The vestibular system is essential for maintaining balance, spatial orientation, and overall coordination. Located deep within the inner ear, this complex network of structures continuously sends information about head position and motion to the brain, enabling us to keep our balance, stabilize our gaze, and perform coordinated movements. Whether you’re walking, running, or simply standing still, the vestibular system plays a critical role in helping you navigate the world. This guide provides an in-depth look at the anatomy, functions, common disorders, diagnostic methods, treatment options, and lifestyle tips to help you maintain optimal vestibular health.
Table of Contents
- Anatomical Insights
- Functional Dynamics
- Common Disorders
- Diagnostic Approaches
- Treatment Strategies
- Supplemental & Nutritional Support
- Lifestyle & Preventive Measures
- Trusted Resources
- Frequently Asked Questions
Anatomical Insights
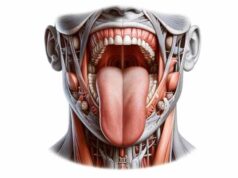
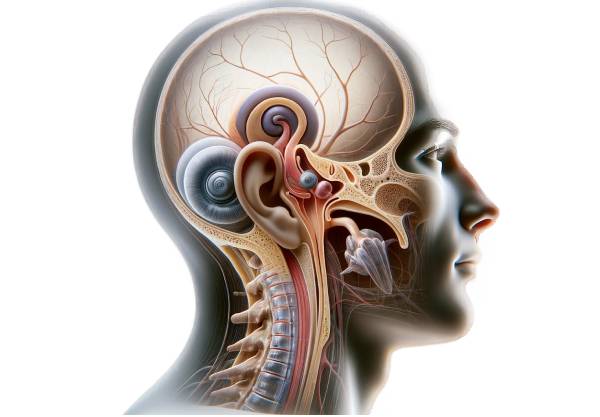
The vestibular system is housed within the inner ear, an intricate structure composed of both bony and membranous labyrinths that protect its delicate sensory components. The outer bony labyrinth forms a rigid protective casing within the temporal bone, filled with a fluid called perilymph. Inside, the membranous labyrinth is suspended and filled with endolymph, creating an environment where sensory organs can detect head movements with precision.
Bone and Membranous Labyrinth
- Bony Labyrinth:
This rigid, bony structure encases the entire vestibular apparatus. It provides critical protection against mechanical trauma and houses the labyrinthine fluids. Its intricate design is essential for safeguarding the sensory components inside. - Membranous Labyrinth:
Suspended within the bony labyrinth, the membranous labyrinth consists of a network of fluid-filled sacs and ducts that include the semicircular canals, utricle, and saccule. This delicate structure is responsible for converting mechanical movements into neural signals.
Semicircular Canals
Three semicircular canals—anterior (superior), posterior, and lateral (horizontal)—are oriented in orthogonal planes. Each canal has a widened region called the ampulla, which contains the crista ampullaris. The hair cells in the crista detect rotational movements:
- Anterior Canal: Detects nodding motions.
- Posterior Canal: Senses tilting of the head toward the shoulders.
- Lateral Canal: Monitors horizontal head movements.
Otolithic Organs
The utricle and saccule, known as the otolithic organs, are specialized for detecting linear accelerations and the effects of gravity:
- Utricle:
Positioned horizontally, it primarily detects horizontal movements and head tilts. - Saccule:
Oriented vertically, it senses vertical accelerations such as those experienced during jumping or sudden drops.
Both organs contain the macula, a sensory epithelium covered by the otolithic membrane embedded with calcium carbonate crystals (otoconia) that enhance sensitivity to gravitational forces.
Sensory Receptors
- Hair Cells:
These specialized cells have hair-like projections (stereocilia) and a single kinocilium. Their deflection due to fluid movement initiates nerve impulses, conveying critical balance and spatial orientation data to the brain.
