clues.
- Physical Assessment: Observation for signs like tracheal deviation, abnormal breath sounds, and palpable tenderness helps narrow down the differential diagnosis.
Radiographic Imaging
Imaging studies provide a non-invasive method to visualize the trachea and adjacent structures:
- Chest X-rays: Widely available and rapid, chest X-rays can reveal gross abnormalities such as tracheal deviation, masses, or the presence of foreign bodies. Although limited in detail, they serve as a valuable first-line tool.
- Computed Tomography (CT): CT scans offer high-resolution, cross-sectional images that delineate the trachea’s anatomy and pathology with precision. Multiplanar reconstruction further enhances diagnostic accuracy in conditions like tracheal stenosis.
- Magnetic Resonance Imaging (MRI): With the advantage of avoiding ionizing radiation, MRI is particularly useful in evaluating soft tissue involvement and vascular relationships, though its higher cost and longer acquisition time may limit routine use.
Endoscopic Examinations
Direct visualization of the tracheal lumen is accomplished through endoscopic techniques:
- Bronchoscopy: Considered the gold standard, bronchoscopy allows for real-time inspection, biopsy, and therapeutic interventions. It can identify inflammation, neoplasms, and dynamic airway collapse with high accuracy.
- Laryngoscopy: While primarily used to inspect the larynx, laryngoscopy can also assess the upper trachea for signs of extension of pathological processes.
Functional Respiratory Testing
Functional assessments provide insights into the physiological impact of tracheal disorders:
- Pulmonary Function Tests (PFTs): These tests, including spirometry, quantify airflow and lung capacity, helping detect obstructive patterns suggestive of tracheal compromise.
- Flow-Volume Loops: Graphical representations of airflow during inhalation and exhalation can indicate fixed or variable airway obstructions, with characteristic patterns seen in stenosis or dynamic collapse.
Tissue Sampling and Histology
When structural abnormalities are observed, tissue sampling becomes essential:
- Endobronchial Biopsy: Small tissue samples obtained during bronchoscopy allow for microscopic examination, crucial for diagnosing neoplasms or specific inflammatory conditions.
- Transbronchial Needle Aspiration (TBNA): This minimally invasive procedure targets lymph nodes or masses adjacent to the airway, aiding in the staging of malignancies and confirming diagnoses.
Laboratory and Advanced Techniques
Additional tests complement imaging and endoscopy:
- Microbiological Cultures and Cytology: Sputum and tissue samples may be cultured to identify infectious agents or analyzed cytologically to detect malignant cells.
- Advanced Imaging:
- Positron Emission Tomography (PET) Scans: Combined with CT, PET scans assess metabolic activity, particularly in malignant lesions, helping to determine the extent of disease.
- Ultrasound: Although less common for direct tracheal imaging, ultrasound is useful for guiding needle biopsies and evaluating superficial neck masses.
Together, these diagnostic methods provide a comprehensive view of tracheal health, guiding clinicians toward tailored treatment strategies.
Management and Treatment Options
Treating tracheal disorders demands a personalized approach that considers the nature and severity of the condition, as well as the patient’s overall health. Both conservative and surgical interventions play pivotal roles in restoring and maintaining airway integrity.
Medical Management
For many tracheal conditions, non-surgical therapies are the first line of treatment:
- Antibiotics and Antivirals: Infections such as acute tracheitis are managed with broad-spectrum antibiotics (e.g., amoxicillin-clavulanate) or antivirals where appropriate. Prompt treatment minimizes complications and supports recovery.
- Anti-inflammatory Agents: Corticosteroids—administered orally, intravenously, or via inhalation—reduce inflammation in conditions like chronic tracheitis, alleviating symptoms and improving airway patency.
- Bronchodilators: Medications such as albuterol are employed to relieve airway constriction, particularly in conditions like tracheomalacia, by relaxing smooth muscle and facilitating easier breathing.
Surgical and Interventional Procedures
When medical management is insufficient, surgical interventions may be necessary:
- Tracheal Resection and Reconstruction: In cases of severe tracheal stenosis or neoplasms, surgical resection of the affected segment followed by end-to-end anastomosis can restore airway continuity.
- Tracheostomy: Creating a direct airway through a neck incision is a life-saving measure in severe airway obstruction, prolonged intubation, or when other treatments fail.
- Bronchoscopic Interventions: Techniques such as endoscopic dilation, stent placement, and laser therapy allow minimally invasive management of obstructions and lesions. Laser ablation is particularly effective in debulking tumorous or granulation tissue.
