What is hyperlysinemia?
Hyperlysinemia is a rare metabolic disorder characterized by high levels of the amino acid lysine in the blood due to a lack of the enzyme saccharopine dehydrogenase. This enzyme is essential in the lysine degradation pathway, and its absence causes an accumulation of lysine and its metabolic intermediates. Lens dislocation, or displacement of the eye’s lens from its normal position, is one of the ocular manifestations of hyperlysinemia. This condition can impair vision and lead to other complications if not treated properly.
Insights into Hyperlysinemia
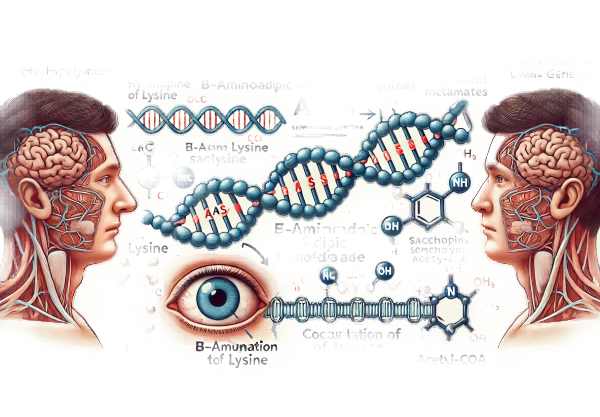
Hyperlysinemia is a hereditary condition inherited in an autosomal recessive pattern, which means that a person must inherit two copies of the defective gene, one from each parent, in order to develop the disorder. The gene responsible for hyperlysinemia is AASS, which encodes the enzyme α-aminoadipic semialdehyde synthase. This enzyme serves two functions: it catalyzes the first steps in the degradation of lysine, resulting in the production of saccharopine and, eventually, acetyl-CoA, a critical molecule in energy production.
The pathophysiology of hyperlysinemia is characterized by the disruption of this degradation pathway, which results in the accumulation of lysine and intermediate metabolites. Elevated lysine levels can disrupt normal cellular functions and have been linked to a variety of metabolic and physiological abnormalities, including those that affect the eye.
Ocular manifestations
Lens dislocation, also known as ectopia lentis, is a significant ocular manifestation of hyperlysinemia. The lens is a transparent, biconvex structure in the eye that directs light to the retina. Hyperlysinemia impairs the structural integrity of ocular tissues, resulting in lens instability. The exact mechanism by which high lysine levels cause lens dislocation is unknown, but it is thought to involve changes in the extracellular matrix and zonular fibers that hold the lens in place.
Systematic Manifestations
Beyond its ocular effects, hyperlysinemia can cause a variety of systemic symptoms. These can include developmental delays, intellectual disabilities, hypotonia (low muscle tone), and seizures. The severity of these symptoms varies greatly among affected individuals. Some people may only have mild symptoms, while others may face more serious developmental and neurological issues.
Genetic and Biochemical Aspects
There are two types of hyperlysinemia based on the enzyme deficiency involved:
- Type I Hyperlysinemia: Caused by a lack of the enzyme saccharopine dehydrogenase (SDH), which results in an accumulation of saccharopine and lysine.
- Type II Hyperlysinemia: Caused by a lack of the enzyme lysine-ketoglutarate reductase (LKR), which results in elevated lysine levels without a significant increase in saccharopine.
Both types produce high levels of lysine in the blood and urine, but their biochemical profiles vary, which is critical for diagnostic purposes.
Epidemiology
Hyperlysinemia is a very rare condition, with only a few documented cases worldwide. Its prevalence is unknown due to the small number of diagnosed individuals. However, it is thought to be more common in certain populations with higher rates of consanguineous marriages, where the chances of inheriting two copies of the defective gene are higher.
Clinical Presentation
Hyperlysinemia has a wide range of clinical manifestations. Some people may be asymptomatic or have only minor symptoms, whereas others may have significant developmental delays, intellectual disability, and neurological disorders. Lens dislocation and other ocular manifestations can cause visual disturbances such as blurred vision, double vision, and, in severe cases, vision loss.
