The vas deferens is a vital component of the male reproductive system, responsible for transporting sperm from the epididymis to the ejaculatory ducts. This slender, muscular tube not only plays a critical role in fertility but also is central to procedures such as vasectomy and its reversal. Its intricate structure, layered histology, and precise neural and vascular regulation ensure that sperm remain viable until ejaculation. In this guide, we explore the detailed anatomy of the vas deferens, delve into its primary functions, examine common disorders, and discuss the diagnostic methods and treatment options available. We also provide evidence-based health tips and nutritional recommendations to support optimal vas deferens and reproductive health.
Table of Contents
- Anatomical Structure
- Primary Functions
- Common Conditions
- Diagnostic Techniques
- Treatment Options
- Supplemental & Nutritional Support
- Health and Lifestyle Tips
- Trusted Resources
- Frequently Asked Questions
Anatomical Structure
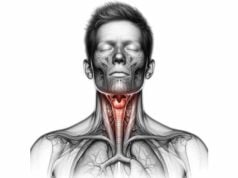
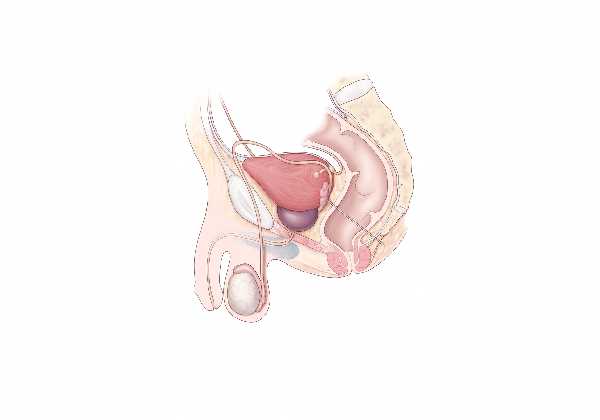
The vas deferens is a long, tubular structure that extends from the tail of the epididymis to the ejaculatory ducts. Measuring between 30 and 45 centimeters in length, it forms a crucial conduit for the transportation of sperm. Its pathway is both complex and carefully arranged: the vas deferens begins at the epididymis, ascends within the spermatic cord, passes through the inguinal canal, traverses the pelvic cavity, and finally joins with the duct of the seminal vesicle. This union creates the ejaculatory duct, which empties into the prostatic urethra.
Gross Structure and Regional Divisions
The vas deferens can be divided into five distinct segments:
- Epididymal Segment:
This proximal segment connects directly to the tail of the epididymis, where sperm mature and are stored. - Funicular Segment:
Located within the spermatic cord, this segment traverses the scrotum and plays an important role in sperm transport. - Inguinal Segment:
As the vas deferens ascends through the inguinal canal, it is accompanied by the testicular artery and veins, reflecting its critical vascular and neural associations. - Pelvic Segment:
Once within the pelvic cavity, the vas deferens crosses over the ureter. Its course here is vital for proper anatomical orientation and is significant during pelvic surgeries. - Ampullary Segment:
The terminal portion near the seminal vesicles is dilated, serving as a storage reservoir before sperm mix with seminal fluid to form semen.
Histological Composition
The wall of the vas deferens is composed of three main layers:
- Mucosal Layer:
- Lined with pseudostratified columnar epithelium that features stereocilia, the mucosal layer increases the surface area for absorption and secretion.
- The lamina propria, a supportive connective tissue beneath the epithelium, contains small blood vessels and nerves that nourish and maintain the mucosa.
- Muscularis:
- This thick middle layer is subdivided into three layers of smooth muscle: an inner longitudinal, a middle circular, and an outer longitudinal layer.
- These muscle layers coordinate to produce peristaltic contractions that propel sperm forward during ejaculation.
- Adventitia:
- The outermost layer is made of loose connective tissue, which anchors the vas deferens to adjacent structures and provides structural support.
Vascular, Lymphatic, and Neural Supply
A robust network ensures the vas deferens remains functional and resilient:
- Blood Supply:
- The primary arterial supply comes from branches of the superior vesical artery, ensuring that the vas deferens receives an adequate flow of oxygen and nutrients.
