Primary Acquired Nasolacrimal Duct Obstruction (PANDO) is a common condition that causes a blockage in the nasolacrimal duct, preventing tears from draining normally from the eye into the nasal cavity. This obstruction causes tear overflow (epiphora) and recurring eye infections. PANDO primarily affects adults, with a higher prevalence in women, particularly those over 40 years old.
Anatomy and Physiology of the Nasolacrimal System
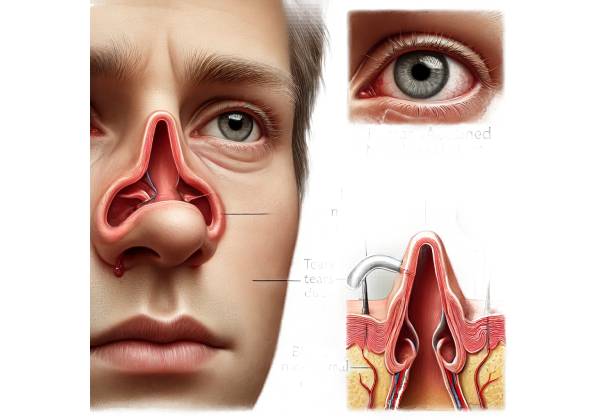
Understanding PANDO requires knowledge of the anatomy and function of the nasolacrimal system. The nasolacrimal system consists of structures involved in tear production and drainage, which ensure that tears adequately lubricate the eye surface and are properly drained to prevent overflow.
- Lacrimal Glands: These glands, located in the upper outer region of each orbit, make the aqueous component of tears.
- Puncta: Small openings in the inner corners of the upper and lower eyelids that allow tears to enter the drainage system.
- Canaliculi are narrow channels that transport tears from the puncta to the lacrimal sac.
- Lacrimal Sac: A reservoir for tears from the canaliculi.
- Nasolacrimal Duct: A duct that connects the lacrimal sac and the nasal cavity, allowing tears to drain into the nose.
Tears normally flow from the lacrimal glands across the eye surface, into the puncta, through the canaliculi into the lacrimal sac, and then into the nasal cavity via the nasolacrimal duct.
Pathophysiology of PANDO
PANDO occurs when the nasolacrimal duct becomes clogged, preventing tears from draining correctly. PANDO’s exact mechanisms are unknown, but several factors contribute to its development:
- Age-Related Changes: As people age, the nasolacrimal duct tissues can develop fibrosis and stenosis, resulting in obstruction.
- Inflammation: Chronic inflammation in the nasolacrimal duct can cause scarring and narrowing.
- Hormonal Factors: Hormonal changes, particularly in postmenopausal women, are thought to contribute to the increased incidence of PANDO in females.
- Anatomical Variations: Differences in the anatomy of the nasolacrimal duct and surrounding structures can predispose people to obstruction.
- Infections: Recurrent or chronic infections of the lacrimal drainage system can cause inflammation and eventual obstruction.
Symptoms of PANDO:
PANDO primarily manifests as symptoms of impaired tear drainage:
- Epiphora: The most common symptom is excessive tearing or overflow of tears. Patients frequently report tears running down their cheeks, especially in cold or windy weather.
- Recurrent Infections: Blockage of the nasolacrimal duct can cause dacryocystitis, which is a lacrimal sac infection. Dacryocystitis causes pain, redness, and swelling in the inner corner of the eye, as well as discharge.
- Mucus Discharge: Chronic obstruction can cause mucus accumulation and a sticky discharge from the eye.
- Blurry Vision: Frequent tearing and discharge can impair vision clarity.
- Swelling and Tenderness: Patients may feel swelling and tenderness in the area surrounding the lacrimal sac.
Epidemiology
PANDO is a common condition, particularly in older adults. It is more common in women, with studies showing a female-to-male ratio of about 3:1. The incidence rises with age, especially after the age of forty. Hormonal changes, anatomical differences, and other factors all contribute to a higher prevalence in women.
Complications
If left untreated, PANDO can cause a number of complications, primarily due to chronic tear retention and the risk of infection:
- Dacryocystitis is an infection of the lacrimal sac that can be acute or chronic. Acute dacryocystitis is characterized by pain, redness, swelling, and pus discharge, whereas chronic dacryocystitis can cause persistent discharge and mild discomfort.
- Conjunctivitis: Secondary bacterial conjunctivitis can develop as a result of stagnant tears, which provide a breeding ground for bacteria.
- Mucocele: Chronic obstruction can cause a mucocele, which is a cystic lesion filled with mucus in the lacrimal sac.
- Orbital Cellulitis is a severe infection that can spread to the tissues surrounding the eye, causing redness, swelling, pain, and potentially vision-threatening complications.
