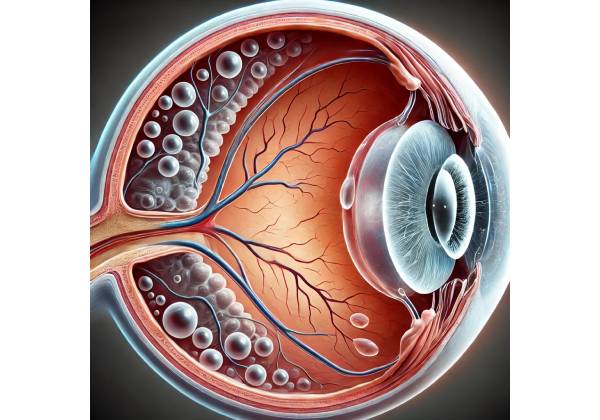
Vitreomacular adhesion (VMA) is an ocular condition characterized by an abnormal attachment between the vitreous humor and the macula, the central part of the retina responsible for fine detail perception. Understanding VMA requires a closer look at the eye’s anatomy, particularly the vitreous body and its relationship to the retina.
Anatomy of Vitreous and Retina
The vitreous humor is a clear, gel-like substance that fills the space between the eye’s lens and its retina. It maintains the eye’s spherical shape and allows light to reach the retina. The retina is a thin layer of light-sensitive tissue in the back of the eye that converts light into neural signals that travel to the brain via the optic nerve.
The macula is a small but important area of the retina that controls central vision, visual acuity, and color perception. Any condition affecting the macula can impair a person’s ability to perform tasks that require fine detail, such as reading, driving, and recognizing faces.
The Procedure for Vitreous Detachment
As people age, the vitreous humor naturally degenerates, a process known as vitreous syneresis. This procedure involves the liquefaction of the vitreous gel, causing it to shrink and eventually pull away from the retina. The event is known as posterior vitreous detachment (PVD). PVD is a common age-related change that rarely causes significant vision problems.
However, in some cases, the vitreous remains partially attached to the macula while other parts have separated from the retina. This partial attachment is known as vitreomacular adhesion (VMA). When VMA occurs, the vitreous continues to exert traction on the macula, which can cause a variety of visual disturbances and, if left untreated, more serious complications.
Symptoms Of Vitreomacular Adhesion
Vitreomacular adhesion can be asymptomatic in the early stages, which means that some people may not notice any symptoms. However, as the condition progresses, the vitreous’s ongoing traction on the macula can cause a variety of visual disturbances. Common symptoms of VMA are:
1. Distorted vision (metamorphopsia):
Patients with VMA frequently report that straight lines appear wavy or distorted. This phenomenon, known as metamorphopsia, is a hallmark symptom of macular involvement and results from abnormal pulling on the macula, disrupting its normal architecture.
2. Blurred vision:
As VMA progresses, people may notice a gradual blurring of their central vision. This can have an impact on activities that require sharp vision, such as reading, facial recognition, and driving.
3. Reduced Visual Acuity:
Over time, persistent traction on the macula can cause a decrease in visual acuity, making it difficult to see fine details. This loss of sharpness can cause problems with daily tasks and lower overall quality of life.
4. Macular Hole Formation:
Continuous pulling on the macula can occasionally result in the formation of a macular hole. A macular hole is a full-thickness defect in the macula that causes significant loss of central vision. The formation of a macular hole is one of the more serious complications of untreated VMA.
5. Increased floaters:
While floaters (small specks or strands that drift across the field of vision) are common in people with PVD, they can also be a sign of VMA. These floaters form when the vitreous gel separates from the retina, and they may be more visible if the vitreous remains partially attached to the macula.
Causes and Risk Factors for Vitreomacular Adhesion
Vitreomacular adhesion is primarily an age-related condition, with the risk rising as people get older. As previously stated, degeneration and liquefaction of the vitreous humor are natural processes that occur with age. However, several factors can influence the incomplete detachment of the vitreous from the retina, resulting in VMA:
1. Age:
Age is the most important risk factor for the development of VMA. The likelihood of developing PVD and, eventually, VMA increases with age, particularly in people over the age of 50.
2. Gender:
Some studies suggest that women may have a slightly higher risk of developing VMA than men. This difference could be due to hormonal changes that affect the vitreous and retina.
3. Myopia (nearsightedness):
Individuals with high myopia have a higher risk of developing VMA. The elongated shape of the myopic eye can cause changes in the vitreous and retina, predisposing them to vitreomacular adhesions.
4. Previous eye surgery:
People who have had cataract surgery or other intraocular procedures may be more likely to develop VMA. Surgical manipulation of the eye can hasten vitreous degeneration and raise the risk of incomplete vitreous detachment.
5. Diabetes:
Diabetic retinopathy, a diabetes complication that affects the retina, can also raise the risk of VMA. The abnormal blood vessels and scar tissue associated with diabetic retinopathy can cause vitreous traction on the macula.