- Innovative Therapies:
- 3D-Printed Tracheal Implants: Customized implants designed using advanced imaging data offer promising solutions for reconstructing complex tracheal defects.
- Stem Cell and Bioengineered Approaches: Ongoing research in regenerative medicine aims to replace damaged tracheal tissue with bioengineered constructs, potentially transforming treatment paradigms.
- Cryotherapy: The controlled application of extreme cold can ablate abnormal tissues, offering a minimally invasive alternative for managing both benign and malignant lesions.
Adjunct and Palliative Care
Supporting therapies complement primary treatments:
- Physiotherapy: Respiratory physiotherapy, including chest percussion and breathing exercises, aids in clearing secretions and strengthening respiratory muscles.
- Speech Therapy: Patients recovering from tracheostomy or those with voice impairments benefit from speech therapy to restore communication capabilities.
- Palliative Measures: In advanced disease, symptom relief and quality-of-life improvements are prioritized through targeted palliative care interventions, such as pain management and psychological support.
Each treatment modality is selected based on detailed diagnostic findings and patient-specific factors, ensuring that management is both effective and tailored to individual needs.
Supplemental Aids for Tracheal Wellness
Optimal tracheal health is not solely achieved through clinical interventions—nutritional support and targeted supplements can also play a key role. The integration of dietary supplements with conventional therapy helps reduce inflammation, bolster immune function, and maintain the structural integrity of the airway.
Key Supplements and Their Benefits
- Vitamin C:
Renowned for its antioxidant properties, vitamin C helps mitigate oxidative stress in the tracheal lining. Its immune-boosting capabilities are essential for preventing infections and supporting overall respiratory health. - Vitamin D:
Vital for immune modulation, adequate levels of vitamin D reduce the incidence of respiratory infections and may help in maintaining mucosal integrity within the trachea. - Omega-3 Fatty Acids:
Found in fish oil and flaxseed, these essential fats possess potent anti-inflammatory properties that help alleviate chronic inflammation, improving the overall resilience of tracheal tissues. - N-Acetylcysteine (NAC):
Acting as a precursor to glutathione, NAC helps thin mucus secretions, making it easier to clear the airway and reducing the risk of mucus plugging in compromised tracheal segments. - Echinacea:
This herbal supplement is celebrated for its immune-enhancing properties. It may reduce the frequency of respiratory infections, thereby indirectly protecting the trachea from recurrent inflammation. - Zinc:
Zinc is crucial for maintaining immune competence and promoting tissue repair. Its role in wound healing is particularly beneficial following surgical interventions involving the trachea. - Curcumin:
As the active compound in turmeric, curcumin offers robust anti-inflammatory and antioxidant benefits. It may help control chronic inflammatory processes that threaten the integrity of tracheal tissues. - Quercetin:
This naturally occurring flavonoid exhibits both anti-inflammatory and antiviral properties, contributing to improved respiratory function and a reduced risk of infection. - Probiotics:
Maintaining a healthy gut microbiome is linked to overall immune function. Probiotics help modulate systemic inflammation and may offer indirect benefits to respiratory health by reinforcing the body’s natural defense mechanisms.
Integrating Supplements into a Wellness Plan
Incorporating these supplements should be tailored to individual health needs and done under professional guidance. A balanced diet, rich in fruits, vegetables, lean proteins, and whole grains, forms the foundation of respiratory health. Supplements are best viewed as an adjunct to, rather than a replacement for, sound nutritional practices and medical treatment.
Tracheal Health: Best Practices
Daily lifestyle choices can profoundly affect tracheal health. Implementing healthy habits not only enhances respiratory efficiency but also helps prevent conditions that might compromise airway integrity.