Nerve Pathways and Central Integration
- Vestibular Nerve:
A branch of the vestibulocochlear nerve (cranial nerve VIII), it carries signals from the hair cells to the brainstem. - Vestibular Nuclei:
Located in the brainstem, these nuclei integrate vestibular input with visual and proprioceptive signals. - Central Connections:
Processed signals are sent to the cerebellum, spinal cord, and ocular motor nuclei, ensuring coordinated body movements, posture adjustments, and stable vision.
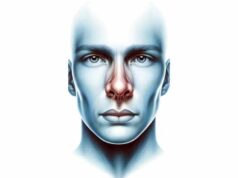
Vascular Supply
The vestibular system is supplied by the labyrinthine artery, a branch of the anterior inferior cerebellar artery (AICA). This artery divides into:
- Anterior Vestibular Artery: Supplies the utricle, part of the saccule, and portions of the semicircular canals.
- Posterior Vestibular Artery: Delivers blood to the remaining parts of the saccule and semicircular canals.
Supporting Systems
The vestibular system works in concert with other systems:
- Proprioceptive System:
Sensors in muscles and joints complement vestibular input for a comprehensive understanding of body position. - Visual System:
Provides external cues that, together with vestibular data, maintain balance and spatial orientation. - Cerebellum:
Integrates all sensory inputs to coordinate smooth, balanced movements.
Clinical Relevance
A robust grasp of vestibular anatomy is essential for diagnosing disorders such as benign paroxysmal positional vertigo (BPPV), Meniere’s disease, and vestibular neuritis. Detailed anatomical knowledge aids in targeting treatments and managing symptoms that disrupt balance and spatial orientation.
Functional Dynamics
The vestibular system’s primary role is to provide the brain with information about head position, motion, and spatial orientation. This sensory input is critical for balance, coordination, and the stabilization of vision during movement.
Balance and Equilibrium
- Detection of Rotational Movements:
The semicircular canals sense rotational movements by detecting changes in the inertia of the endolymph fluid. When the head rotates, the fluid lags, bending the cupula within the ampulla and stimulating hair cells. - Sensing Linear Movements and Gravity:
The utricle and saccule detect linear accelerations and head tilts. The displacement of the otolithic membrane over the macula’s hair cells provides precise information about the head’s orientation relative to gravity.
Vestibulo-Ocular Reflex (VOR)
The VOR is a key mechanism that stabilizes vision during head movements:
- Mechanism:
When the head moves, the vestibular system triggers compensatory eye movements via the ocular motor nuclei. This reflex ensures that the eyes remain fixed on a target, allowing for clear vision during rapid movements. - Importance:
VOR is vital for activities like walking or running, where constant head movement could otherwise result in blurred vision.
Postural Control and Motor Coordination
- Vestibulo-Spinal Reflex (VSR):
The vestibular system communicates with the spinal cord to adjust muscle tone, ensuring that posture is maintained despite shifts in head position. - Integration with the Cerebellum:
The cerebellum processes vestibular input alongside other sensory information to fine-tune motor responses and maintain overall balance.
Sensory Integration
- Multimodal Integration:
The vestibular system works in tandem with visual and proprioceptive inputs. The brain synthesizes these signals to form a cohesive perception of body orientation and movement. - Adaptive Compensation:
When vestibular function is compromised, the brain can increase reliance on visual and proprioceptive cues to maintain balance—a process known as central compensation.
Hormonal and Neural Modulation
- Neural Regulation:
The vestibular nuclei modulate signals through complex neural pathways, influencing both motor and autonomic responses. - Role of Neurotransmitters:
Neurotransmitters such as glutamate and GABA play roles in modulating vestibular signal transmission, affecting both excitatory and inhibitory pathways that shape balance and motion perception.
Common Vestibular Disorders
Vestibular disorders can severely impact balance, coordination, and quality of life. Understanding these conditions helps in early detection and appropriate treatment.
Benign Paroxysmal Positional Vertigo (BPPV)
BPPV is a common vestibular disorder caused by dislodged otoconia entering one of the semicircular canals, most often the posterior canal.
