Introduction to Ocular Surface Squamous Neoplasia
Ocular Surface Squamous Neoplasia (OSSN) refers to a group of malignant and pre-malignant lesions that develop from the squamous epithelium of the ocular surface, primarily affecting the conjunctiva and cornea. OSSN encompasses conditions ranging from mild dysplasia to invasive squamous cell carcinoma. These lesions are the most common ocular surface tumors, and they can manifest as a visible mass on the eye, often appearing as a white or pink growth. OSSN primarily affects older adults, with risk factors including prolonged UV exposure, HPV infection, immunosuppression (e.g., HIV/AIDS), and prior ocular surface disease or trauma.
The symptoms of OSSN can be subtle and nonspecific, making early detection difficult. If the lesion crosses the visual axis, patients may experience redness, irritation, a foreign body sensation, or visual changes. Clinical examination is frequently used to make a diagnosis, with imaging techniques such as high-resolution optical coherence tomography (HR-OCT) and ultrasound biomicroscopy assisting in determining the extent and invasiveness of the lesion. Histopathological examination after biopsy remains the gold standard for definitive diagnosis.
OSSN can progress from a pre-cancerous state to an invasive carcinoma, potentially causing significant ocular morbidity and even vision loss if not treated promptly. Management strategies seek to eliminate the tumor, preserve vision, and reduce recurrence.
OSSN is managed and treated using a combination of medical and surgical approaches, each tailored to the size, location, and severity of the lesion. The primary goals are to completely remove or destroy the tumor, prevent recurrence, and keep the ocular surface healthy and functioning properly.
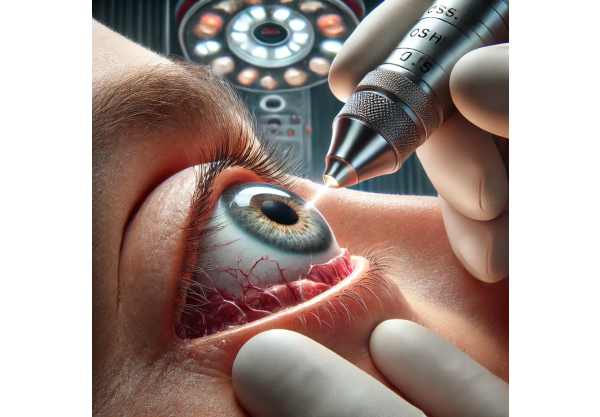
Surgical Excision
Surgical excision is a common treatment option for OSSN, particularly for well-defined, localized lesions. The procedure entails removing the lesion with a margin of healthy tissue to ensure complete excision and reduce the risk of reoccurrence. Adjunctive therapies, such as cryotherapy, are frequently used on the surgical margins to eliminate any remaining malignant cells. The excised tissue is then sent for histopathological examination to ensure complete removal and to guide future treatment, if necessary.
Topical Chemotherapy
Topical chemotherapy is becoming increasingly popular as a primary or adjunctive treatment for OSSN. Direct application of medications to the ocular surface includes mitomycin C (MMC), 5-fluorouracil (5-FU), and interferon alpha-2b (IFNα2). These agents are effective for treating diffuse, multifocal, or recurrent lesions and can be used when surgery is not an option. Topical chemotherapy is less invasive and can be administered in an outpatient setting, reducing the need for surgical intervention while maintaining ocular surface integrity.
** Mitomycin C (MMC)**: MMC is a powerful antineoplastic agent that inhibits DNA synthesis and effectively treats OSSN. It is usually administered as an eye drop in cycles, with a treatment plan tailored to the lesion’s response. MMC is especially useful for larger, more aggressive lesions and can be used alongside surgical excision to reduce recurrence rates.
5-fluorouracil (5-FU): 5-FU is another topical chemotherapeutic agent that inhibits DNA synthesis. It is not as popular as MMC, but it can be effective for smaller or less aggressive lesions. 5-FU is also administered in cycles, and the side effects are typically mild and manageable.
Interferon Alpha-2b (IFNα2b): This immunomodulatory agent effectively treats OSSN. It is available in two forms: topical drops and periocular injections. IFNα2b is especially beneficial for patients who are resistant to other chemotherapeutic agents or have large lesions. It works by increasing the immune response to tumor cells and has a good safety profile.
Radiation Therapy
Radiation therapy, such as brachytherapy and external beam radiation, is an option for treating OSSN, especially if the disease is recurrent or extensive. Brachytherapy entails placing radioactive plaques near the tumor, which delivers high doses of radiation directly to the affected area while sparing healthy tissue. External beam radiation therapy (EBRT) is less commonly used, but it can be effective for large or invasive lesions that do not respond to surgery or topical treatments. Radiation therapy can be extremely effective, but it requires specialized equipment and expertise.
Immunotherapy
Recent advances in immunotherapy have created new opportunities for treating OSSN. Immune checkpoint inhibitors, such as pembrolizumab and nivolumab, which have revolutionized cancer treatment, are being tested for efficacy in OSSN. These drugs work by blocking immune response-inhibiting proteins, allowing the body’s immune system to more effectively target and destroy cancer cells. Clinical trials are currently underway to determine the best use of these agents in OSSN, and preliminary results are promising.
Photodynamic therapy (PDT)
Photodynamic therapy (PDT) is a new treatment option for OSSN that uses photosensitizing agents and light exposure to kill tumor cells. The photosensitizer, usually a porphyrin derivative, is applied to the ocular surface and selectively absorbed by tumor cells. When exposed to a specific wavelength of light, the photosensitizer activates, releasing reactive oxygen species that cause cell death. PDT provides a non-invasive treatment option with the potential for high specificity while causing minimal damage to surrounding tissues. It is especially beneficial to patients with recurring or multifocal lesions.
Laser Therapy
Laser therapy, such as CO2 laser ablation and argon laser photocoagulation, is an option for treating OSSN. These methods require the precise application of laser energy to vaporize or coagulate tumor tissue. Laser therapy is an outpatient treatment that is effective for small, well-defined lesions. It has the advantage of being minimally invasive and recovering quickly, but it may require additional treatments to ensure complete tumor eradication.
Advanced Diagnostic and Monitoring Techniques
Advances in diagnostic imaging and molecular diagnostics improve the ability to detect, characterize, and monitor OSSN. High-resolution optical coherence tomography (HR-OCT) and confocal microscopy produce detailed images of the ocular surface, allowing precise measurement of lesion depth and extent. These technologies aid in early diagnosis and treatment decisions. Furthermore, molecular diagnostic techniques like polymerase chain reaction (PCR) and next-generation sequencing (NGS) are being used to identify specific genetic and molecular markers linked to OSSN. These markers can provide information about tumor behavior and response to treatment, allowing for more personalized treatment approaches.
Targeted Therapy
Targeted therapy, which uses drugs to target specific molecular pathways involved in tumor growth and progression, is an active area of research in OSSN. Agents that block specific growth factor receptors, signaling pathways, or other molecular targets are being tested for efficacy in treating OSSN. Targeted therapy may provide more effective and less toxic treatment options for patients with advanced or refractory disease.
Integrative and complementary therapies
Integrative and complementary therapies are being investigated to aid in the treatment of OSSN. Nutritional support, herbal medicine, and mind-body practices such as acupuncture and meditation may improve overall well-being, reduce treatment-related side effects, and improve patients’ quality of life while undergoing conventional treatments. While these therapies are not a replacement for medical treatment, they can be useful supplements in a comprehensive care plan.