- Venous Drainage:
- Venous return occurs through the pampiniform plexus—a complex network of veins in the spermatic cord that eventually drains into the testicular vein.
- Lymphatic Drainage:
- Lymph from the vas deferens is channeled to the internal iliac lymph nodes, which play a role in immune surveillance and infection control.
- Nerve Supply:
- Innervation is predominantly sympathetic, provided via the hypogastric plexus. This autonomic input regulates the peristaltic contractions necessary for sperm transport.
Surrounding Structures and Anatomical Relationships
Understanding the vas deferens also requires consideration of its adjacent structures:
- Spermatic Cord:
- The vas deferens forms an integral part of the spermatic cord, which also contains the testicular artery, veins, lymphatics, and nerves.
- Inguinal Canal:
- The passage of the vas deferens through the inguinal canal is significant both anatomically and surgically, as it relates to conditions like inguinal hernias.
- Proximity to the Ureter:
- In the pelvic region, the vas deferens crosses over the ureter. Surgeons must be mindful of this relationship during procedures to avoid inadvertent injury.
- Seminal Vesicles:
- The terminal segment of the vas deferens connects with the duct of the seminal vesicle, forming the ejaculatory duct—a critical junction for the formation of semen.
Anatomical Variations and Clinical Implications
Variations in the vas deferens can affect fertility and surgical outcomes:
- Congenital Absence:
- Some men may be born with the congenital bilateral absence of the vas deferens (CBAVD), often associated with cystic fibrosis, leading to infertility despite normal sperm production.
- Anomalous Course:
- Rare variations in the course or structure of the vas deferens can complicate surgical interventions, such as vasectomy or its reversal.
A thorough understanding of the vas deferens’ anatomy is essential for diagnosing conditions, planning surgical interventions, and ensuring optimal male reproductive health.
Primary Functions
The vas deferens serves as a crucial conduit in the male reproductive system. Its primary functions are centered on the transport, storage, and delivery of sperm, all of which are integral to male fertility.
Sperm Transport and Storage
- Peristaltic Movements:
- The coordinated contractions of the smooth muscle layers generate peristaltic waves that move sperm from the epididymis through the vas deferens to the ejaculatory ducts.
- This process is tightly regulated by the sympathetic nervous system, ensuring that sperm travel efficiently during ejaculation.
- Temporary Sperm Storage:
- The ampullary segment of the vas deferens serves as a storage reservoir, allowing sperm to accumulate before ejaculation.
- This storage capability ensures that a sufficient number of sperm are available when ejaculation is triggered.
Role in Ejaculation
During ejaculation, the vas deferens plays a pivotal role in mixing sperm with seminal fluid to form semen:
- Sympathetic Stimulation:
- The release of norepinephrine from sympathetic nerves stimulates vigorous contractions of the vas deferens.
- These contractions propel sperm into the ejaculatory ducts where they mix with fluids from the seminal vesicles and prostate.
- Formation of Semen:
- The amalgamation of sperm with seminal and prostatic fluids creates semen, which provides the medium necessary for sperm viability and motility.
- Ejaculatory Duct Formation:
- The junction where the vas deferens meets the duct of the seminal vesicle forms the ejaculatory ducts, a critical passage that leads to the urethra for semen expulsion.
Sperm Viability and Nutrient Support
The vas deferens also contributes to maintaining the viability of sperm:
- Nutrient-Rich Environment:
- The fluid within the vas deferens contains nutrients and protective factors that help preserve sperm integrity during transit.
- Protection Against Stress:
- The structural and vascular characteristics of the vas deferens protect sperm from oxidative stress and mechanical damage, ensuring they remain healthy until ejaculation.
Hormonal Regulation
Hormones significantly influence the function of the vas deferens:
- Testosterone:
- Testosterone, produced by the testes, is crucial for the development and maintenance of the vas deferens. It promotes the growth of smooth muscle and supports sperm production.
- Oxytocin:
- Though more commonly associated with female reproduction, oxytocin plays a role in the male reproductive system by enhancing the contractility of the vas deferens during ejaculation.
- Other Regulatory Factors:
- A balanced hormonal environment ensures that the vas deferens can effectively support the transport and maturation of sperm, directly impacting fertility.