- Pathophysiology:
Dislodged calcium carbonate crystals disturb the normal flow of endolymph, triggering inappropriate stimulation of the hair cells in the crista ampullaris. - Symptoms:
Sudden, brief episodes of vertigo triggered by changes in head position; accompanying symptoms can include nausea and nystagmus. - Treatment:
Canalith repositioning maneuvers, such as the Epley and Semont maneuvers, are highly effective in relocating the crystals back to the utricle.
Meniere’s Disease
Meniere’s disease is a chronic condition characterized by episodic vertigo, fluctuating hearing loss, tinnitus, and a sensation of fullness in the affected ear.
- Etiology:
Abnormal fluid buildup (endolymphatic hydrops) in the inner ear is thought to be the primary cause. - Symptoms:
Vertigo episodes lasting 20 minutes to several hours, progressive hearing loss, tinnitus, and a feeling of pressure or fullness in the ear. - Management:
Dietary modifications (low-sodium diet), diuretics, vestibular suppressants, and, in severe cases, surgical interventions such as endolymphatic sac decompression are used.
Vestibular Neuritis
Vestibular neuritis is an inflammation of the vestibular nerve, often resulting from a viral infection, causing acute vertigo.
- Presentation:
Sudden onset of severe vertigo, nausea, and imbalance, usually without hearing loss. - Treatment:
Corticosteroids to reduce inflammation and vestibular rehabilitation therapy (VRT) to promote central compensation.
Labyrinthitis
Labyrinthitis involves inflammation of both the vestibular nerve and the labyrinth, often resulting from infections.
- Symptoms:
Severe vertigo, hearing loss, tinnitus, and sometimes ear pain. - Management:
Similar to vestibular neuritis, treatment includes corticosteroids, antiviral or antibiotic medications (if infection is present), and VRT.
Vestibular Migraine
Vestibular migraine is a subtype of migraine where vertigo is a predominant symptom, sometimes without the classic headache.
- Symptoms:
Episodes of vertigo lasting minutes to hours, often accompanied by sensitivity to light and sound, and visual disturbances. - Management:
Avoidance of migraine triggers, prophylactic medications (beta-blockers, antiepileptics), and acute treatments (triptans). Vestibular rehabilitation may also be beneficial.
Superior Canal Dehiscence Syndrome (SCDS)
SCDS is a rare condition in which a thinning or absence of the bony covering of the superior semicircular canal leads to abnormal stimulation.
- Symptoms:
Vertigo triggered by loud sounds or pressure changes, autophony (abnormally loud perception of one’s own voice), and imbalance. - Treatment:
Surgical repair via a middle fossa craniotomy or transmastoid approach is typically required to plug the dehiscent canal.
Bilateral Vestibulopathy
Bilateral vestibulopathy is characterized by the loss of vestibular function in both ears, leading to chronic imbalance.
- Etiology:
Ototoxic medications, bilateral Meniere’s disease, or idiopathic causes. - Symptoms:
Chronic imbalance, difficulty walking in low-light conditions, and oscillopsia during head movements. - Management:
Primarily relies on vestibular rehabilitation therapy to enhance visual and proprioceptive compensation, along with assistive devices if needed.
Diagnostic Approaches
Effective diagnosis of vestibular disorders requires a multifaceted approach, combining clinical examination, specialized vestibular tests, imaging studies, and functional assessments to determine the underlying cause.
Clinical Evaluation
- Patient History:
Detailed history-taking includes the onset, duration, frequency, and triggers of vertigo or dizziness, as well as associated symptoms like hearing loss, tinnitus, and headache. - Physical Examination:
A thorough examination assesses balance, coordination, and gait. Specific tests such as the Romberg test, head thrust test, and Dix-Hallpike maneuver are used to detect vestibular abnormalities.