Complications of Vitreomacular Adhesion
While VMA can cause significant visual symptoms, it can also lead to more serious complications if not treated properly. The complications include:
**1. Vitreomacular Traction Syndrome (VMTS): **
VMT occurs when the vitreous exerts sufficient traction on the macula to cause structural changes in the retina. This can cause macular edema (macula swelling) and further vision distortion. VMT is a more advanced form of VMA and may necessitate surgical intervention.
2. Macular Holes:
As previously stated, a macular hole is a serious complication of VMA. Continuous pulling on the macula can eventually lead to a tear, resulting in a full-thickness hole. A macular hole causes significant loss of central vision and usually requires surgical repair.
**3. The epiretinal membrane (ERM)
In some cases, prolonged traction on the macula can cause the formation of an epiretinal membrane, also known as a macular pucker. This thin layer of scar tissue forms on the surface of the retina, distorting vision and lowering visual acuity.
4. Retinal detachment:
Although less common, severe VMA can result in retinal detachment. This happens when the vitreous gel pulls away from the retina with enough force to separate it from the surrounding tissue. Retinal detachment is a medical emergency that requires immediate surgical intervention to avoid permanent vision loss.
Effects on Quality of Life
Vitreomacular adhesion can have a significant impact on a person’s quality of life, especially as the disease progresses and symptoms worsen. Visual disturbances caused by VMA, such as distorted vision and decreased visual acuity, can make it difficult to perform daily tasks that require clear vision. Activities like reading, driving, and using digital devices can become increasingly difficult, resulting in frustration and a loss of independence.
In addition to the practical challenges, VMA has a significant psychological impact. The fear of losing vision, as well as the uncertainty about the condition’s progression, can cause anxiety and depression. Individuals with VMA may also feel isolated or self-conscious about their visual impairments, especially if they are unable to participate in social activities or hobbies that they previously enjoyed.
Given the risk of significant visual impairment, individuals with VMA should seek regular eye examinations and appropriate treatment to manage the condition and avoid complications.
Diagnostic methods
Vitreomacular adhesion is diagnosed using a combination of clinical evaluation, imaging techniques, and a thorough assessment of the patient’s symptoms. The goal is to detect the presence of VMA, assess the amount of vitreous traction on the macula, and determine the best course of action. Several diagnostic methods are frequently used to assess VMA:
1. Clinical Examination
The first step in diagnosing VMA is a comprehensive clinical examination by an eye care professional. This usually includes:
- Visual Acuity Testing: To determine visual acuity and identify any reductions.
- Slit-Lamp Biomicroscopy: A slit-lamp examination enables the clinician to see the anterior segment of the eye in great detail. However, a special attachment known as a fundus lens or a contact lens can be used to examine the vitreous and retina, particularly the macula.
2. Optical Coherence Tomography (OCT
Optical coherence tomography (OCT) is a non-invasive imaging technique that has become the gold standard for detecting vitreomacular adhesions. OCT produces high-resolution cross-sectional images of the retina and vitreous, allowing clinicians to see the precise location and size of the adhesion. OCT can detect even subtle changes in the macula’s structure and is extremely useful in detecting VMA, VMT, and other related conditions.
3. B-scan ultrasonography
B-scan ultrasonography may be used in cases where OCT is insufficient, particularly if there is media opacity (e.g., cataracts) that obscures the view of the retina. This ultrasound technique generates images of the vitreous and retina, allowing you to determine the presence and extent of vitreomacular adhesion.
4. Fundus Photography
Fundus photography is another tool for documenting the appearance of the retina and macula. While not as detailed as OCT, fundus photography can reveal important information about the retina’s overall appearance, as well as any signs of traction or abnormal changes caused by vitreomacular adhesion. It is frequently used in conjunction with other diagnostic tests to provide a comprehensive assessment of the retina’s condition.
5. Fluorescein angiography
Fluorescein angiography is a diagnostic procedure that involves injecting a fluorescent dye into the bloodstream and photographing the dye as it travels through the blood vessels in the retina. This test is especially useful for detecting abnormal retinal blood vessels and assessing any leakage or swelling in the macula. While fluorescein angiography is not the primary method for diagnosing VMA, it can help rule out other conditions, such as macular edema, that may be associated with VMA or complicate its treatment.
6. Indocyanine green angiography (ICG)
Indocyanine Green Angiography (ICG) is another imaging technique for assessing choroidal circulation beneath the retina. Although ICG is not commonly used to diagnose VMA, it may be used to evaluate the deeper layers of the retina and choroid, especially if there are other concerns, such as choroidal neovascularization.
7. Amsler Grid Test
The Amsler Grid is a simple yet effective tool for assessing the central visual field. Patients must concentrate on a central dot within a grid of horizontal and vertical lines. If the patient perceives any lines as wavy, distorted, or missing, this could indicate macular involvement, which is consistent with conditions such as VMA. The Amsler Grid test is especially useful for patients to monitor their vision at home and detect changes that may indicate worsening VMA or progression to more serious complications such as a macular hole.