Impact on Male Fertility
The proper functioning of the vas deferens is essential for male fertility:
- Sperm Delivery:
- Without an unobstructed vas deferens, mature sperm cannot be effectively delivered to the urethra, leading to infertility.
- Obstructions and Anomalies:
- Conditions such as congenital absence, scarring, or blockage can result in azoospermia (absence of sperm in the ejaculate), highlighting the critical role the vas deferens plays in reproductive success.
Through its multifaceted roles—from ensuring efficient sperm transport and storage to contributing to ejaculation and maintaining sperm viability—the vas deferens is indispensable for male reproductive health.
Common Conditions
Various disorders can affect the vas deferens, impacting its structure and function. Early identification and proper management of these conditions are essential for maintaining male fertility and reproductive health.
Vasectomy
A vasectomy is a widely performed surgical procedure designed to achieve male sterilization by interrupting the continuity of the vas deferens.
- Procedure Overview:
- During a vasectomy, a small incision or puncture is made in the scrotum to expose the vas deferens. A segment of the duct is then cut, cauterized, or clipped, effectively preventing sperm from entering the ejaculatory ducts.
- Effectiveness and Reversibility:
- Vasectomy is highly effective, with success rates exceeding 99%. Although it is considered permanent, reversal procedures such as vasovasostomy or vasoepididymostomy are available, albeit with varying degrees of success.
- Potential Complications:
- Complications can include infection, hematoma, chronic pain (post-vasectomy pain syndrome), and the formation of sperm granulomas.
Congenital Absence of the Vas Deferens (CBAVD)
CBAVD is a congenital condition in which one or both vas deferens fail to develop, often associated with mutations in the CFTR gene and cystic fibrosis.
- Clinical Presentation:
- Men with CBAVD typically present with infertility despite normal sperm production in the testes.
- Diagnostic Approach:
- Diagnosis involves genetic testing for CFTR mutations and imaging studies to confirm the absence of the vas deferens.
- Management Options:
- Assisted reproductive technologies (ART), such as testicular sperm extraction (TESE) and intracytoplasmic sperm injection (ICSI), offer viable options for achieving pregnancy in affected individuals.
Vas Deferens Obstruction
Obstructions in the vas deferens can impede the passage of sperm, leading to infertility.
- Etiology:
- Obstructions may result from infections (e.g., epididymitis), surgical complications (such as post-vasectomy scarring), trauma, or congenital anomalies.
- Symptoms and Diagnosis:
- The primary symptom is infertility, often characterized by azoospermia. Diagnostic tools include semen analysis, scrotal ultrasound, and vasography.
- Treatment:
- Surgical reconstruction, including vasovasostomy or vasoepididymostomy, can sometimes restore the sperm transport pathway and improve fertility.
Epididymitis and Deferentitis
Inflammation of the epididymis (epididymitis) and the vas deferens (deferentitis) can impair sperm transport and cause discomfort.
- Causes:
- Common causes include bacterial infections (often sexually transmitted infections like chlamydia or gonorrhea), urinary tract infections, and sometimes viral infections.
- Symptoms:
- Symptoms include scrotal pain, swelling, redness, and sometimes systemic signs such as fever.
- Treatment:
- Management typically involves antibiotics, anti-inflammatory medications, and supportive care such as scrotal elevation and ice packs.
Vas Deferens Tumors
Tumors of the vas deferens are rare but can be either benign or malignant.
- Presentation:
- A palpable mass, discomfort, or pain in the scrotum may indicate the presence of a tumor. Obstruction and infertility can also result from tumor growth.
- Diagnosis and Management:
- Diagnosis is made via imaging studies (ultrasound, MRI) and confirmed with biopsy. Treatment options vary based on the tumor’s nature and extent and may include surgical excision, radiation therapy, or chemotherapy.
Varicocele
Although primarily a condition of the pampiniform plexus, varicocele can indirectly affect the vas deferens by altering the temperature and blood flow within the spermatic cord.
- Causes and Symptoms:
- Varicocele arises from malfunctioning venous valves, leading to dilated veins. It often causes a dull ache, swelling, and may contribute to reduced sperm quality.