Differential Diagnosis
PANDO symptoms may overlap with those of other conditions that affect the lacrimal drainage system. It is critical to distinguish PANDO from other causes of epiphora and tear drainage problems.
- Secondary Nasolacrimal Duct Obstruction: Caused by external factors such as trauma, tumors, or inflammatory diseases of the nasolacrimal duct.
- Canalicular Obstruction: Blockage of the canaliculi rather than the nasolacrimal duct, most commonly caused by trauma, infections, or chronic inflammation.
- Punctal Stenosis: The narrowing or blockage of the puncta that prevents tears from entering the drainage system.
- Lacrimal Gland Disorders: Conditions affecting the lacrimal glands can alter tear production and cause symptoms similar to PANDO.
Effects on Quality of Life
PANDO has a significant impact on a patient’s quality of life, especially if left untreated. Chronic tearing and recurring infections can cause discomfort, embarrassment, and social issues. Patients may also feel anxious and frustrated as a result of the condition’s persistence. A timely diagnosis and appropriate management are critical for relieving symptoms and improving the patient’s overall well-being.
Diagnostic methods
Primary Acquired Nasolacrimal Duct Obstruction (PANDO) requires a thorough clinical evaluation, specialized tests, and imaging studies to confirm the presence and location of the obstruction. Here are the detailed diagnostic methods for PANDO:
Clinical Evaluation
- Patient History: A complete patient history is required to determine the onset, duration, and severity of symptoms. The clinician will inquire about episodes of excessive tearing, recurring eye infections, discharge, and any history of trauma or prior eye surgery.
- Physical Examination: A thorough examination of the eye and its surrounding structures is performed. The clinician looks for swelling, redness, discharge, and tenderness around the lacrimal sac. The puncta and canaliculi are also examined to rule out any other possible causes of tear drainage problems.
Tear Drainage Tests
- Fluorescein Dye Disappearance Test: This test involves injecting a small amount of fluorescein dye into the conjunctival sac. The dye should normally drain via the nasolacrimal system. The clinician checks the eye after a few minutes to see if the dye has vanished, indicating proper tear drainage. Retained dye indicates a blockage.
- Jones Dye Test (Primary and Secondary): This two-part test helps determine the location of the obstruction.
- Primary Jones Test: Fluorescein dye is injected into the eye, and a cotton swab is placed in the nasal cavity to check for dye presence after a few minutes. The absence of dye indicates a blockage.
- Secondary Jones Test: If the primary test is negative, the clinician will irrigate the lacrimal system with saline. The presence of fluorescein in the nasal cavity following irrigation indicates a partial obstruction or functional drainage issue.
Lacrimal Irrigation
Lacrimal irrigation is the process of flushing saline through the nasolacrimal system to ensure patency. A small cannula is inserted through the punctum and saline is gently injected. Resistance or reflux of saline indicates a blockage. This procedure is also useful in determining the level of obstruction.
Imaging Studies
- Dacryocystography: This radiographic technique involves injecting a contrast dye into the lacrimal sac and obtaining X-ray images to visualize the anatomy of the nasolacrimal duct. It aids in the determination of the location and extent of the obstruction.
- Dacryoscintigraphy is a nuclear medicine scan that uses a radioactive tracer to measure tear drainage. The tracer is injected into the eye, and a gamma camera monitors its progression through the nasol lacrimal system. This imaging technique provides functional information about the tear drainage process and aids in the detection of any blockages or slow drainage areas.
Nasal Endoscopy
Nasal endoscopy is a minimally invasive procedure that involves the use of a thin, flexible endoscope to examine the nasal cavity and the nasolacrimal duct opening. This enables the clinician to identify any anatomical abnormalities, such as polyps, deviations, or obstructions, that may be contributing to PANDO.
Additional Diagnostic Tests
In some cases, additional tests may be required to rule out other conditions or gather more detailed information about the obstruction.
- Punctal Plug Test: Temporary punctal plugs are placed into the puncta to see if occlusion alleviates symptoms. If tearing significantly decreases, it indicates that the primary problem may be with the puncta or canaliculi rather than the nasolacrimal duct.
- Computed Tomography (CT) Scan: If structural abnormalities or tumors affecting the nasolacrimal duct are suspected, a CT scan may be ordered. It shows detailed cross-sectional views of the nasal and lacrimal anatomy.
- Magnetic Resonance Imaging (MRI): MRI can be used to assess soft tissue structures and detect masses or inflammatory processes that may be causing obstruction.
Primary Acquired Nasolacrimal Duct Obstruction Management
Managing Primary Acquired Nasolacrimal Duct Obstruction (PANDO) focuses on symptom relief, infection prevention, and restoring normal tear drainage. The severity of the condition, the patient’s preferences, and the presence of any complications all influence treatment decisions. Here are the primary ways to manage PANDO:
Medical Management
- Antibiotic Therapy: Patients with acute dacryocystitis are prescribed antibiotics to treat the infection. Depending on the severity of the infection, topical antibiotic eye drops or systemic antibiotics may be required. Amoxicillin-clavulanate, ciprofloxacin, and doxycycline are among the most commonly prescribed antibiotics.