8. Patient History and Symptom Assessment
A thorough examination of the patient’s medical history and symptoms is critical to the diagnostic process. Understanding the onset, duration, and progression of symptoms like blurred vision, metamorphopsia, and floaters can help diagnose VMA. A detailed history can also help distinguish VMA from other macular conditions and guide the selection of additional diagnostic tests.
Vitreomacular Adhesion Management
Managing vitreomacular adhesion (VMA) requires a variety of approaches, depending on the severity of the condition, the presence of symptoms, and the risk of complications like macular hole formation or significant vision loss. Management strategies vary from observation and monitoring to medical and surgical interventions.
1. Observation and Monitoring
In cases where VMA is mild and does not cause significant symptoms, a cautious approach of observation may be recommended. Because some cases of VMA resolve spontaneously as the vitreous separates from the macula, regular monitoring with follow-up eye exams and Optical Coherence Tomography (OCT) imaging may be adequate. During these follow-up visits, the eye care provider will determine whether the adhesion has progressed, resolved, or resulted in complications like vitreomacular traction (VMT) or a macular hole.
Patients under observation are usually advised to closely monitor their vision at home, often using tools such as the Amsler Grid, and to report any changes in their vision right away. If symptoms worsen or there is evidence of progression on OCT, more active treatment may be required.
2. Pharmaceutical Treatment
Pharmacological intervention is an option for patients with symptomatic VMA, especially if they are at risk of developing more serious conditions such as VMT or macular holes. One of the primary pharmacological treatments for VMA is the use of ocriplasmin (Jetrea), a recombinant protease enzyme that degrades the proteins that cause the vitreous to adhere to the macula.
Ocriplasmin Injection:
Ocriplasmin is injected directly into the vitreous cavity. The enzyme dissolves the proteins that are responsible for the adhesion between the vitreous and the macula. This treatment is especially effective in patients with early-stage VMA or those with minimal vitreous traction. Studies have shown that ocriplasmin can cause vitreomacular separation in a significant percentage of patients, potentially avoiding surgery.
However, ocriplasmin is not appropriate for all patients and may cause side effects such as temporary vision changes, eye pain, and inflammation. The decision to use ocriplasmin should be based on a thorough discussion between the patient and their eye care provider, taking into account the potential benefits and risks.
3. Surgical Intervention
Patients with advanced VMA, particularly those who develop VMT or a macular hole, may require surgery to relieve traction on the macula and prevent further damage. The most common surgical procedure for VMA is vitrectomy.
Vitrectomy:
Vitrectomy is a surgical procedure that removes vitreous gel from the eye and relieves traction on the macula. During the procedure, the surgeon may also remove any epiretinal membrane that has developed on the macula. This helps to flatten the macula, resulting in better visual outcomes. In cases of a macular hole, the surgeon may take additional steps, such as filling the eye with a gas bubble, to encourage hole closure and healing.
Vitrectomy is typically considered when VMA causes significant symptoms, such as vision distortion or decreased visual acuity, or when there is a risk of progression to a macular hole. While vitrectomy is extremely effective at treating VMA and improving vision, it is not without risks. Possible complications include cataract formation, retinal detachment, infection, and intraocular bleeding. The risks and benefits of any surgical procedure, as with any other, should be carefully considered, and patients should be well-informed about the expected outcomes and potential side effects.
4. Lifestyle Changes and Supportive Care
In addition to medical and surgical treatments, lifestyle changes and supportive care can help manage VMA. Patients with VMA could benefit from the following approaches:
- Visual Aids: For those who have vision distortion or decreased acuity, using visual aids like magnifiers or enhanced lighting can help with daily tasks like reading and using digital devices.
- Nutrition and Eye Health: Consuming antioxidant-rich foods like leafy greens, berries, and fish may improve overall eye health. While there is no direct evidence linking diet to the resolution of VMA, maintaining a healthy nutritional status is beneficial to eye health.
- Regular Eye Exams: Ongoing follow-up with an eye care provider is required to monitor the progression of VMA and adjust treatment plans as needed. Early detection of complications can result in timely intervention and better visual outcomes.
Overall, VMA management is individualized based on the patient’s condition, symptoms, and risks. Eye care professionals can effectively manage VMA by combining observation, pharmacological treatments, surgical options, and supportive care to help patients keep their vision and quality of life.
Trusted Resources and Support
Books
- “Retinal and Vitreous Surgery” by Steve Charles, MD
This book offers a comprehensive overview of surgical techniques and management strategies for retinal and vitreous conditions, including vitreomacular adhesion. - “The Retina Illustrated” by Justis P. Ehlers, MD, and Chirag P. Shah, MD
This textbook provides detailed illustrations and explanations of various retinal conditions, including VMA, making it a valuable resource for both patients and professionals.
Organizations
- American Academy of Ophthalmology (AAO)
The AAO provides extensive resources for patients and healthcare professionals, including information on the latest research and treatment options for vitreomacular adhesion. - The Retina Society
An organization dedicated to advancing knowledge and research in retinal diseases. Their website offers educational materials and updates on the latest advancements in the treatment of conditions like VMA.