- Diagnosis and Treatment:
- Diagnosis is typically made through physical examination and confirmed with scrotal ultrasound. Treatments include varicocelectomy or embolization, which can improve the overall environment for the vas deferens and enhance fertility.
Understanding these conditions is essential for the diagnosis, management, and preservation of male fertility. Early intervention and appropriate treatment can often restore normal function and improve reproductive outcomes.
Diagnostic Techniques
A comprehensive diagnostic evaluation is critical for identifying and managing disorders of the vas deferens. A range of techniques is employed, from clinical examinations and laboratory tests to advanced imaging and surgical exploration.
Clinical Examination
- Patient History:
- A detailed history covering fertility issues, pain, infections, previous surgeries (like vasectomy), and other relevant reproductive concerns is the first step in evaluation.
- Physical Examination:
- A careful examination of the scrotum, testicles, and spermatic cord can reveal abnormalities such as swelling, tenderness, varicoceles, or palpable masses.
Semen Analysis
Semen analysis is a cornerstone in assessing male fertility and the function of the vas deferens.
- Sperm Count:
- Evaluates the concentration of sperm in the ejaculate; low counts may indicate obstruction or dysfunction.
- Motility and Morphology:
- Assesses how well sperm move and their structural integrity. Obstructions in the vas deferens often result in poor motility and abnormal sperm shape.
Imaging Studies
- Scrotal Ultrasound:
- This non-invasive imaging technique uses sound waves to visualize the vas deferens, testicles, and surrounding structures, helping to detect blockages, varicoceles, or tumors.
- Transrectal Ultrasound (TRUS):
- Particularly useful for evaluating the prostate and seminal vesicles, TRUS can also help assess the distal portion of the vas deferens.
- MRI and CT Scans:
- These modalities provide high-resolution images of the pelvic region, assisting in the diagnosis of complex cases, such as tumors or congenital anomalies.
Vasography
- Procedure:
- Vasography involves injecting a contrast dye into the vas deferens, followed by X-ray imaging to map the duct’s course and identify any obstructions or structural abnormalities.
- Indications:
- This technique is particularly useful when other tests suggest an obstruction but are inconclusive.
Genetic Testing
- CFTR Mutation Analysis:
- Genetic screening for CFTR mutations is important in cases of congenital bilateral absence of the vas deferens (CBAVD), as these are commonly associated with cystic fibrosis.
- Y-Chromosome Microdeletion Testing:
- This test identifies deletions in the Y chromosome that may contribute to male infertility.
Biopsy and Histopathological Examination
- Tissue Sampling:
- In cases where tumors or chronic inflammatory changes are suspected, a biopsy of the vas deferens or adjacent tissue may be performed.
- Histopathology:
- Microscopic examination of the biopsy sample can confirm the presence of malignancy or chronic inflammatory conditions.
Hormonal Evaluation
- Hormone Level Testing:
- Measuring levels of testosterone, follicle-stimulating hormone (FSH), and luteinizing hormone (LH) can provide insight into the endocrine factors affecting sperm production and transport.
- Interpreting Results:
- Abnormal hormone levels can indicate underlying conditions that may impact the function of the vas deferens and overall fertility.
By combining these diagnostic techniques, clinicians can obtain a comprehensive picture of vas deferens health, enabling tailored treatment strategies and improved reproductive outcomes.
Treatment Options
Effective treatment of vas deferens disorders depends on accurate diagnosis and the severity of the condition. A variety of interventions—ranging from conservative medical management to advanced surgical techniques—are available to restore or preserve male fertility.
Medical Management
- Antibiotics and Anti-inflammatory Agents:
- For infections leading to epididymitis or deferentitis, appropriate antibiotics (such as doxycycline or ciprofloxacin) and NSAIDs are administered to reduce inflammation and relieve pain.
- Hormonal Therapy:
- In cases where hormonal imbalances affect sperm production or transport, hormone replacement therapies may be employed to normalize testosterone, FSH, and LH levels.
Minimally Invasive Procedures
- Percutaneous Embolization:
- Primarily used for treating varicocele, this procedure involves the insertion of a catheter to deliver coils or sclerosing agents to block the abnormal veins, thereby reducing pressure on the vas deferens.