Complications
Hyperlysinemia complications, particularly those associated with lens dislocation, may include:
- Glaucoma: Lens displacement can cause increased intraocular pressure, which can lead to glaucoma, a serious condition that can result in permanent vision loss if not treated promptly.
- Cataracts: Opacification of the lens can occur, resulting in cataract formation and additional visual impairment.
- Retinal Detachment: In some cases, lens instability can result in retinal detachment, which is a medical emergency that requires immediate attention to prevent permanent vision loss.
Differential Diagnosis
Differentiating hyperlysinemia from other metabolic and genetic disorders that can present with similar symptoms, including:
- Marfan Syndrome: A connective tissue disorder that can cause lens dislocation and other systemic symptoms such as cardiovascular abnormalities.
- Homocystinuria is a metabolic disorder characterized by high homocysteine levels, which can cause lens dislocation, developmental delays, and thromboembolic events.
- Sulfite Oxidase Deficiency is a rare metabolic disorder characterized by neurological and ocular symptoms, including lens dislocation.
Genetic Counseling
Hyperlysinemia has an autosomal recessive inheritance pattern, so affected families should seek genetic counseling. This can help parents understand the risk of recurrence in future pregnancies and consider options like prenatal testing and preimplantation genetic diagnosis.
Recognizing Hyperlysinemia
Hyperlysinemia is diagnosed through a combination of clinical evaluation, biochemical testing, and genetic analysis. Common diagnostic methods include the following:
Biochemical Testing
Biochemical testing is the first step in diagnosing hyperlysinemia. Lysine and its metabolites levels are determined through analysis of blood and urine samples. Key tests include:
- Plasma Amino Acid Analysis: This test determines the concentration of amino acids in the bloodstream. Hyperlysinemia is characterized by elevated levels of lysine.
- Urinary Amino Acid Analysis: This test identifies amino acids in the urine. High levels of lysine and its metabolites, such as saccharopine, help to confirm hyperlysinemia.
- Enzyme Assays: Saccharopine dehydrogenase or lysine-ketoglutarate reductase deficiency can be confirmed using specific enzyme activity assays on cultured fibroblasts or leukocytes.
Genetic Testing
Genetic testing is required to confirm the diagnosis and determine the specific mutation in the AASS gene. The techniques used include:
- DNA Sequencing: This method involves sequencing the AASS gene to identify mutations. Next-generation sequencing (NGS) panels for metabolic disorders may include the AASS gene, allowing for more in-depth analysis.
- Targeted Mutation Analysis: If a specific mutation is known to exist in the patient’s family, targeted analysis can be used to detect its presence in the patient.
- Whole Exome Sequencing (WES): When the diagnosis is uncertain, WES can identify mutations in the AASS gene and other genes linked to similar metabolic disorders.
Clinical Evaluation
A thorough clinical evaluation is essential for diagnosing hyperlysinemia, especially when assessing ocular manifestations such as lens dislocation. This includes:
- Ophthalmologic Examination: An ophthalmologist examines the eye to determine the position and condition of the lens, as well as to look for any other ocular abnormalities.
- Neurological Assessment: A neurological exam to determine developmental delays, intellectual disability, and other neurological symptoms.
- Developmental Assessment: An evaluation of the patient’s developmental milestones and cognitive function to detect any delays or abnormalities.
Imaging Studies
Imaging studies can be used to evaluate the structural integrity of the eye and detect complications caused by lens dislocation. This includes:
- Slit-Lamp Examination: This imaging technique provides detailed visualization of the anterior segment of the eye, including the lens, in order to detect dislocation or subluxation.
- Ultrasound Biomicroscopy (UBM): UBM produces high-resolution images of the eye’s internal structures, which can aid in determining the position of the lens and any associated abnormalities.