- Anti-inflammatory Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) or corticosteroid eye drops can be used to reduce inflammation in the nasolacrimal duct and surrounding tissues, resulting in symptom relief.
- Warm Compresses and Massage: Applying warm compresses to the affected area several times per day can help relieve symptoms by increasing drainage and decreasing swelling. A gentle massage over the lacrimal sac can also help remove minor obstructions and improve tear flow.
Surgical Management
When conservative treatments are ineffective, surgical intervention may be required to restore tear drainage and relieve symptoms.
- Dacryocystorhinostomy (DCR): This is the gold standard surgical procedure for treating PANDO. It opens a new path for tears to drain directly into the nasal cavity, bypassing the clogged nasolacrimal duct. There are two primary approaches to DCR:
- External DCR: An incision is made on the side of the nose to gain access to the lacrimal sac and establish a new drainage pathway. This method has a high success rate and enables direct visualization of the surgical site.
- Endoscopic DCR: This minimally invasive technique avoids external incisions by performing the procedure through the nasal cavity with an endoscope. It has the advantage of a shorter recovery time and less visible scarring, but it may have a slightly lower success rate than external DCR.
- Balloon Dacryoplasty: This minimally invasive procedure involves inserting a catheter containing a small balloon into the nasolacrimal duct. The balloon is inflate to dilate the duct and relieve the obstruction. Balloon dacryoplasty may be useful for partial obstructions or patients who are not candidates for DCR.
- Intubation: Silicone tubes or stents can be inserted into the nasolacrimal duct to keep it open and allow tear drainage. Intubation is frequently combined with other procedures, such as DCR or balloon dacryoplasty, to improve their efficacy.
- Punctal Procedures: Patients suffering from punctal stenosis or canalicular obstruction may benefit from procedures such as punctal dilation, punctoplasty, or canaliculotomy to restore tear drainage. These procedures enlarge or reconstruct the puncta or canaliculi in order to improve tear flow.
Post-operative Care
Effective postoperative care is critical for ensuring the success of surgical treatments and avoiding complications.
- Medications: Antibiotic and anti-inflammatory eye drops are prescribed following surgery to prevent infection and inflammation. It is critical to adhere to the ophthalmologist’s medication regimen.
- Follow-Up Visits: Regular follow-up visits are scheduled to monitor the healing process, check the patency of the new drainage pathway, and detect any complications. During these visits, the surgeon may perform irrigation or endoscopic procedures to ensure proper tear drainage.
- Activity Restrictions: Patients should avoid strenuous activities, heavy lifting, and nasal blowing during the initial healing period. These precautions help to avoid disruption of the surgical site and lower the risk of complications.
Lifestyle and Supportive Measures
In addition to medical and surgical treatments, a number of lifestyle and supportive measures can help manage PANDO.
- Eye Hygiene: Proper eye hygiene, such as regular cleaning of the eyelids and lashes, can help prevent infections and reduce irritation.
- Protective Eyewear: Wearing protective eyewear while engaging in activities that expose the eyes to dust, wind, or irritants can lower the risk of exacerbating symptoms.
- Hydration and Diet: Staying hydrated and eating a well-balanced diet high in vitamins and minerals can benefit overall eye health and healing.
Trusted Resources and Support
Books
- “Diseases of the Lacrimal System” by Mohammad Javed Ali
- This comprehensive book provides detailed information on the anatomy, physiology, and pathology of the lacrimal system, including PANDO. It covers diagnostic methods, treatment options, and surgical techniques in depth.
- “Clinical Ophthalmology: A Systematic Approach” by Jack J. Kanski
- A widely used textbook that offers a thorough overview of various ocular conditions, including nasolacrimal duct obstructions. It includes sections on diagnosis, management, and surgical procedures, making it a valuable resource for both students and practitioners.
Organizations
- American Academy of Ophthalmology (AAO)
- Website: www.aao.org
- The AAO provides extensive resources on eye conditions, including PANDO. Their website offers patient education materials, research updates, and professional guidelines to help patients and healthcare providers stay informed about the latest developments in ophthalmology.
- American Society of Ophthalmic Plastic and Reconstructive Surgery (ASOPRS)
- Website: www.asoprs.org
- ASOPRS is a professional organization dedicated to the field of ophthalmic plastic and reconstructive surgery. Their website provides information on various lacrimal disorders, including PANDO, and offers resources for finding qualified surgeons and seeking appropriate treatment.