Vestibular Function Testing
- Electronystagmography (ENG) and Videonystagmography (VNG):
These tests record involuntary eye movements (nystagmus) in response to vestibular stimulation. Caloric testing (using warm and cold stimuli) and positional tests help localize dysfunction. - Rotational Chair Testing:
The patient is seated in a rotating chair while eye movements are monitored. This test provides an overall assessment of the vestibular system’s responsiveness, especially in bilateral vestibulopathy. - Vestibular Evoked Myogenic Potentials (VEMPs):
VEMPs measure the reflexive muscle responses (in the neck or eyes) to sound stimulation, assessing the function of the saccule and utricle. Both cervical (cVEMP) and ocular (oVEMP) tests are used.
Imaging Studies
- Magnetic Resonance Imaging (MRI):
High-resolution MRI scans provide detailed images of the inner ear, helping to diagnose vestibular neuritis, labyrinthitis, and tumors such as acoustic neuromas. - Computed Tomography (CT) Scans:
CT imaging is especially useful for evaluating the bony structures of the inner ear, making it invaluable in diagnosing superior canal dehiscence syndrome and other osseous abnormalities.
Audiometric and Vestibular-Audiometric Tests
- Pure Tone Audiometry:
Assesses hearing thresholds to identify sensorineural or conductive hearing loss associated with vestibular disorders. - Speech Audiometry:
Evaluates speech recognition ability, providing additional context to hearing impairment. - Tympanometry:
Assesses middle ear function, which can influence vestibular function in certain cases.
Posturography
- Computerized Dynamic Posturography (CDP):
Measures a patient’s ability to maintain balance on a moving platform under various conditions, integrating vestibular, visual, and proprioceptive inputs. - Static and Dynamic Balance Tests:
These tests evaluate balance control and help pinpoint deficiencies in vestibular function.
Laboratory and Genetic Tests
- Blood Tests:
Basic blood tests, including complete blood count (CBC) and inflammatory markers (e.g., C-reactive protein), can indicate systemic infection or inflammation. - Genetic Testing:
In cases of suspected hereditary vestibular disorders, genetic tests may be performed to identify mutations that affect vestibular function.
Advanced Diagnostic Modalities
- Optical Coherence Tomography (OCT):
An emerging imaging modality that offers high-resolution cross-sectional images of vestibular structures, potentially identifying early pathological changes. - Fluorescence Spectroscopy:
This technique evaluates biochemical changes in inner ear tissues, aiding in the early detection of precancerous or degenerative changes.
By combining these diagnostic tools, clinicians can accurately pinpoint the underlying causes of vestibular disorders and tailor treatments to individual needs.
Treatment Strategies
The management of vestibular disorders is multifaceted and depends on the specific diagnosis, severity of symptoms, and patient needs. Treatments range from conservative management and physical therapy to minimally invasive procedures and advanced surgical interventions.
Medical Management
- Vestibular Suppressants:
Medications such as meclizine, dimenhydrinate, and diazepam help reduce the intensity of vertigo and associated nausea by damping vestibular system activity. - Diuretics:
In Meniere’s disease, diuretics are used to reduce endolymphatic fluid buildup, alleviating vertigo and pressure. - Corticosteroids:
Used in vestibular neuritis and labyrinthitis, corticosteroids reduce inflammation and speed recovery. - Antibiotics/Antivirals:
When infections are implicated, targeted antibiotics or antiviral medications are prescribed to address the underlying cause.
Vestibular Rehabilitation Therapy (VRT)
- Customized Exercise Programs:
VRT consists of specific exercises aimed at promoting central compensation, improving balance, and reducing dizziness. These may include gaze stabilization, balance training, and habituation exercises. - Multisensory Integration:
Rehabilitation strategies encourage the integration of visual, proprioceptive, and vestibular inputs, enhancing overall stability.
Canalith Repositioning Procedures
- Epley Maneuver:
This series of head and body movements repositions dislodged otoconia in the semicircular canals, particularly effective for treating BPPV. - Semont Maneuver:
An alternative repositioning maneuver that can also help alleviate BPPV symptoms. - Brandt-Daroff Exercises:
Home-based exercises that facilitate the gradual repositioning of otoconia, useful for patients with recurrent BPPV.