Differential Diagnosis
Given the symptoms’ overlap with other metabolic and genetic disorders, differential diagnosis is critical. Specific biochemical and genetic tests may be used to rule out conditions such as Marfan syndrome, homocystinuria, and sulfite oxidase deficiency.
Hyperlysinemia Treatment Options
Treatment for hyperlysinemia focuses on symptom management, particularly ocular manifestations such as lens dislocation, as well as addressing the underlying metabolic disorder. Here are the standard treatment options together with emerging therapies:
- Dietary Management: One of the primary treatments for hyperlysinemia is dietary changes that reduce lysine intake. A diet low in lysine and high in other essential amino acids can help alleviate symptoms and reduce lysine accumulation in the body. Patients frequently consult with a dietitian to develop a balanced, lysine-restricted diet plan.
- Medications: There are no specific medications that can directly lower lysine levels; however, supportive treatments such as anticonvulsants may be prescribed to manage seizures, and other symptomatic treatments can be used as needed.
- Ocular Surgery: For lens dislocation, surgical intervention may be required. This may include:
- Lens Extraction: Removing the dislocated lens to relieve symptoms and avoid complications such as glaucoma or retinal detachment.
- Intraocular Lens Implantation: Following lens extraction, an artificial lens can be implanted to restore vision.
- Scleral Fixation: In some cases, the natural lens can be repositioned and secured with scleral sutures.
- Regular Monitoring: A multidisciplinary team consisting of metabolic specialists, ophthalmologists, and neurologists must monitor the patient continuously. Regular follow-ups allow doctors to monitor the patient’s progress and make adjustments to treatments as needed.
Emerging Therapies
- Gene Therapy: Research is currently underway to develop gene therapy approaches to correct the underlying genetic defect in hyperlysinemia. Gene therapy seeks to introduce a functional copy of the defective AASS gene into the patient’s cells, potentially leading to a permanent cure.
- Enzyme Replacement Therapy (ERT): ERT entails giving synthetic or recombinant enzymes to make up for the deficient enzyme in hyperlysinemia. This approach is still in the experimental stage, but it shows promise for treating metabolic disorders.
- Advanced Dietary Supplements: Researchers are looking into specific amino acid supplements and other metabolic regulators to find more effective dietary interventions for managing lysine levels without compromising overall nutrition.
Best Practices for Avoiding Hyperlysinemia (Related Lens Dislocation)
- Genetic Counseling: If there is a family history of hyperlysinemia, consult a genetic counselor before beginning a pregnancy. This can aid in the risk assessment and discussion of options such as prenatal testing or preimplantation genetic diagnosis.
- Prenatal Testing: For families with a history of hyperlysinemia, prenatal testing such as amniocentesis or chorionic villus sampling (CVS) can detect the disorder early in pregnancy, allowing for timely intervention.
- Newborn Screening: Have newborns undergo metabolic screening tests to detect hyperlysinemia early. Early detection can lead to timely dietary and medical interventions, preventing severe symptoms.
- Avoid Consanguineous Marriages: In populations where consanguineous marriages are common, it is best to avoid them in order to lower the risk of autosomal recessive disorders such as hyperlysinemia.
- Regular Ophthalmologic Exams: Individuals with hyperlysinemia require regular eye exams to monitor for lens dislocation and other ocular complications. Early detection enables timely intervention.
- Maintain a Balanced Diet: Those diagnosed with hyperlysinemia should strictly follow a lysine-restricted diet as prescribed by a healthcare professional. This helps to regulate lysine levels and avoid systemic and ocular complications.
- Educate Family Members: Raising awareness among family members about hyperlysinemia and its genetic implications can aid in early detection and prevention measures.
Trusted Resources
Books
- “Inherited Metabolic Diseases: A Clinical Approach” by Georg F. Hoffmann and Johannes Zschocke
- “Ophthalmic Genetics: Clinical and Molecular Approaches” by Elias I. Traboulsi
- “The Eye in Pediatric Systemic Disease” by Alex V. Levin and Robert W. Enzenauer






