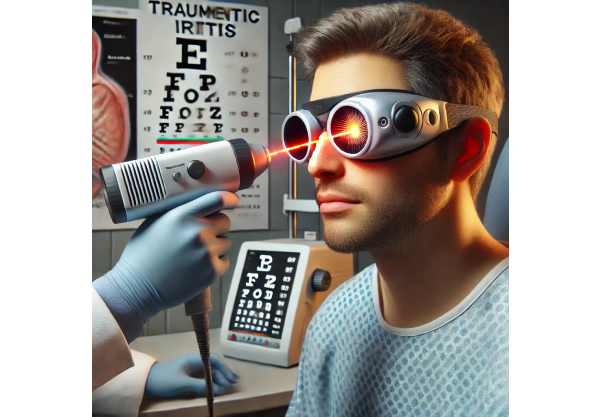
Traumatic iritis is an inflammatory condition of the iris, or colored part of the eye, caused by blunt or penetrating trauma. Traumatic iritis, as opposed to infectious or autoimmune iritis, is caused directly by physical injury. If not treated promptly, this condition can cause severe discomfort and visual disturbances. Symptoms of traumatic iritis include eye pain, redness, light sensitivity (photophobia), blurred vision, and, in some cases, headache. When exposed to bright light or when moving the eyes, the pain may worsen.
The pathophysiology of traumatic iritis involves iris tissue disruption, which causes inflammation and an immune response. This response may result in the release of inflammatory mediators, causing additional irritation and swelling. In severe cases, traumatic iritis can cause complications such as increased intraocular pressure, cataracts, or glaucoma, all of which can impair vision. A comprehensive eye examination, which includes a slit-lamp examination to detect inflammation and damage in the anterior segment of the eye, is frequently used to diagnose the condition.
Early and accurate diagnosis is critical for successful management of traumatic iritis. To alleviate symptoms, reduce inflammation, and avoid long-term complications, the condition necessitates a personalized treatment plan. Understanding the underlying causes and mechanisms of traumatic iritis is critical for developing effective treatment plans and enhancing patient outcomes.
Best Practices for Traumatic Iritis Management
Traumatic iritis management and treatment focuses on pain relief, inflammation reduction, and complication prevention. Standard treatment methods usually include a combination of medications and supportive care measures.
Medical Management
Medical management is the cornerstone of traumatic iritis treatment, with the goal of reducing inflammation and providing symptom relief. The key components of medical management are:
- Corticosteroids: Topical corticosteroid eye drops, such as prednisolone or dexamethasone, are frequently used to reduce inflammation. These medications help to reduce the immune response and alleviate symptoms. More severe inflammation may necessitate periocular or systemic corticosteroids.
- Cycloplegic Agents: Atropine or cyclopentolate are used to dilate the pupil and keep the iris from adhering to the lens or cornea (posterior synechia). Cycloplegic agents also help to relieve pain by paralyzing the ciliary muscles, which control pupil movement.
Nonsteroidal Anti-inflammatory Drugs (NSAIDs) Topical NSAIDs, such as ketorolac, can be used alongside corticosteroids to reduce inflammation and pain. These medications reduce the production of prostaglandins, which are involved in the inflammatory process.
Supportive Care
Supportive care is essential for managing symptoms and promoting recovery. This includes:
- Cold Compresses: Putting cold compresses on the affected eye can help relieve pain and swelling.
- Sunglasses: Wearing sunglasses can help relieve photophobia and protect the eyes from bright light, which can aggravate symptoms.
- Rest and Hydration: Getting enough rest and hydration can help the body heal faster and feel better overall.
Monitoring and Follow-up
Regular monitoring and follow-up visits are critical for assessing treatment response and detecting complications early. During follow-up visits, the ophthalmologist will assess the level of inflammation, look for synechiae, and monitor intraocular pressure to prevent secondary glaucoma.
Innovative Approaches to Treating Traumatic Iritis
Advancements in the treatment of traumatic iritis have resulted in novel approaches that improve the effectiveness and safety of managing this condition. These cutting-edge innovations cover a wide range of topics, including drug delivery systems, novel pharmacological agents, and advanced diagnostic tools.
Sustained-release drug delivery systems.
One of the most significant advances in traumatic iritis treatment has been the development of sustained-release drug delivery systems. These systems ensure consistent and prolonged medication release, reducing the need for frequent dosing and improving patient compliance.
Dexamethasone Intravitreal Implants (Ozurdex) These biodegradable implants are inserted into the eye and gradually release dexamethasone over several months. This approach maintains a consistent concentration of corticosteroids, effectively controlling inflammation and reducing the need for eye drops.
