Proliferative vitreoretinopathy (PVR) is a serious complication that can develop after retinal detachment surgery, ocular trauma, or other retinal procedures. It involves the formation of membranes on both surfaces of the retina, which contract and cause the retina to detach again, resulting in vision loss. PVR is defined by the proliferation of retinal pigment epithelial (RPE) cells, glial cells, and fibroblasts, which combine to form fibrous scar tissue. This condition affects 5-10% of patients undergoing retinal detachment surgery, posing a significant clinical challenge in ophthalmology.
PVR development is a complex, multi-stage process that starts with cell migration and proliferation in the vitreous cavity. These cells adhere to the retinal surfaces, forming membranes that can contract and pull the retina out of position. The severity of PVR varies, but in its advanced stages, it can result in total retinal detachment, severe vision impairment, or blindness. PVR symptoms include floaters, flashes of light, and progressive vision loss, which require immediate medical attention.
A detailed eye examination with indirect ophthalmoscopy and imaging techniques such as optical coherence tomography (OCT) and ultrasound is usually required to diagnose PVR. Early detection and intervention are critical for successfully managing PVR and preventing permanent vision loss. Because of its complexity, PVR requires a combination of surgical and medical approaches.
Traditional Management and treatment of proliferative vitreoretinopathy
The management and treatment of proliferative vitreoretinopathy focuses on preventing disease progression and addressing any retinal detachment that has occurred. Traditional treatment methods include surgical intervention and adjunctive therapies that inhibit cellular proliferation and membrane formation.
Surgical Interventions
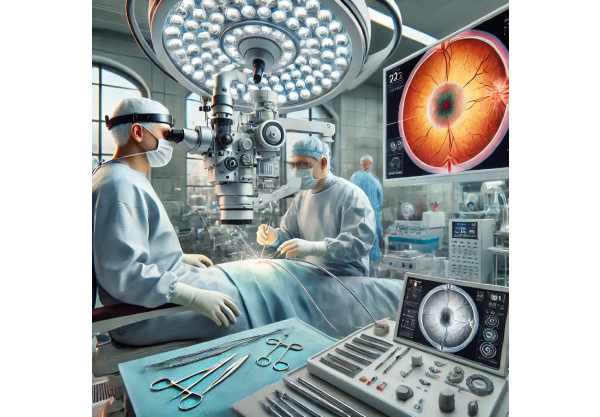
The primary treatment for PVR is surgery, which involves reattaching the retina and removing any fibrous membranes. The main surgical techniques are:
- Vitrectomy: This is the most commonly performed surgical procedure for PVR. It entails removing the vitreous gel from the eye and replacing it with a saline solution, oxygen, or silicone oil. The surgeon also removes the fibrous membranes on the retina to relieve traction before reattaching the retina.
- Membrane Peeling: During a vitrectomy, the surgeon carefully removes the epiretinal and subretinal membranes that have formed on the retina. This is a delicate procedure that requires precision to avoid damaging the retinal tissue.
- Retinectomy: If the membranes are extensive and tightly adhered to the retina, a retinectomy may be necessary. This entails removing a portion of the retina to relieve the traction and allow for reattachment.
- Scleral Buckling: This procedure involves wrapping a flexible band around the eye to counteract forces that pull the retina out of place. Scleral buckling can be used in conjunction with vitrectomy in certain cases.
Adjunctive therapies
Adjunctive therapies work to prevent PVR recurrence by inhibiting cellular proliferation and inflammation. These treatments can be used in conjunction with surgical interventions to improve outcomes.
- Intravitreal Injections: Corticosteroids, anti-VEGF agents, and anti-inflammatory drugs can be administered directly into the vitreous cavity to reduce inflammation and inhibit cellular proliferation.
- Anti-Proliferative Agents: Drugs like 5-fluorouracil (5-FU) and low-molecular-weight heparin (LMWH) have been used to inhibit cell proliferation, which leads to membrane formation.
- Radiation Therapy: Low-dose radiation has been investigated as a means of inhibiting cellular proliferation and lowering the risk of PVR recurrence, but its application is limited due to potential side effects.
Post-operative Care and Monitoring
Postoperative care is critical to ensuring treatment success and monitoring for signs of recurrence. This includes:
- Regular Follow-Up Visits: Patients should have frequent follow-up visits to monitor their retinal attachment, IOP, and overall eye health.
- Imaging Studies: OCT and ultrasound imaging are used to evaluate the retinal structure and look for early signs of membrane formation or retinal detachment.
- Medication Adherence: Patients may need to continue taking topical or systemic medications to reduce inflammation and prevent infection.