Surgical Interventions
- Endolymphatic Sac Surgery:
Used in Meniere’s disease, this surgery reduces endolymphatic pressure by decompressing the endolymphatic sac. - Vestibular Nerve Section:
In severe cases of intractable vertigo (often associated with Meniere’s disease), cutting the vestibular nerve can alleviate symptoms while preserving hearing. - Labyrinthectomy:
A radical option where the vestibular apparatus is removed, generally reserved for cases where hearing is already lost.
Innovative and Complementary Treatments
- Ototoxic Gentamicin Therapy:
Low-dose gentamicin injections can selectively ablate vestibular hair cells in Meniere’s disease, reducing vertigo episodes. - Botulinum Toxin Injections:
Emerging evidence suggests Botox may help manage vestibular migraines and reduce abnormal neural firing. - Virtual Reality (VR) Therapy:
VR-based rehabilitation offers immersive, controlled environments to help patients adapt to vestibular deficits and improve balance. - Acupuncture and Chiropractic Care:
Complementary therapies such as acupuncture and certain chiropractic techniques may offer symptom relief for some patients by modulating neural pathways and reducing muscle tension.
Psychological Support
- Cognitive Behavioral Therapy (CBT):
CBT can help manage the anxiety and stress often associated with chronic vestibular disorders, improving overall quality of life. - Support Groups:
Connecting with others facing similar challenges can provide emotional support and practical advice.
By employing a combination of these treatment strategies, healthcare providers can effectively manage vestibular disorders, reduce symptoms, and help patients regain balance and spatial orientation.
Supplemental & Nutritional Support
Certain nutritional supplements have shown promise in supporting vestibular health by reducing inflammation, improving nerve function, and enhancing overall inner ear health.
Recommended Supplements
- Ginkgo Biloba:
Known to improve cerebral and inner ear blood flow, ginkgo biloba helps alleviate symptoms of vertigo and tinnitus by reducing oxidative stress and enhancing neural function. - Magnesium:
Magnesium’s muscle-relaxing and neuroprotective properties can reduce migraine frequency and severity, including vestibular migraines. - Vitamin D:
Essential for calcium regulation and inner ear health, adequate vitamin D levels are associated with a reduced risk of BPPV and other vestibular disorders. - Vitamin B12:
Critical for nerve health, vitamin B12 supplementation may alleviate vertigo and balance issues, particularly in individuals with a deficiency. - Coenzyme Q10 (CoQ10):
CoQ10 supports cellular energy production and acts as an antioxidant, potentially reducing the frequency of vestibular migraines. - Omega-3 Fatty Acids:
With strong anti-inflammatory effects, omega-3 fatty acids found in fish oil help improve neural function and reduce inflammation in the vestibular system. - Zinc:
Zinc supports immune function and tissue repair, and deficiencies have been linked to inner ear disorders such as tinnitus. - Melatonin:
Melatonin can help regulate sleep cycles disrupted by vestibular disorders and has antioxidant properties that may protect inner ear structures. - Ginger:
Well-known for its anti-nausea properties, ginger can help alleviate vertigo-related nausea and improve gastrointestinal motility.
Integrating Supplements into Your Routine
Consult with a healthcare provider before starting any supplement regimen. When integrated with a balanced diet rich in fruits, vegetables, lean proteins, and whole grains, these supplements can serve as a valuable adjunct to conventional treatments and support overall vestibular function.
Lifestyle & Preventive Measures
Adopting healthy lifestyle habits is essential for maintaining vestibular function and preventing balance disorders. The following strategies focus on reducing risk factors and promoting overall inner ear and neural health.