- Cyclosporine Implants: Cyclosporine is an immunosuppressive agent that can be used to reduce inflammation in severe cases of traumatic iritis. Sustained-release cyclosporine implants provide continuous drug delivery, which improves therapeutic outcomes while reducing side effects from systemic administration.
Novel Pharmaceutical Agents
Pharmacological innovations have resulted in the development of new agents that target specific pathways involved in the inflammatory process of traumatic iritis.
- Biological Agents: Biologics, such as tumor necrosis factor (TNF) inhibitors, are being studied for their ability to modulate the immune response in traumatic iritis. These agents can specifically target inflammatory cytokines, making them a more effective way to reduce inflammation.
- JAK Inhibitors: JAK inhibitors, such as tofacitinib, have shown promise in the treatment of autoimmune and inflammatory disorders. Their effectiveness in managing traumatic iritis is being studied, particularly in cases where standard treatments have failed.
Advanced Diagnostic Tools
Accurate and timely diagnosis is critical for successful treatment of traumatic iritis. Diagnostic technology has advanced, making it easier to detect and monitor this condition.
- Optical Coherence Tomography (OCT): OCT is a non-invasive imaging technique that generates high-resolution cross-sectional images of the eye’s anterior and posterior segments. It allows for detailed visualization of inflammation, edema, and structural changes, which aids in the diagnosis and management of traumatic iritis.
- Anterior Segment Ultrasound Biomicroscopy (UBM): UBM is an imaging modality that uses high-frequency ultrasound to see the anterior segment of the eye in great detail. It can detect subtle changes in the iris and ciliary body, providing important information for diagnosing and treating traumatic iritis.
Gene Therapy & Regenerative Medicine
Emerging fields such as gene therapy and regenerative medicine may provide new treatments for traumatic iritis by targeting the underlying mechanisms of inflammation and tissue damage.
- Gene Therapy: Gene-editing technologies such as CRISPR-Cas9 are being studied for their ability to alter genes involved in the inflammatory response. Gene therapy, which selectively targets and edits these genes, could provide a new approach to treating traumatic iritis.
- Stem Cell Therapy: Researchers are investigating stem cell-based treatments for repairing and regenerating damaged ocular tissues. Stem cells have the ability to differentiate into different cell types, which promotes healing and reduces inflammation. Researchers are working to develop safe and effective stem cell therapies for traumatic iritis.
Artificial Intelligence, Machine Learning
Artificial intelligence (AI) and machine learning are improving the diagnosis and treatment of traumatic iritis by allowing for more accurate and efficient clinical data analysis.
- AI-Driven Diagnostics: Artificial intelligence algorithms can analyze large amounts of clinical and imaging data to identify patterns and detect early signs of traumatic iritis. These tools can help clinicians make accurate diagnoses and create personalized treatment plans.
- Predictive Analytics: Machine learning models can forecast the likelihood of complications and treatment outcomes based on patient-specific information. This data can help guide clinical decisions and improve patient care.
Telemedicine & Remote Monitoring
The integration of telemedicine and remote monitoring technologies improves access to care and management of traumatic iritis.
- Remote Consultations: Telemedicine platforms allow for remote consultations with ophthalmologists, providing timely access to expert care, particularly for patients in underserved areas. This approach allows for early diagnosis and ongoing management without the need for frequent in-person visits.
- Wearable Devices: Wearable devices with sensors can track ocular parameters like intraocular pressure and inflammation in real time. These devices can send data to healthcare providers, enabling continuous monitoring and timely interventions.
Personalized Medicine
Personalized medicine is increasingly important in the treatment of traumatic iritis. Advances in genetic testing and biomarker identification enable personalized treatment plans based on an individual’s genetic and biochemical profile.
- Customized Treatment Plans: By understanding a patient’s genetic predispositions and injury responses, clinicians can create more effective and personalized treatment plans. Personalized medicine has the potential to improve therapy effectiveness by optimizing drug selection, dosing, and duration.
Biocompatible ocular implants aim to provide structural support and deliver medications directly to the source of inflammation.
- Anti-inflammatory Ocular Inserts: These inserts are placed in the conjunctiva sac and release anti-inflammatory agents over time. They provide a simple and effective way to control inflammation in traumatic iritis.
- Biodegradable Ocular Scaffolds: Biodegradable scaffolds can be implanted to promote tissue regeneration and drug delivery. These scaffolds degrade over time, releasing drugs in a controlled manner while promoting healing.