Innovative Approaches to Treating Proliferative Vitreoretinopathy
Recent advances in medical research and technology have resulted in significant improvements in the treatment of proliferative vitreoretinopathy. These cutting-edge approaches aim to increase surgical success rates, prevent recurrence, and improve overall patient outcomes.
Genetic Therapy
Gene therapy is a new field that shows promise for treating PVR by targeting the genetic factors that contribute to cellular proliferation and membrane formation. Researchers are looking into using gene editing techniques like CRISPR/Cas9 to change the expression of genes involved in PVR pathogenesis. Early research has shown that gene therapy can inhibit the proliferation of retinal pigment epithelial cells and reduce the formation of fibrous membranes.
Stem Cell Therapy
Stem cell therapy is a novel approach to treating PVR that promotes retinal repair and regeneration. Researchers are looking into the use of mesenchymal stem cells (MSCs) and induced pluripotent stem cells (iPSCs) to replace damaged retinal cells and restore normal function. Stem cells can also be engineered to produce anti-inflammatory and anti-proliferative factors, providing a two-fold benefit in the treatment of PVR. Clinical trials are currently underway to determine the safety and efficacy of stem cell-based therapies for retinal diseases, including PVR.
Advanced Drug Delivery Systems
Drug delivery system innovations improve the efficacy of PVR adjunctive therapies. These advanced systems aim to deliver medications to the retina in a sustained, targeted manner, reducing the need for frequent injections and increasing patient compliance. Notable advancements include:
- Sustained-Release Implants are biodegradable implants that release anti-inflammatory or anti-proliferative drugs over time. These implants can be inserted into the vitreous cavity during a vitrectomy to provide continuous drug delivery.
- Nanoparticle-Based Delivery: Drugs can be encapsulated in nanoparticles and delivered directly to the retina’s target cells. This approach improves drug efficacy while minimizing systemic side effects.
Immunomodulation
Immunomodulatory therapies seek to alter the immune response involved in the development of PVR. By targeting specific inflammatory pathways, these therapies can reduce the proliferation of fibroblasts and other cells involved in membrane formation. Recent studies have focused on identifying key cytokines and chemokines involved in PVR and developing targeted therapies to inhibit their activity. Clinical trials are being conducted to investigate the use of immunomodulatory agents, such as TNF-alpha and interleukin-6 (IL-6) inhibitors, in the treatment of PVR.
Personalized Medicine
Personalized medicine is revolutionizing PVR treatment by tailoring therapies to each patient’s genetic and molecular profile. Advances in genomics and biomarker research are allowing clinicians to identify patients at high risk for PVR and develop tailored treatment plans. To improve outcomes and reduce the risk of recurrence, personalized approaches may include genetic testing, biomarker analysis, and tailored drug regimens.
Artificial Intelligence, Machine Learning
Artificial intelligence (AI) and machine learning are revolutionizing the field of ophthalmology, including the management of PVR. AI algorithms can identify patterns and predict disease progression by analyzing large datasets containing imaging studies, clinical records, and genetic information. This capability enables personalized treatment plans and optimal patient care. Notable advancements include:
- AI-Based Diagnostic Tools: AI algorithms can examine OCT and ultrasound images to detect early signs of PVR and track disease progression. These tools provide ophthalmologists with valuable insights, allowing for more accurate diagnoses and timely interventions.
- Predictive Modeling: Machine learning models can predict the success of various treatment options based on individual patient characteristics, allowing treatment plans to be tailored for the best possible results.
Surgical Innovations
Surgical techniques and technologies are constantly evolving, increasing the safety and efficacy of PVR treatment. Innovations in this field include:
- Robotic-Assisted Surgery: Robotic systems improve accuracy and control during vitrectomy and membrane peeling procedures. These systems can lower the likelihood of complications and improve surgical outcomes.
- Microincisional Surgery: Advances in surgical instruments and techniques have allowed for the development of microincisional vitrectomy, which employs smaller incisions and less invasive procedures. This shortens recovery times and minimizes surgical trauma.
Clinical Trials and Research Networks
Ongoing clinical trials and collaborative research networks are critical for furthering PVR treatment. These initiatives bring together researchers, clinicians, and patients to speed up the development of new treatments and improve patient outcomes. The key research areas are:
- Combination Therapies: Researchers are looking into the synergistic effects of combining surgical, medical, and adjunctive therapies to improve treatment efficacy and lower recurrence rates.
- Innovative Therapeutics: Clinical trials are evaluating new therapeutic agents, such as small molecule inhibitors and biologics, to target specific pathways involved in PVR pathogenesis.