Daily Lifestyle Practices
- Stay Hydrated:
Adequate fluid intake supports proper inner ear fluid dynamics and overall cellular function. - Balanced Diet:
Consuming a nutrient-rich diet helps maintain hormonal balance, reduces inflammation, and supports neural health. Include plenty of fruits, vegetables, whole grains, and lean proteins. - Regular Exercise:
Activities such as walking, yoga, tai chi, and swimming improve balance, coordination, and cardiovascular health, which are essential for optimal vestibular function. - Stress Management:
Chronic stress can exacerbate vestibular symptoms. Engage in mindfulness, meditation, and deep breathing exercises to lower stress levels. - Sleep Hygiene:
Adequate, quality sleep supports overall brain function and aids in the recovery and maintenance of vestibular pathways. - Avoid Rapid Head Movements:
Gradual movements can prevent triggering vertigo or dizziness, especially in individuals with vestibular dysfunction. - Protect Your Ears:
Use ear protection in noisy environments to prevent potential damage to inner ear structures. - Monitor Medications:
Be aware of ototoxic medications that may impair vestibular function and discuss alternatives with your healthcare provider if necessary. - Regular Check-Ups:
Routine examinations by a healthcare provider help detect vestibular issues early, allowing for prompt intervention. - Healthy Environment:
Avoid exposure to environmental toxins and pollutants that may negatively impact neural and vascular health.
Implementing these lifestyle and preventive measures can significantly enhance vestibular function and reduce the risk of balance-related issues.
Trusted Resources
Staying informed and accessing reliable information is crucial for managing vestibular health. Below are some authoritative resources to guide further reading and clinical practice.
Books
- “Balance: A Dizzying Journey Through the Science of Our Most Delicate Sense” by Carol Svec
Explores the science behind balance and the vestibular system, offering insights into disorders and treatment strategies. - “The Vestibular System: A Sixth Sense” by Charles C. Della Santina and Andrew C. Goldberg
A comprehensive resource covering the anatomy, physiology, and clinical aspects of the vestibular system. - “Overcoming Meniere’s Disease: A Practical Guide” by Spencer Payne
Provides practical advice and treatment options for managing Meniere’s disease and improving quality of life.
Academic Journals
- Journal of Vestibular Research
This peer-reviewed journal publishes original research, reviews, and clinical studies on vestibular disorders and advances in diagnostic and therapeutic approaches. - Otolaryngology–Head and Neck Surgery
A leading journal that includes research on vestibular conditions, treatment modalities, and innovative diagnostic techniques.
Mobile Apps and Online Tools
- Vestibular First:
An app offering educational resources, diagnostic tools, and treatment guidelines specifically for vestibular disorders. - DizzyFix:
Provides guided canalith repositioning maneuvers, enabling patients with BPPV to perform home treatments under professional guidance. - Balancia:
Offers balance training exercises and tracks progress, helping users improve stability and reduce dizziness.
Frequently Asked Questions
What is the primary function of the vestibular system?
The vestibular system provides essential sensory information about head position and movement, enabling balance, spatial orientation, and the stabilization of vision during motion.
How does the vestibulo-ocular reflex (VOR) work?
The VOR stabilizes vision during head movements by triggering compensatory eye movements. When the head moves, the vestibular system sends signals to the ocular motor nuclei, which adjust eye position to maintain a steady gaze.
What causes benign paroxysmal positional vertigo (BPPV)?
BPPV is caused by dislodged otoconia from the utricle that migrate into a semicircular canal, disrupting normal fluid dynamics and triggering vertigo with head movements.
How is Meniere’s disease managed?
Meniere’s disease is managed with dietary modifications, diuretics, vestibular suppressants, and in severe cases, surgical interventions such as endolymphatic sac decompression to reduce inner ear fluid buildup.
What treatments are available for vestibular neuritis?
Vestibular neuritis is treated with corticosteroids to reduce inflammation, along with vestibular rehabilitation therapy (VRT) to promote central compensation and restore balance.
Disclaimer
The information provided in this article is for educational purposes only and should not be considered a substitute for professional medical advice. Always consult a qualified healthcare provider for personalized guidance and treatment options.
Please share this article on Facebook, X (formerly Twitter), or your preferred platform to help promote awareness about vestibular health and encourage proactive balance care.