Lifestyle Modifications
- Avoid Smoking:
Smoking introduces a host of toxins that irritate the tracheal lining and can lead to chronic inflammation, increasing the risk of tracheal disorders. Quitting smoking is one of the most effective strategies to protect respiratory health. - Practice Good Hygiene:
Regular handwashing and minimizing contact with individuals suffering from respiratory infections reduce the risk of contracting pathogens that could inflame the trachea. - Maintain Adequate Hydration:
Drinking sufficient water helps keep mucus secretions fluid, facilitating their clearance from the airways and reducing the risk of blockages. - Use Humidifiers:
In dry environments, a humidifier can help maintain the moisture balance of the tracheal mucosa, preventing irritation and dryness that may predispose the airway to infections. - Adopt a Balanced Diet:
A nutrient-rich diet supports immune function and tissue repair. Incorporating a variety of vitamins, minerals, and antioxidants can help protect the trachea from oxidative damage and inflammation. - Exercise Regularly:
Regular physical activity enhances lung capacity and strengthens the respiratory muscles. Improved cardiovascular fitness also supports efficient oxygen exchange and overall respiratory health. - Stay Updated with Vaccinations:
Vaccines against influenza, pertussis, and other respiratory pathogens are crucial for preventing infections that could compromise tracheal integrity. - Minimize Exposure to Pollutants:
Reducing contact with air pollutants, chemicals, and environmental toxins is essential. When exposure is unavoidable, using masks and air purifiers can provide an added layer of protection. - Manage Allergies Proactively:
Allergies can trigger chronic inflammation. Appropriate management—through medication or immunotherapy—helps minimize the inflammatory burden on the trachea. - Regular Medical Check-Ups:
Routine examinations allow for early detection and intervention of potential tracheal issues, ensuring that minor problems do not evolve into serious complications.
These best practices, when consistently applied, contribute significantly to maintaining a healthy trachea and overall respiratory wellness.
Recommended References and Resources
For those seeking additional information on tracheal health, a variety of trusted resources are available—from authoritative books to peer-reviewed journals and specialized mobile applications.
Books
- “The Respiratory System at a Glance” by Jeremy P.T. Ward and Jane Ward:
This concise resource provides a clear overview of respiratory anatomy and common disorders, making it ideal for both students and healthcare professionals. - “Principles of Pulmonary Medicine” by Steven E. Weinberger, Barbara A. Cockrill, and Jess Mandel:
A comprehensive text that covers the full spectrum of pulmonary medicine, including detailed discussions on tracheal conditions and their management. - “Clinical Respiratory Medicine” by Richard K. Albert, Stephen G. Spiro, and James R. Jett:
Offering in-depth insights into respiratory diseases, this book is a valuable reference for understanding both the diagnostic and therapeutic aspects of tracheal disorders.
Academic Journals
- American Journal of Respiratory and Critical Care Medicine:
A leading publication that features cutting-edge research on respiratory diseases, including studies on tracheal pathology and innovative treatment strategies. - Chest:
The official journal of the American College of Chest Physicians, it provides expert reviews, clinical guidelines, and the latest research findings relevant to tracheal and pulmonary health.
Mobile Applications
- Medscape:
An extensive resource offering up-to-date clinical information, guidelines, and drug references, ideal for both medical professionals and students. - MDCalc:
This app provides clinical calculators and decision support tools that are especially useful in assessing respiratory function and guiding treatment choices. - UpToDate:
A trusted clinical decision support system that delivers evidence-based articles and treatment guidelines on a wide range of medical conditions, including those affecting the trachea.
Frequently Asked Questions
What are common symptoms of tracheal disorders?
Tracheal disorders often manifest with persistent coughing, shortness of breath, and wheezing. Patients may also experience stridor, chest discomfort, and recurrent respiratory infections. Early recognition of these symptoms is critical for prompt diagnosis and treatment, preventing further complications.
How is tracheal stenosis typically diagnosed?
Tracheal stenosis is usually diagnosed through a combination of imaging techniques such as CT scans and X-rays, coupled with direct visualization using bronchoscopy. Pulmonary function tests and flow-volume loops further support the diagnosis by highlighting characteristic airflow limitations.
Can lifestyle changes improve tracheal health?
Absolutely. Adopting a healthy lifestyle—including smoking cessation, regular exercise, and a balanced diet—can significantly improve tracheal health. Maintaining good hydration, using humidifiers, and avoiding environmental pollutants also contribute to a reduced risk of tracheal inflammation and related disorders.
What surgical options are available for severe tracheal conditions?
Surgical interventions for severe tracheal conditions include tracheal resection with reconstruction, tracheostomy, and minimally invasive procedures like bronchoscopic dilation and stenting. The choice of surgery depends on the condition’s severity, location, and overall patient health.
How do supplements support tracheal function?
Certain supplements, including vitamins C and D, omega-3 fatty acids, and N-acetylcysteine, offer antioxidant and anti-inflammatory benefits that support tracheal health. These nutrients help reduce oxidative stress and improve immune function, contributing to better airway protection and recovery.
Disclaimer
The information provided in this article is intended for educational purposes only and should not be construed as medical advice. Always consult a healthcare professional for medical concerns or before beginning any new treatment regimen.
Please share this article on Facebook, X (formerly Twitter), or your favorite social platform to help others learn more about maintaining optimal tracheal and respiratory health.