- Vasectomy Reversal Procedures:
- Vasovasostomy:
- This surgical procedure reconnects the severed ends of the vas deferens after a vasectomy, aiming to restore the pathway for sperm transport.
- Vasoepididymostomy:
- When there is blockage at the level of the epididymis, this more complex surgery creates a direct connection between the vas deferens and the epididymis.
Surgical Interventions
- Varicocelectomy:
- Surgical ligation of varicocele veins improves blood flow and reduces the negative impact of varicocele on sperm quality. It is performed via open, laparoscopic, or microsurgical techniques.
- Vas Deferens Reconstruction:
- In cases of obstruction or congenital abnormalities, reconstructive surgery can restore the continuity of the vas deferens. Techniques such as end-to-end anastomosis or bypass grafting are used.
- Tumor Excision:
- For vas deferens tumors, surgical excision is necessary. The approach depends on whether the tumor is benign or malignant, with additional treatments such as radiation or chemotherapy for cancerous lesions.
Advanced and Innovative Treatments
- Microsurgical Techniques:
- The use of high-magnification microscopes during surgery (microsurgery) enhances precision, reducing the risk of complications during procedures like vasovasostomy or varicocelectomy.
- Stem Cell Therapy:
- Experimental treatments using stem cells aim to regenerate damaged vas deferens tissue. Although still in the early research stages, this approach shows promise for repairing congenital or acquired defects.
- Robotic-Assisted Surgery:
- Robotic systems, such as the da Vinci Surgical System, allow for highly precise, minimally invasive surgeries on the vas deferens, improving recovery times and surgical outcomes.
Assisted Reproductive Technology (ART)
- Intracytoplasmic Sperm Injection (ICSI):
- For cases of severe obstruction or congenital absence, sperm can be directly extracted from the testes (via TESE) and injected into an egg, bypassing the need for a fully functional vas deferens.
- Testicular Sperm Extraction (TESE):
- This procedure involves surgically extracting sperm directly from testicular tissue when they are absent from the ejaculate due to vas deferens issues.
By selecting the most appropriate treatment based on the specific condition and patient needs, clinicians can help restore fertility and alleviate symptoms associated with vas deferens disorders.
Supplemental & Nutritional Support
In addition to conventional medical and surgical treatments, certain nutritional supplements can support the health of the vas deferens and overall male reproductive system. These supplements work by improving sperm quality, reducing oxidative stress, and maintaining hormonal balance.
Recommended Supplements
- Zinc:
- Zinc is critical for sperm production and motility. It supports testosterone synthesis and helps protect sperm from oxidative damage.
- Vitamin C:
- As a powerful antioxidant, vitamin C protects sperm against free radicals and improves overall sperm count and quality.
- L-Carnitine:
- L-Carnitine enhances energy production within sperm cells, improving their motility and viability.
- Coenzyme Q10 (CoQ10):
- CoQ10 promotes cellular energy production and acts as an antioxidant, which is vital for maintaining the health and motility of sperm.
- Selenium:
- Selenium plays a key role in antioxidant defense, supporting sperm health and ensuring proper morphology.
- Folic Acid:
- Folic acid is essential for DNA synthesis and repair, which helps ensure that sperm develop normally.
- Omega-3 Fatty Acids:
- Found in fish oil, omega-3 fatty acids have anti-inflammatory properties that improve sperm quality and overall reproductive health.
- Vitamin E:
- Vitamin E works synergistically with vitamin C to provide antioxidant protection, promoting healthy sperm function.
- Ashwagandha:
- This adaptogenic herb helps reduce stress and supports hormonal balance, potentially improving sperm quality and overall reproductive health.
Integrating Supplements
It is advisable to consult a healthcare provider before beginning any supplement regimen. When integrated into a balanced diet rich in fruits, vegetables, lean proteins, and whole grains, these supplements can enhance vas deferens function, support sperm viability, and contribute to overall male fertility.
Health and Lifestyle Tips
Maintaining optimal health of the vas deferens and overall reproductive function involves a combination of proper lifestyle choices, dietary habits, and regular health monitoring. Here are some practical tips to promote reproductive health:
- Maintain a Balanced Diet:
- Incorporate nutrient-dense foods, including fruits, vegetables, lean proteins, and healthy fats, to support overall reproductive health.
- Exercise Regularly:
- Regular physical activity improves blood circulation, reduces stress, and supports hormonal balance.
- Avoid Smoking:
- Smoking negatively impacts sperm quality and overall reproductive health. Quitting smoking is one of the most effective ways to improve fertility.
- Limit Alcohol Intake:
- Excessive alcohol consumption can impair sperm production and motility. Moderation is key.
- Manage Stress:
- Engage in stress-reduction techniques such as meditation, yoga, or mindfulness, as chronic stress can adversely affect reproductive hormones.
- Stay Hydrated:
- Adequate hydration is essential for maintaining overall health and optimal sperm production.
- Wear Loose-Fitting Clothing:
- Opt for loose underwear and avoid tight-fitting pants to minimize heat buildup in the scrotum, which can negatively impact sperm quality.
- Avoid Environmental Toxins:
- Reduce exposure to pesticides, industrial chemicals, and other environmental toxins that may impair reproductive health.
- Regular Health Check-Ups:
- Routine medical examinations, including semen analyses and hormonal evaluations, help detect potential issues early on.
- Practice Safe Sex:
- Use protection to prevent sexually transmitted infections (STIs) that can damage the vas deferens and affect fertility.
By incorporating these healthy habits into your daily routine, you can support the proper function of the vas deferens and enhance overall reproductive health.
Trusted Resources
For further information on vas deferens health and male reproductive function, consider these authoritative resources:
Books
- “The Male Reproductive System” by Richard E. Jones and Kristin H. Lopez
- An in-depth resource covering the anatomy, physiology, and disorders of the male reproductive system, including the vas deferens.
- “Male Infertility: A Comprehensive Guide to Pathogenesis, Diagnosis, and Management” by Eberhard Nieschlag, Hermann M. Behre, and Susan Nieschlag
- This book provides detailed insights into male infertility, with extensive discussions on the role of the vas deferens.
- “Andrology: Male Reproductive Health and Dysfunction” by Eberhard Nieschlag and Hermann M. Behre
- A comprehensive textbook focusing on male reproductive health, including chapters on the vas deferens and associated conditions.
Academic Journals
- Journal of Andrology
- A peer-reviewed journal publishing original research and reviews on male reproductive health, including studies on the vas deferens.
- Human Reproduction
- This leading journal covers advanced research in reproductive biology, including innovative treatments and diagnostic methods for vas deferens disorders.
Mobile Apps and Online Tools
- MyFertilityMD
- An app designed to help men track their reproductive health, including fertility and lifestyle factors affecting the vas deferens.
- Men’s Health App
- Offers a wide range of resources on male health, including information on reproductive function and preventive strategies.
- Fertility Tracker
- A comprehensive app for monitoring fertility parameters, including semen analysis results and lifestyle influences on reproductive health.
Frequently Asked Questions
What is the primary function of the vas deferens?
The vas deferens transports mature sperm from the epididymis to the ejaculatory ducts and plays a critical role in mixing sperm with seminal fluid during ejaculation, which is essential for male fertility.
How does a vasectomy work?
A vasectomy is a surgical procedure in which a segment of the vas deferens is cut or sealed to prevent sperm from reaching the ejaculatory ducts, thereby providing a permanent method of contraception.
What causes congenital absence of the vas deferens?
Congenital absence of the vas deferens (CBAVD) is often associated with mutations in the CFTR gene, commonly seen in men with cystic fibrosis, resulting in infertility despite normal sperm production.
How are obstructions in the vas deferens diagnosed?
Obstructions are typically diagnosed through semen analysis, imaging studies such as scrotal ultrasound and vasography, and sometimes genetic testing to rule out congenital causes.
What treatment options exist for vas deferens obstructions?
Treatment options for obstructions include surgical reconstruction procedures such as vasovasostomy or vasoepididymostomy, along with assisted reproductive technologies like ICSI when reconstruction is not feasible.
Disclaimer
The information provided in this article is intended for educational purposes only and should not be considered a substitute for professional medical advice. Always consult a qualified healthcare provider for personalized recommendations and treatment options.
Please share this article on Facebook, X (formerly Twitter), or your preferred platform to help spread awareness about vas deferens health and promote informed reproductive care.